Abstract
Purpose
The goal of this research is to develop stable formulations for live attenuated influenza vaccines (LAIV) by employing the drying methods freeze drying, spray drying, and foam drying.
Methods
Formulated live attenuated Type-A H1N1 and B-strain influenza vaccines with a variety of excipient combinations were dried using one of the three drying methods. Process and storage stability at 4, 25 and 37°C of the LAIV in these formulations was monitored using a TCID50 potency assay. Their immunogenicity was also evaluated in a ferret model.
Results
The thermal stability of H1N1 vaccine was significantly enhanced through application of unique formulation combinations and drying processes. Foam dried formulations were as much as an order of magnitude more stable than either spray dried or freeze dried formulations, while exhibiting low process loss and full retention of immunogenicity. Based on long-term stability data, foam dried formulations exhibited a shelf life at 4, 25 and 37°C of >2, 1.5 years and 4.5 months, respectively. Foam dried LAIV Type-B manufactured using the same formulation and process parameters as H1N1 were imparted with a similar level of stability.
Conclusion
Foam drying processing methods with appropriate selection of formulation components can produce an order of magnitude improvement in LAIV stability over other drying methods.
Similar content being viewed by others
Introduction
The three human influenza pandemics in the 20th century killed tens of millions of people throughout the world. And while the more recent outbreak in 2009 caused by the H1N1 influenza virus did not cause high mortality in the general population as did the viruses responsible for influenza pandemics in the last century, its rapid spread reminded us of the shortcomings of our current vaccination capabilities and the need to improve our ability to respond quickly. One of the major challenges for containing the virus is the speed and capacity of vaccine production and distribution to meet the global immunization need. Without improvements, it is anticipated that the vaccine shortages experienced in 2009 will occur again should another outbreak take place. Influenza vaccines are generally used within months of production, thus the stability and shelf life of these vaccines have not been major issues. However, the ability to stockpile influenza vaccine for years at a time greatly improves our pandemic preparedness. Further, with improved vaccine stability that obviates the need for the cold chain in distribution, the ability to get the vaccine where it needs to be is greatly enhanced.
Since 1997, avian influenza A H5N1 virus has caused widespread outbreaks in poultry and other bird populations. Sporadic human infections occurred in several regions of the world and the disease has become endemic in Southeastern Asia. The mortality rate in humans is nearly 60% according to data from World Health Organization (WHO) (1). Currently, the H5N1 virus has not caused extensive human-to-human transmission, and outbreaks have been contained successfully. The concern of the scientific community is that a highly virulent H5N1 virus capable of human-to-human spread may emerge as the result of reassortment between H5N1 virus and seasonal influenza virus, causing another catastrophic pandemic in the future. Thus, H5N1 remains a major threat for another potential pandemic which may be more deadly than the 2009 H1N1 virus-related pandemic.
Pandemic influenza preparedness, as detailed in the Implementation Plan for the National Strategy for Pandemic Influenza, focuses extensively on the establishment and maintenance of stockpiles of H5N1 influenza vaccine and on the rapid immunization of citizens when there is an outbreak (2). The United States Government has stockpiled approximately 23 million doses of H5N1 split vaccine. The formulation of the stockpiled H5N1 split vaccine is based on the formulation of the seasonal influenza vaccine, which has a relatively short shelf life under refrigeration conditions (Table I).
The existing formulations of H5N1 influenza vaccines are not ideal for either long-term stockpiling or for rapid deployment to contain an outbreak of a potential pandemic. It is very expensive to establish and maintain the stockpile of H5N1 split vaccine due to high manufacturing costs and turnover of the stockpile. It costs approximately US$1 billion for the United States Government to establish a 23 million dose vaccine stockpile (4). Split influenza vaccine is expected to have a shelf life of 2 to 3 years based on the seasonal vaccine, during which the potency of the vaccine gradually decreases. It is anticipated that the stockpiled H5N1 vaccine will be discarded at the end of its shelf life and will need to be replaced with newly produced vaccine.Footnote 1 This has already begun to occur with the procurement by the Department of Health and Human Services in 2008 of 1.2 million doses of H5N1 bulk vaccine to “replenish losses due to diminished product stability over the past 4 years.” (5)
Currently stockpiled H5N1 vaccines are not ideal for rapid deployment. It is essential to immunize people in the affected area quickly once the outbreak takes place. A contagious influenza virus can spread to several continents in a matter of days to a couple of weeks. It may take 1 to 3 months to deploy the stockpiled split H5N1 influenza vaccine for the following reasons:
-
These vaccines are stockpiled in bulk and separately from the adjuvant (a component that lowers the required quantity of vaccine antigen per dose, thus enabling immunization of more people with the stockpiled vaccine).
-
All stockpiles are stored at the manufacturers’ facilities, which may be far away from where the disease outbreaks occur. When vaccine is needed, the manufacturers need to complete the blending, fill-and-finish, and testing before releasing the products.
