Abstract
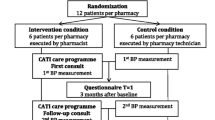
Objective: The primary objective of this study was to evaluate the effect of a pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. The clinical outcomes of this pharmacotherapy adherence approach were the secondary objective of the study. Setting: Public Primary Health Care Unit in a municipality in the Brazilian State of Sao Paulo. Method: A 36-month randomized, controlled, prospective clinical trial was carried out with 200 patients divided into two groups: control (n = 100) and intervention (n = 100). The control group received the usual care offered by the Primary Health Care Unit (medical and nurse consultancies). The patients randomized into the intervention group received pharmaceutical care intervention besides the usual care offered. Main outcome measure: Pharmacotherapy adherence (Morisky-Green test translated into Portuguese and computerized dispensed medication history) and clinical measurements (blood pressure, fasting glucose, A1C hemoglobin, triglycerides and total cholesterol) were evaluated at the baseline and up to 36 months. A P value <0.05 was considered statistically significant. Results: A total of 97 patients from the intervention group and 97 patients from the control group completed the study (n = 194). Significant improvements in the pharmacotherapy adherence were verified for the intervention group according to the Morisky-Green test (50.5% of adherent patients at baseline vs. 83.5% of adherent patients after 36 months; P < 0.001) and the computerized dispensed medication history (52.6% of adherent patients at baseline vs. 83.5% of adherent patients after 36 months; P < 0.001); no significant changes were verified in the control group. Significant improvements in the number of patients reaching adequate values for their blood pressure (26.8% at baseline vs. 86.6% after 36-months; P < 0.001), fasting glucose (29.9% at baseline vs. 70.1% after 36 months; P < 0.001), A1C hemoglobin (3.3% at baseline vs. 63.3% after 36 months; P < 0.001), triglycerides (47.4% at baseline vs. 74.2% after 36 months; P < 0.001) and total cholesterol (59.8% at baseline vs. 80.4% after 36 months; P = 0.002) were verified in the intervention group, but remained unchanged in the control group. Conclusion: These results indicated the effectiveness of pharmaceutical care in improving pharmacotherapy adherence, with positive effects in the clinical outcomes of the patients studied.

Similar content being viewed by others
References
International Diabetes Federation. Diabetes Atlas. 4th ed. Brussels: International Diabetes Federation; 2009. ISBN-13: 978-2-930229-71-3. Available: http://www.diabetesatlas.org/content/diabetes.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
Bloch KV, Melo AN, Nogueira AR. Prevalence of anti-hypertensive treatment adherence in patients with resistant hypertension and validation of three indirect methods for assessing treatment adherence. Cad Saude Publica. 2008;24(12):2979–84.
Krapek K, King K, Warren SS, George KG, Caputo DA, Mihelich K, et al. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother. 2004;38(9):1357–62.
Prado JC, Kupek E, Mion D. Validity of four indirect methods to measure adherence in primary care hypertensives. J Hum Hypertens. 2007;21(7):579–84.
DiMatteo MR. Evidence-based strategies to foster adherence and improve patient outcomes. JAAPA. 2004;17(11):18–21.
Odegard OS, Gray SL. Barriers to medication adherence in poorly controlled diabetes mellitus. Diabetes Educ. 2008;34(4):692–7.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;(2):CD000011.
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43.
Krass I, Taylor SJ, Smith C, Armour CL. Impact on medication use and adherence of Australian pharmacists’ diabetes care services. J Am Pharm Assoc. 2005;45(1):33–40.
Planas LG, Crosby KM, Mitchell KD, Farmer KC. Evaluation of a hypertension medication therapy management program in patients with diabetes. J Am Pharm Assoc. 2009;49(2):164–70.
Sá-Borges AP, Guidoni CM, Ferreira LD, Freitas O, Pereira LRL. The pharmaceutical care of patients with type 2 diabetes. Pharm World Sci. 2010;32(6):730–6.
Lyra-Júnior DP, Marcellini PS, Pelá IR. Effect of pharmaceutical care intervention on blood pressure of elderly outpatients with hypertension. Braz J Pharm Sci. 2008;44(3):451–7.
Obreli-Neto PR, Cuman RKN. Pharmaceutical care program for the rational use of drugs in the elderly users of a Basic Health Unit in the Sao Paulo State, Brazil. Lat Am J Pharm. 2010;29(3):333–9.
Correr CJ, Pontarolo R, Wiens A, Rossignoli P, Melchiors AC, Radominski R, et al. Economic evaluation of pharmacotherapeutic follow-up in type 2 diabetes mellitus patients in community pharmacies. Arq Bras Endocrinol Metabol. 2009;53(7):825–33.
Brazilian Society of Cardiology, Brazilian Society of Hypertension, Brazilian Society of Nephrology. V Brazilian guidelines on hypertension. Arq Bras Cardiol. 2007;89(3):24–79.
Brazilian Society of Diabetes. Brazilian Society of Diabetes’ Guidelines 2009. Rio de Janeiro, RJ: Diagraphic Editora; 2009.
Strand LM, Cipolle RJ, Morley PC, Frakes MJ. The impact of pharmaceutical care practice on the practitioner and the patient in the ambulatory practice setting: twenty-five years of experience. Curr Pharm Des. 2004;10(31):3987–4001.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of self-reported measure of medication adherence. Med Care. 1986;24(1):67–74.
Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60(7):657–65.
Takiya L, Peterson AM, Finley R. Meta-analysis of interventions for medication adherence to antihypertensives. Ann Pharmacother. 2004;38(10):1617–24.
Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36(8):1138–61.
Becker MH, Maiman LA. Strategies for enhancing patient compliance. J Community Health. 1980;6(2):113–35.
Lee LK, Grace KA, Taylor JA. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296(21):2563–71.
George J, Phun YT, Bailey MJ, Kong DC, Stewart K. Development and validation of the medication regimen complexity index. Ann Pharmacother. 2004;38(9):1369–76.
Lyra-Júnior DP, Kheir N, Abriata JP, Rocha CE, Santos CB, Pela IR. Impact of pharmaceutical care interventions in the identification and resolution of drug-related problems and on quality of life in a group of elderly outpatients in Ribeirào Preto (SP), Brazil. Ther Clin Risk Manag. 2007;3(6):989–98.
Al Mazroui NR, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with Type 2 diabetes mellitus. Br J Clin Pharmacol. 2009;67(5):547–57.
Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice: the clinician’s guide. New York, NY: The McGraw-Hill Companies; 2004. ISBN: 10: 0-07-136259-2.
Niquille A, Bugnon O. Relationship between drug-related problems and health outcomes: a cross-sectional study among cardiovascular patients. Pharm World Sci. 2010;32(4):512–9.
Kicklighter CE, Nelson KM, Humphries TL, Delate T. An evaluation of a clinical pharmacy-directed intervention on blood pressure control. Pharm Practice. 2006;4(3):110–6.
Brawley LR, Culos-Reed SN. Studying adherence to therapeutics regimens: overview, theories, recommendations. Control Clin Trials. 2000;21(5):156–63.
Acknowledgments
The authors would like to thank the pharmacists and researchers for their assistance during the research.
Funding
None.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Obreli-Neto, P.R., Guidoni, C.M., de Oliveira Baldoni, A. et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm 33, 642–649 (2011). https://doi.org/10.1007/s11096-011-9518-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-011-9518-x