Abstract
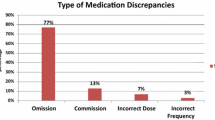
Background Medication errors are one of the main causes of morbidity amongst hospital inpatients. More than half of medication errors occur at ‘interfaces of care’, when patients are discharged or transferred to the care of another physician. Medication reconciliation is the process of reviewing patients’ complete previous medication regimen, comparing it with current prescriptions, and analysing and resolving any discrepancies that the pharmacist does not believe to be intentional (unjustified discrepancies). Objective To quantify and analyse reconciliation unjustified discrepancies detected by a pharmacist in patients admitted to an internal medicine unit (IMU) over a 3-year period. Setting and method The hospital employs a pharmacist who acts as a link between the primary care services and the internal medicine specialist care unit. A retrospective descriptive study on the reconciliation discrepancies found was carried out. Medication reconciliation was performed upon admission in all patients transferred from the Accident and Emergency department (A&E) and admitted to the IMU, and also at the time of discharge. The interventions were categorised based on the consensus document on terminology and medication classification published by the Spanish Society of Hospital Pharmacy. Main outcome measure Number of patients with unjustified discrepancies, also known as reconciliation errors. Results 2,473 patients had their treatment reviewed at the time of admission and 1,150 at discharge. 866 reconciliation discrepancies were detected in 446 patients (1.94 per patient). 807 (93 %) were accepted by the prescribing physician and classified as reconciliation errors. 16.8 % of patients had at least one reconciliation error: 63.8 % of these errors were incomplete prescriptions, 16.6 % were medication omissions and 10.5 % were errors in dosage, administration method and/or frequency. Conclusion The rate of medication errors found in this study is low compared with other similar studies. The most common error was “incomplete prescriptions”, most of them generated by the Accident and Emergency department. A computerised clinical history would help to decrease the number of reconciliation errors. Pharmacist interventions focused on medication reconciliation are well accepted by physicians, improving the quality of clinical histories and decreasing the number of medication errors that occur across transitions in patient care.


Similar content being viewed by others
References
Estudio Nacional sobre Efectos adversos ligados a la hospitalización. ENEAS 2005. [National Study on Hospitalisation-related Adverse Effects in Spain. ENEAS 2005] [cited 2013 March 1]. Available from: http://www.seguridaddelpaciente.es/contenidos/castellano/2006/ENEAS.pdf.
Rozich J, Resar R. Medication safety: one organization’s approach to the challenge. Qual Manag Health Care. 2001;8:27–34.
Cornish PL, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink DN, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–9.
Lessard S, DeYoung J, Vazzana N. Medication discrepancies affecting senior patients at hospital admission. Am J Health Syst Pharm. 2006;63:740–3.
Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health Syst Pharm. 2004;61:1689–95.
Rodríguez Vargas B, Delgado Silveira E, Bermejo Vicedo T. Estudio prospectivo de conciliación de la medicación al ingreso hospitalario. [Prospective study on conciliation of medication at the time of admission into hospital]. Aten Farm. 2011; 13(5):272-8.
Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173:510–5.
WHO Collaborating Centre for Patient Safety Solutions [cited 2013 March 1]. Available from: http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution6.pdf.
National Institute for Health and Clinical Excellence (NICE), National Patient Safety Agency. Technical patient safety solutions for medicines reconciliation on admission of adults to hospital [cited 2013 March 4]. Available from: http://guidance.nice.org.uk/PSG001/Guidance/pdf/English.
Joint Commission on Accreditation of Healthcare Organizations. Comprehensive accreditation manual for hospitals. Oakbrook Terrace, 2006 [cited 2013 March 1]. Available from: http://is.downstate.edu/is/jcaho/camh06/2006%20jcaho%20manual.pdf.
5 Million Lives Campaign. Getting Started Kit: Prevent Adverse Drug Events. How-to Guide: Prevent Adverse Drug Events by Implementing Medication Reconciliation. Cambridge, MA: Institute for Healthcare Improvement, 2011 [cited 2013 March 1]. Available from: http://www.ihi.org/knowledge/Pages/Tools/HowtoGuidePreventAdverseDrugEvents.aspx.
Roure Nuez C, Aznar Saliente T, Delgado Sánchez O, Fuster Sanjurjo L, Villar Fernández I. Grupo coordinador del grupo de trabajo de la SEFH de conciliación de la medicación. Documento de consenso en terminología y clasificación de los programas de conciliación de la medicación. [Consensus document on terminology and classification of medication reconciliation programmes, published by the Spanish Society of Hospital Pharmacy (SEFH)] Barcelona: Ediciones Mayo; 2009.