-
Current vaccines can only be distributed using a rate-limiting cold chain system in order to maintain the vaccines’ potency. Because of the need for a cold chain, administration of the current vaccines must take place in traditional settings, such as doctors’ offices and pharmacies.
To date, there is no stockpiled live attenuated H5N1 vaccine. By analogy to the live attenuated H1N1 vaccine, a live attenuated H5N1 vaccine would have a much higher production yield than the split influenza vaccine—thus it is an attractive option for stockpiling. However, the existing formulations of live attenuated vaccine (H1N1 or seasonal influenza vaccines) are only stable for a few months when stored at 4°C and are not stable at all at higher temperatures, making it impossible to create a stockpile.
In comparison to inactivated or subunit-based vaccines, live attenuated vaccines have the advantage of exhibiting a natural antigenic profile, replicative competency, and mimic the natural route of infection, thus eliciting a longer-lasting and more comprehensive immune response without the need for a booster or adjuvant (6). However, as with most live vaccines, storage stability is more difficult to maintain than with protein based vaccines. The stability of LAIV during long-term storage and possible temperature excursions during shipment can limit their implementation.
A recent review of the challenges and approaches in addressing issues of vaccine stabilization has been provided by Kumru et al. (7). The current live attenuated viral vaccines on the market are either formulated in the dry state (lyophilized or tablet) and/or require frozen storage to guarantee shelf life of more than 1 year, with the possible exception of Merck’s RotaTeq rotavirus vaccine, which is a refrigerated (2–8°C) liquid formulation. All require some form of refrigeration to guarantee shelf life.
This paper summarizes research and development efforts to design dried LAIV formulations with enhanced thermal stability through application of plasticizer technology. Plasticizer technology was developed by Aridis Pharmaceuticals for stabilizing biopharmaceuticals by encasing the biologic in a glassy matrix that minimizes chemical and physical degradation. The glassy matrix is formed by excipients with high glass transition temperature, such as sugars. Judicious addition of plasticizers (such as glycerol or sorbitol) can dampen local molecular motion within the glass, further enhancing stability (8–10). This technology has previously been used to successfully stabilize bacterial and viral vaccines such as parainfluenza virus (PIV) (11), respiratory syncytial virus (RSV) (unpublished), Measles (12), Typhoid (Ty21a) (13), Anthrax pA antigen (13), adenovirus (14), and rotavirus (15).
Following a similar approach as Abdul-Fattah and coworkers for PIV (11), three drying methods to produce solid LAIV formulations with this glassy matrix were examined, including foam (or, equivalently, vacuum) drying, spray drying and freeze drying (or lyophilization). It is known the excipient profile of an optimized formulation can make a substantial impact on the stability of the vaccine and can vary significantly for each drying method in order to address differences in process stresses as well as in the physicochemical properties of the final solid dosage form. Therefore, in contrast to (11) where only two formulations (one with and one without surfactant) were used for all the drying methods, lead formulation candidates in our current studies were selected following independent excipient screenings. These partially optimized formulations were tailored to each of the three drying methods in order to provide a more fair assessment of each process’ ability to stabilize the vaccine. However, similar to (11), the same lead foam dried formulations were also freeze dried to provide a direct comparison of stability based solely on drying method. In addition, a commercial freeze dried formulation of the LAIV was included in the stability study to again compare a more optimized formulation specific to the freeze drying method.
All three methods of drying begin with an aqueous formulation containing a variety of excipients in addition to the biologic agent, but differ in how the water is removed. In foam drying the bulk of the removal is accomplished essentially by boiling off the water at moderate temperatures under vacuum to produce a foamy closed-cell structure as the final product. In freeze drying the water is frozen at low temperature before water removal occurs under vacuum by sublimation, producing a more dense porous solid or “cake”. Both of these methods are generally performed by loading the formulated “wet blend”Footnote 2 into vials and removing the water with equipment that can create the required vacuum environment and controlled temperatures (i.e. freeze driers or lyophilizers). In spray drying the liquid is sprayed from a nozzle generally at elevated temperatures to produce a fine mist of droplets; as the droplets pass through a drying chamber solvent is removed by rapid evaporation causing them to solidify into powder particles, which are ultimately collected by a cyclone centrifuge before being vialed. While foam drying is the least mature technology, particularly in the pharmaceutical industry where no commercial products are produced by this method, we hope to show in this study that it can offer significant advantages for stabilization of some biologics such as LAIV. Other drying methods such spray freeze drying have also been used to produce dried LAIV powders (16). A more detailed comparison of these different drying methods as applied to vaccines can be found in a recent review by Otake et al. (3).
The initial work in this study involved application of plasticizer technology to several LAIV vaccine formulations using both foam drying and spray drying processes. This was accomplished by screening a variety of formulation compositions selected based on past experience in successfully stabilizing other live viral vaccines. Lead formulations with the best balance of process and storage stability were identified for each drying method through this initial screening under accelerated storage conditions. LAIV stability in standard lyophilized formulations that mimicked select lead foam dried formulations was also studied for comparison. The main focus here is to present the long term stability (LTS) results for the lead formulations under the three drying methods at various temperatures, as well as immunogenicity results in a ferret model. The goal of this effort was to demonstrate a formulation/drying process combination that provids storage stability meeting the targets of less than 1 log TCID50/ml potency loss in 156 weeks at 4°C, in 12 weeks at 25°C and in 4 weeks at 37°C.
Materials & Methods
Formulation Components
LAIV Vaccines
The live attenuated Type-A H1N1 and B-strain influenza vaccines used in these studies were obtained from the Serum Institute of India (SII). The Type-A strain H1N1 was supplied both in bulk liquid form and as a formulated freeze dried solid, the latter of which is marketed by SII as the commercial product NASOVAC™. This LAIV was developed using the backbone of attenuated strain A/Leningrad/134/17/57 from the Institute of Experimental Medicine (IEM), Russian Federation but has the A/17/California/2009/38 antigenic specificity of Hemagglutinin and Neuraminidase identical to the wild type virus of the H1N1 2009 pandemic strain. The formulated freeze dried NASOVAC™ excipient composition upon reconstitution is claimed by SII to be: Gelatin (Partially hydrolyzed) 2.5%, Sorbitol 5%, L-Alanine 0.1%, L-Histidine 0.21%, Tricine 0.3%, L-Arginine hydrochloride 1.6%, Lactalbumin hydrolysate 0.35%, Phosphate buffer saline Base. The LAIV Type-B was a B/Brisbane/60/2008-like reassortant that was supplied in a media consisting of 7.2% sucrose, 11 mM phosphate and 5 mM glutamate.
Storage of the SII LAIV bulk at −80°C showed no activity loss over 12 weeks, while the potency of the material declined at a rate of 0.056 log TCID50/mL per week when stored at 4°C. Based on these results, the bulk material was stored frozen at −80°C and working aliquots were stored at 4°C for no longer than 1 week. It was also found that a significant potency loss from samples being placed directly in the −80°C freezer could largely be avoided by flash freezing with liquid nitrogen.
Formulation Excipients
A variety of excipients were included in the formulations evaluated in formulation screening and LTS studies. These are listed in Table II with their classification.
pH Measurement
The pH of the formulations was measured with a VWR Symphony pH meter (model SB21). The meter was calibrated with three references solutions (pH 4.0, 7.0 and 10.0, Orion Application Solution, Thermo Electron Corporation) prior to each measurement. pH adjustment was performed by titration with 1 N potassium hydroxide or hydrochloric acid solution.
Residual Moisture Content
Residual moisture content in the samples was measured by Karl Fischer (KF) titration using an Aquacounter AQ-300 coulometric titrator (Hiranuma Sangyo, lbaraki, Japan). KF titration measures trace quantities of water in a sample based on the stoichiometric reaction of water with sulfur dioxide and iodine in an anhydrous solution containing a suitable base. A weighed amount of solid sample is dissolved in a measured amount of Hydranal® Coulomat AG solvent (Riedel-de Haën Laboratory Chemicals, Sigma-Aldrich Inc.) in a dry serum glass vial, which is capped with a butyl rubber stopper and aluminum crimp seal. A measured amount of this sample solution is injected into the titration cell for analysis to determine the moisture content of the sample. The measurement is blank corrected with pure solvent, and the percent weight of moisture in the sample is calculated. Instrument calibration is also verified using Hydranal® water standards (Sigma Aldrich). All measurements were performed in triplicate. Relative standard deviations were generally less than 25%, with the highest being for freeze dried samples with the lowest moisture content.
Thermal Analysis
Differential scanning calorimetry (DSC) was performed on dried samples to determine their glass transition temperature (Tg). A Mettler Toledo DSC821e was used for this purpose. Samples were loaded into 100uL DSC Crucible Set Aluminum pans (Mettler Toledo part no. ME-51119872) and hermetically sealed with Aluminum lid (Mettler Toledo part no. ME-51119871) using a Mettler Toledo Crucible Sealing Press. The weight of samples was determined on a Mettler Toledo balance AG204. Prior to analyzing a sample, instrument calibration was performed using a 99.99% Indium standard. During sample analysis, the sample was held at −20°C for 5 min followed by a temperature ramp from −20 to 150 at 7°C/min. STARe Thermal Analysis Software (Mettler Toledo) was used to analyze the results and determine the Tg values, indicated by the midpoint of the transition. All measurements were performed in duplicate and standard deviations were less than 1°C.