Delgado Sánchez O, Anoz Jiménez L, Serrano Fabiá A, Nicolás Picó J. Conciliación de la medicación [Medication Reconciliation]. Med Clin (Barc). 2007;129:343–8.
Sociedad Española de Farmacia Hospitalaria., 2020 Hacia el futuro con seguridad [Spanish Society of Hospital Pharmacy (SEFH), 2020, Looking ahead safely] [cited 2013 March 4] Disponible en http://www.sefh.es/sefhpdfs/2020b.pdf.
Evaluación de la seguridad de los sistemas de utilización de medicamentos en los hospitales españoles (2007) Informe. Mayo 2008 [Safety assessment of drug use systems in Spanish hospitals (2007) Report. May 2008] [cited 2013 March 4] http://www.seguridaddelpaciente.es/contenidos/castellano/2008/evaluacionSeguridadSistemasMedicamentos.pdf.
Evolución de la implantación de prácticas seguras de utilización de medicamentos en los hospitales españoles (2007–2011) [Progress of the implementation of safe practices of drug use in Spanish hospitals (2007–2011)] [cited 2013 March 4] http://seguridaddelpaciente.es/recursos/documentos/evolucion_practicas_seguras_medicamentos.pdf.
Climente-Martí M, García-Mañón ER, Artero-Mora A, Jiménez-Torres NV. Potential risk of medication discrepancies and reconciliation errors at admission and discharge from an inpatient medical service. Ann Pharmacother. 2010;44:1747–54.
Zoni AC, Durán García ME, Jiménez Muñoz AB, Salomón Pérez R, Martin P, Herranz Alonso A. The impact of medication reconciliation program at admission in an internal medicine department. Eur J Intern Med. 2012;23:696–700.
Hernández Prats C, Mira Carrió A, Arroyo Domingo E, Díaz Castellano M, Andreu Giménez L, Sánchez Casado MI. Conciliation discrepancies at hospital discharge. Aten Primaria. 2008;40:597–602.
Delgado Sánchez O, Nicolás Picó J, Martínez López I, Serrano Fabiá A, Anoz Jiménez L, Fernández Cortés F. Errores de conciliación en el ingreso y en el alta hospitalaria en pacientes ancianos polimedicados. Estudio prospectivo aleatorizado multicéntrico. [Reconciliation errors at admission and departure in old and polymedicated patients. Prospective, multicenter randomized study]. Med Clin (Barc). 2009;133:741–4.
Soler-Giner E, Izuel-Rami M, Villar-Fernández I, Real Campaña JM, Carrera Lasfuentes P, Rabanaque Hernández MJ. Calidad de la recogida de la medicación domiciliaria en urgencias: discrepancias en la conciliación [Quality of home medication collection in the emergency department: reconciliation discrepancies]. Farm Hosp. 2011;35:165–71.
Durán-García E, Fernandez-Llamazares CM, Calleja-Hernández MA. Medication reconciliation: passing phase or real need? Int J Clin Pharm. 2012;34(6):797–802.
Pàez Vives F, Recha Sancho R, Altadill Amposta A, Montaña Raduà RM, Anadón Chortó N, Castells Salvadó M. Abordaje interdisciplinar de la conciliación de la medicación crónica al ingreso en un hospital. [An interdisciplinary approach to reconciling chronic medications on admission to hospital]. Rev Calid Asist. 2010;25:308–13.
Gómez Valent M, García Argelaguet M, López Rico I, Pontes García C, Cruel Niebla M, Queralt Gorgas Torner M. Conciliación de la prescripción en pacientes quirúrgicos. [Medication reconciliation in surgical patients]. Aten Farm. 2012;14:160–6.
ISMP´s list of high-alert medications [cited 2013 June 12] Available from: http://www.ismp.org/tools/highalertmedications.pdf.
Grupo REDFASTER. Guía para la conciliación de los medicamentos en los Servicios de Urgencias. [Medication reconciliation in Accident and Emergency department Guide]. Sociedad Española de Farmacia Hospitalaria. 2012. Available from: http://www.fasterweb.es/documentos/guia_conciliacion.pdf.
Acknowledgments
We would like to thank the physicians in the Internal Medicine Unit on the 12th floor of the Lozano Blesa Clinical Hospital in Zaragoza for all their help with the day-to-day work involved in this study, which would not have been possible without their cooperation.
Funding
This project was funded with cohesion funds provided by the Autonomous Region of Aragon.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 4.
Rights and permissions
About this article
Cite this article
Allende Bandrés, M.Á., Arenere Mendoza, M., Gutiérrez Nicolás, F. et al. Pharmacist-led medication reconciliation to reduce discrepancies in transitions of care in Spain. Int J Clin Pharm 35, 1083–1090 (2013). https://doi.org/10.1007/s11096-013-9824-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-013-9824-6