TCID50 Potency Assay
Madin Darby Canine Kidney (MDCK) cells from ECACC (European Collection of Cell Cultures) were used for the TCID50 assay. In order to increase throughput and reduce human subjectivity relative to the manual microscopy-based method for detecting the cytopathic effect (CPE), a colorimetric detection system utilizing MTT dye ([3-{4,5-dimethyliazol-yl)-2,5 diphenyltetrazolium bromide]) was developed. Data demonstrated that the MTT method provided reliable detection of CPE in MDCK cells inoculated with LAIV and comparable titer estimates to the microscopy method. Hence, the MTT-based TCID50 assay was used to measure LAIV potency throughout formulation development.
The detailed method included growth of the MDCK cells in a 96-well assay plate at 20,000 cells/well in a humidified 37°C incubator 5% CO2 for 2 days or until confluency of the cell monolayer was reached. On the day of the assay, the assay plates were washed and replenished with fresh media prior to virus inoculation. The samples were pre-diluted in the assay media to a virus concentration appropriate for the assay. The pre-diluted samples were dispensed into a 96-well dilution block containing fixed amount of assay media with added Trypsin at 1:10 initial dilution followed by a step-wise ten-fold serial dilution leaving one well without the virus for cell control. The serially diluted virus sample and the control were inoculated onto the MDCK assay plates in multiples of six replicates then kept in a humidified 36°C incubator, 5% CO2 for 6 days to allow the infection to develop. At the 6th day post-infection, the cytopathic effect (CPE) was determined.
To determine the reproducibility and robustness of the MTT-based CPE read-out, a comparison was made with the manual read-out method by running 20 assay replicates each day for 2 days. After the manual count of the CPE by microscopy was recorded, the media was removed from the assay plate and replaced with the MTT dye diluted in assay media. This was followed by incubation at 37°C, 5% CO2 for a few hours until the yellow tetrazolium salt was reduced to purple formazan crystals which were then solubilized by the addition of a detergent. The color development was quantified by absorbance using a spectrophotometer equipped with a plate reader. The absorbance values were transferred to a spreadsheet to calculate the titer read-out. The absorbance cut-off value was derived by the standard deviation of the absorbances from the series of non-infected wells and multiplying by 2 (2 standard deviations) and subtracting from the threshold mean. Absorbance values below the cut-off level were counted as positive CPE’s. The variability (95% confidence interval) of the MTT dye method was ±0.3 log TCID50/mL for the 20 replicates. Similar variability was observed on a different day for 20 replicates. The average difference between the MTT-dye method and the manual microscopy method was 0.1 log TCID50/mL. The titer from the manual method was calculated by converting the CPE counts using the Karber table with adjustments for final dilution of the sample on the assay plate.
Foam Drying Process Development
Foam drying is a water (or solvent) removal process that is carried out under vacuum without ever freezing the liquid being removed. Water is removed by lowering the pressure below the liquid vapor pressure (i.e. boiling) and, as the dissolved solids concentration increases and the liquid becomes more viscous, it begins to foam forming static bubbles; the final dried product is a solid foamy structure (See Fig. 6). This is in contrast to lyophilization (or freeze drying) were the water is removed by sublimation. Thus the advantage of foam drying is that it avoids the stresses associated with freezing, in addition to producing drug product with minimal interfacial area relative to either freeze drying or spray drying (spray drying generates the highest specific surface of the three dried products) (17); both conditions are associated with enhanced stability of the formulated biologics, particularly those sensitive to these mechanisms of inactivation. Typically the initial total solids content associated with the wet blend for foam drying is significantly higher than in freeze or spray drying, as it not only provides less burden on the drying process to remove the water and helps to reduce splashing on the vial walls because of the initially more viscous solution, the lyophilization requirement to produce an “elegant” cake and the aerosolization nozzle shear/pressure or particle size constraints in spray drying do not apply to foam drying.
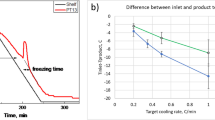
The foam drying process for manufacture of dried formulations was performed using a VirTis AdVantage 2.0 XL-70 laboratory scale freeze dryer. The liquid formulations were dispensed as 1 ml into 10 ml USP Type 1 borosilicate glass serum vials (24 × 50 mm (Dia.x H) 13x20mm (Mouth I.D x O.D.), Wheaton) and later sealed with gray chlorobutyl rubber stoppers (3 leg lyo (13x20mm), Wheaton). Prior to formulation screening, the drying process conditions were determined by foam-drying the placebo formulations consisting of a buffer in combination with sugars, polymers, surfactants, plasticizers and/or other stabilizers. Beginning with an initial solids content of approximately 30 wt%, the foam drying conditions were designed to give a stable foam structure with residual moisture level between 2 and 4%, as measured by Karl Fischer titration. The final process for producing the LTS samples utilized a cycle that ran at temperatures ranging from 15 to 45°C, as the pressure was progressively lowered to 100 mTorr to start the cycle. Specifically, the 72 h process had the following steps:
Foam Drying Cycle | ||||
Step | Temperature | Time | Condition | Vacuum |
( °C) | (min) | (mTorr) | ||
1 | 15 | 120 | Hold | 100 |
2 | 15 | 1250 | Hold | 100 |
3 | 20 | 50 | Ramp | 100 |
4 | 20 | 300 | Hold | 100 |
5 | 35 | 150 | Ramp | 100 |
6 | 35 | 300 | Hold | 100 |
7 | 40 | 50 | Ramp | 100 |
8 | 40 | 1250 | Hold | 100 |
9 | 40 | 600 | Hold | 100 |
10 | 45 | 50 | Ramp | 100 |
11 | 45 | 200 | Hold | 100 |
At the end of the cycle the freeze dryer was back-filled with Argon just prior to stoppering the vials. Vials were immediately crimped with an aluminum seal upon removal from the freeze dryer.
Freeze Drying Process Development
The freeze drying process for manufacture of lyophilized formulations was also performed with the VirTis AdVantage 2.0 XL70 freeze dryer. The liquid formulations were dispensed as 0.5 ml into 3 ml USP Type 1 borosilicate glass serum vials (17x38mm (Dia. x H), 7 × 13 mm (Mouth I.D x O.D.), Wheaton) and later sealed with gray chlorobutyl rubber stoppers (2 leg Lyo (7x13mm), Wheaton). However, in contrast to foam drying, the liquid formulation is first frozen at low temperature prior to lowering the pressure, which allows the bulk of the water to be removed by sublimation of the ice that forms. The freeze dried formulations were produced with a conservative drying cycle with the process ramping the temperature from −45 to 25°C at a pressure of 100 mTorr over the course of over 2 days. Following a freeze step at −45°C for 2 h and a ramp down to 100 mTorr (about 20 min), the detailed drying cycle was as follows:
Freeze Drying Cycle | ||||
Step | Temperature | Time | Condition | Vacuum |
( °C) | (min) | (mTorr) | ||
1 | −45 | 30 | Hold | 100 |
2 | −31 | 140 | Ramp | 100 |
3 | −31 | 720 | Hold | 100 |
4 | −31 | 720 | Hold | 100 |
5 | −31 | 720 | Hold | 100 |
6 | −12 | 190 | Ramp | 100 |
7 | −12 | 240 | Hold | 100 |
8 | 15 | 135 | Ramp | 100 |
9 | 15 | 360 | Hold | 100 |
10 | 25 | 150 | Ramp | 100 |
11 | 25 | 300 | Hold | 100 |
At the end of the cycle the freeze dryer was back-filled with Argon just prior to stoppering the vials. Vials were immediately crimped with an aluminum seal upon removal from the freeze dryer.
The freeze drying conditions were designed to give a good cake structure and residual moisture levels near 1–2 wt%, consistent with typical lyophilized products. The lower moisture content realistically achievable with this drying method is a result of the combined effect of the higher specific surface area (relative to foam drying) (17) and the very low vacuum pressures over extended periods of time (relative to spray drying).
Spray Drying Process Development
The spray drying process for manufacture of lead formulations was performed using a Büchi Mini Spray Dryer Model B-190 (Flawil, Switzerland). The spray dryer was housed in a temperature- and humidity-controlled, nitrogen environment enclosure, maintained at 26.5 to 29.5°C with liquid nitrogen and at less than 10% relative humidity by circulation through a calcium sulfate canister. The formulated solutions were atomized using a custom low pressure, two-fluid nozzle energized with high frequency sonic or ultrasonic vibrations to reduce stresses on the virus and minimize process loss (18). The resulting droplets were dried by evaporation in a heated nitrogen gas stream supplied from the enclosure. The dry powder was collected using a cyclone separator, and then manually transferred within the environmental enclosure in approximately 100 mg portions into individual USP Type 1 serum borosilicate glass 2 ml vials (15 × 32 mm (Dia. x H), 7 × 13 mm (Mouth I.D x O.D.), Wheaton) with gray chlorobutyl rubber stoppers (2 leg Lyo (7 × 13 mm), Wheaton) for later characterization and stability testing.
Prior to formulation screening, the spray drying process conditions were determined by spray-drying placebo formulations consisting of a buffer in combination with sugars, polymers, surfactants, plasticizers and/or other stabilizers. The process parameters were adjusted to maintain a nozzle outlet temperature of approximately 45°C. Inlet temperatures were typically about 60°C with nozzle pressures up to 24 psi and a nominal 1 ml/min liquid feed rate. The spray-drying conditions were designed to generate powders with at least 50% mass yield and residual moisture levels between 1 and 4%. The moisture content of the powders produced by spray drying are generally higher than that of a freeze dried product because the system is operated at atmospheric pressure and must rely on rapid evaporation in the drying chamber (on the order of seconds) to remove moisture, versus several hours under vacuum for the later. The small particles generated (1–40 μm) provide high specific surface area (17) relative to either freeze or foam drying, which, when combined with the elevated drying temperatures, partially make up for these drying disadvantages, but, unfortunately, can also lead to greater process and storage losses in potency.
Formulation Screening
A total of 39 foam dried formulations and 30 spray dried formulations were initially evaluated in a partial factorial DOE in order to identify critical excipients and select lead formulations. These formulations contained 3 to 10 components. Each formulation contained at least one sugar and one buffer. The excipient concentration levels and the overall composition of the formulations were selected based on prior experience with other dried vaccine formulations; the composition ranges for the wet blends are listed in Table III.
The impact of individual excipients on the final formulation stability is described in the Results section below.
Long-Term Stability Study
Three lead foam dried formulations, one lead freeze dried formulation and two lead spray dried formulations were manufactured in order to evaluate real-time storage stability. For bookkeeping, the suffix “LTS” was appended to the formulation ID of the new batches generated for the long-term stability study (e.g., FM3LTS). The excipient profile of these formulations is provided in Table IV.
Also included in the study was the freeze dried formulation NASOVAC™ (composition given in Formulation Components section), which is a marketed product by Serum Institute of India. Storage stability was evaluated at 4, 25, and 37°C for up to 74 weeks using triplicate samples at each time point. Throughout the study, pH and moisture content of all formulations remained stable.
Process stability was determined by measuring viral titer pre- and post-drying using the TCID50 assay. Process stability results are reported as process loss, which was calculated by subtracting the titer of the reconstituted dried sample from the pre-dried sample titer.
Storage stability was assessed by monitoring at various time points the viral titer of samples stored under specified temperature-controlled conditions. Storage stability results are presented as the rate of titer loss, which was calculated by multiplying the linear slope of the temporal viral titer measurements by −1, i.e. a positive rate of titer loss reflects sample degradation. Specifically, the storage stability of the formulations was quantified by simple linear regression of the data for the measure potency of the reconstituted samples over time and expressed as the negative slope of a linear model fitted by ordinary least squares to a plot of log TCID50/ml versus weeks of storage for a given formulation in the units of log TCID50/ml/week. Models other than linear did not consistently improve the fit of the data and therefore, to maintain comparative equivalence between the different formulations and drying methods, they were not included in the analysis. The analysis was performed using SigmaPlot® (Systat Software Inc.), which provided the slope as well as its standard error and 95% confidence limits, which was subsequently used to estimate the projected time for 1 log TCID50/ml loss in titer.
Immunogenicity Study
Lead foam dried, spray dried and freeze dried LAIV formulations were evaluated in ferrets for safety and immunogenicity. These formulations were prepared at a higher target titer than used in stability studies in order to enable dosing at levels consistent with published literature. Groups of five seronegative (800–1100 g) male ferrets (Triple F Farms, Sayre, PA, USA) were administered with each formulation by nasal instillation (0.1 mL per nare) under anesthesia to assess safety and immunogenicity. The frozen LAIV bulk that was used to manufacture the dried formulations served as a control in the study. The priming dose was administered approximately 4 weeks after the formulations were manufactured. A second boosting dose was administered 4 weeks after the priming dose. Blood samples were collected prior to each dose, and 4 weeks after the boost. Immunogenicity of the formulations was assessed using the serum hemagglutination inhibition (HAI) assay as described previously (19). Briefly, serum from individual ferrets was treated with receptor destroying enzyme (RDE, Denka Seiken, LTD, Tokyo Japan), heat inactivated, and serially diluted in phosphate buffered saline. Influenza A viruses are added to each dilution, followed by incubation at room temperature. HAI titer is reported as the inverse of the highest dilution of serum that inhibits agglutination of turkey RBC’s.
Results
Formulation Screening
Formulations for the screening studies were selected based on previous experience with biologics stabilization utilizing these drying technologies. The formulations were generated by modest perturbation from a few base formulations (all containing at least one sugar and a buffer) that have worked successfully in the past, with the excipient contents of the wet blend within the ranges provided in Table III.
Screening of Foam Dried Formulations
In the initial screening of 39 excipient combinations, plasticizer technology using foam drying was applied to stabilize the LAIV formulations. These formulations were screened based on their ability to maintain viral potency through the drying process and during storage under accelerated conditions at 37°C for 12 weeks. Three lead foam dried formulations were selected and tested for long-term storage stability at 4, 25, and 37°C in a 74 week study.
Foam drying transformed all 39 liquid formulations into glassy, closed-cell foams with residual moisture contents between 2 and 5%wt. In general, a modest process-related reduction in viral titer was observed after foam drying <1 TCID50/mL. The majority of the foam dried formulations appeared to be relatively stable at 37°C with viral titer slowly declining over a 12 week study at an average rate of 0.15 ± 0.24 log TCID50/mL/wk, and 9 formulations (24%) less than 0.05 log TCID50/mL/wk. This rate of titer loss was significantly slower than observed with formulations prepared by spray drying or freeze drying. There was no discernible correlation between the residual moisture content in the foams and process or storage stability. Hence, changes in stability were assumed to be related to changes in formulation composition.
Formulation screening identified gelatin and arginine as key stabilizers for foam dried LAIV (Fig. 1). The rate of viral titer loss during storage at 37°C was 0.06 ± 0.03 log TCID50/mL/wk for formulations containing gelatin, as compared to 0.28 ± 0.16 log TCID50/mL/wk for formulations without gelatin. The high percent relative standard deviation for these quantities (50–57%) is the result of the variability in stability of the different formulations, coupled with the fact that the rates of titer loss overall were rather low. In the absence of gelatin, arginine proved to be an important stabilizer. The mean rate of titer loss for gelatin-free formulations with and without arginine was 0.13 ± 0.08 and 0.39 ± 0.09 log TCID50/mL/wk, respectively. In gelatin-containing formulations, the addition of arginine did not further improve storage stability. While both gelatin and arginine improved storage stability, neither appeared to impact process stability (data not shown).
Sucrose and trehalose were comparable stabilizing / bulking agents. Plasticizers, which are believed to dampen molecular vibrations and thus enhance protection from degradation mechanisms, seemed to improve LAIV stability in certain formulations, but a more robust factorial formulation study design would be needed to determine with greater confidence the relative benefit of the plasticizers. There was not an obvious advantage of one buffer system over another. LAIV stability was comparable in formulations with and without Pluronic F68. Similarly, inclusion of methionine, EDTA, or metal ions did not notably improve LAIV stability. Due to the limited formulation space evaluated, it is possible that some of these excipients may in fact enhance LAIV stability in foam dried formulations, but their impact was too small to be clearly identified in this study.
Lead formulations were selected based primarily on process loss and the rate of titer loss during storage at 37°C, weighing storage stability higher than process stability. The number of excipients was also considered, giving preference to formulations with fewer components if stability profiles were similar. While several foam dried formulations demonstrated exceptional stability, FM3, FM18, and FM23x were selected as the lead formulations. In addition to sucrose and gelatin, the plasticizer sorbitol (which was used in selected formulations FM18 and FM23x) appeared to have a benefit. FM3 and FM18 had the best overall combination of process and storage stability with the fewest components. Although a process loss of less than 0.5 log TCID50/ml is generally desirable, FM23x had the best combined stability of the gelatin-free formulations with a process loss of 0.5 log TCID50/ml in the screening study.
Screening of Freeze Dried LAIV Formulations
Five freeze-dried analogs of the foam dried LAIV formulations were manufactured to evaluate whether the drying process itself impacted LAIV stability in the solid-state. The lyophilized versions were designed to have an initial total solids content of approximately 10% (i.e., three-fold lower than the foam formulation), while maintaining similar weight ratios of the excipients. The lower solids content in these formulations is typical for freeze drying as it provides for a more porous solid product, which improves drying efficiency as well as reconstitution time. Subsequently, the process loss and storage stability of the freeze dried formulations were evaluated under accelerated conditions (37°C) for up to 8 weeks. Process loss and storage stability in one select lyophilized analog formulation and in the commercially available freeze-dried LAIV product (NASOVAC™, Serum Institute of India) were similarly studied for comparison with the foam dried formulations in the long-term storage stability study.
After lyophilization, all five formulations appeared to have good cake structure. The residual moisture content ranged from 0.8 to 1.9%wt, which was consistent with typical lyophilized products and was lower than their foam dried counterparts. There was no measureable process loss for three of the formulations, and approximately 0.5-log loss for the other two (Fig. 2). Upon storage at 37°C, the viral titer decreased at an average rate from about 0.4 to 0.6 log TCID50/mL per week across the five formulations. This rate of titer loss is approximately ten-fold higher than observed in the corresponding foam dried formulations. The slowest rate of titer loss was observed for formulation Lyo(FM23x). However, there was also visible cake collapse within 2 weeks for this formulation, whereas no cake collapse was observed with the other formulations. The reason for cake collapse is uncertain; the elevated temperature of storage was apparently above the collapse temperature of the dried formulation, although this was not measured; average moisture content of Lyo(FM23x) was higher (1.6%) relative to other freeze dried formulations, which had less the 1% moisture. Although not superior in all aspects, Lyo(FM18) was selected as the lead formulation for real-time stability testing because of its good physical stability, limited number of excipients, and similarity to one of the lead foam dried formulations to provide a direct drying method comparison.
Screening of Spray Dried Formulations
In the initial screening of 30 excipient combinations, plasticizer technology was applied to stabilize the spray dried formulations, which were then characterized in the same manner as the foam dried formulations. Similar to freeze drying, the solids content of the liquid fed to the spray dryer was one half to one third that of the foam dried formulations. Formulations were screened based their ability to maintain viral potency through the drying process and during storage under accelerated conditions at 37°C. Two lead spray dried formulations were selected and tested for long-term storage stability at 4, 25, and 37°C in a 60 week study.
Spray drying transformed all 30 liquid formulations into fine powders with residual moisture contents between 1 and 5%wt. In general, a moderate process-related reduction in viral titer was observed after spray drying with mean process loss of 0.9 ± 0.5 log TCID50/mL, which trended higher than foam dried formulations.
Viral titer rapidly declined in all spray dried formulations upon storage at 37°C with an average rate of titer loss of 0.7 ± 0.4 log TCID50/mL/wk. For most formulations, vaccine potency dropped below the assay detection limit within 4–6 weeks. This rate of titer loss for all spray dried formulations was significantly faster than that observed with foam dried formulations. There was not a discernible correlation between the residual moisture content in the spray dried powders and process or storage stability. Hence, changes in stability were assumed to be related to changes in formulation composition or process parameters.
On average, formulations containing Pluronic F68 had lower process loss than formulations without (0.8 ± 0.4 versus 1.2 ± 0.4 log TCID50/mL, respectively), suggesting that the surfactant may shield LAIV from destabilizing stresses during the drying process. In contrast to foam dried formulations, gelatin and arginine did not appear to be strong stabilizers, although their inclusion did not reduce stability. Somewhat surprisingly, the inclusion of plasticizers also did not significantly improve LAIV stability in the formulation combinations evaluated in this study. Inclusion of methionine, EDTA, or metal ions had marginal benefit on LAIV stability. Sucrose and trehalose appeared to be comparable stabilizing / bulking agents. Similarly, there was not an obvious benefit of one buffer system over another.
Lead formulations were selected based primarily on process loss and the rate of titer loss during storage at 37°C, weighing storage stability higher than process stability. The number of excipients was also considered, giving preference to formulations with fewer components if stability profiles were similar. Two spray dried formulations, SD18 and SD30, demonstrated the best overall combination of process and storage stability during formulation screening. They differed from the lead foam and freeze dried formulations with the inclusion of trehalose, which acts to increase the glass transition temperature of the resulting solid.
Evaluation of Drying Processes for Long-Term Stability
Lead Foam-Dried Formulations
The three foam dried formulations exhibited a similar level of storage stability (Fig. 3). At 37°C, vaccine potency slowly declined during the first 6 weeks, reducing viral titer by ~0.6-log TCID50/mL in all formulations. At subsequent time points, the viral titer continued to decrease, but at a much slower rate. After 20 week at 37°C, the variability in viral titer for FM23xLTS increased significantly, wherein the titer in some vials was near or below the detection limit of the TCID50 assay while other vials had similar titer to previous time points. This increase in titer variability among samples corresponded with collapsed foam structure in the vials with low titer. A similar increase in variability and collapse of foam structure in a subset of samples was also observed with FM18LTS after 25 weeks at 37°C, but was not observed with FM3LTS. The apparent change in foam structures was not observed in the 25 and 4°C stability samples for any formulation. The observed stability of these formulations at 37°C was comparable with that observed during formulation screening, demonstrating good batch-to-batch repeatability.
At 4 and 25°C, viral titer slowly decreased over the 74 week study (Fig. 3). The change in potency was more pronounced at 25 than at 4°C, as expected. At 25°C, the titer loss approached 1-log TCID50/mL for all three formulations after 48 weeks, but there was little-to-no subsequent loss in titer between the 48 and 72 weeks time points. At 4°C, viral titer declined by approximately 0.5-log after 72 weeks for all formulations.
The rate of titer change during storage was estimated by linear regression for each formulation at each storage temperature. These rates are summarized in Table V. The three foam dried formulations appeared to have similar stability profiles, and were significantly more stable than the formulations prepared by lyophilization (Table VII) or spray drying (Table IX), especially at elevated temperatures. Based on the lower 95% confidence limit for the rate of titer loss, the shelf life for the lead H1N1 foam dried formulations have exceeded the target stability specifications at 37°C (4 weeks) and 25°C (12 weeks) (Table VI). The target shelf life at 4°C (156 weeks) was within the 95% confidence interval for two of the formulations (FM18LTS and FM23xLTS), suggesting that this target could also potentially be achieved by these formulations.
Freeze Dried Formulations
When stored at 37°C, vaccine potency rapidly declined in both freeze dried formulations (Fig. 4). Within 4 weeks, viral titer was reduced by 2.8-log TCID50/mL in Lyo(FM18)LTS and 2.5-log TCID50/mL in NASOVAC™. After 8 weeks, both formulations at 37°C were near the detection limit of the TCID50 assay. Similarly, the potency of the freeze dried formulations at 25°C declined fairly rapidly, losing more than 1.5-log TCID50/mL within 8 weeks. Both formulations showed significantly improved stability when stored at 4°C, exhibiting a slow and steady decline in H1N1 viral titer over time. The potency of NASOVAC™ decreased by approximately 0.5-log after 60 weeks, whereas Lyo(FM18)LTS lost over 1.5-log TCID50/mL during the same period.
The rate of titer change during storage was estimated by linear regression for each formulation at each storage temperature. At 25 and 37°C, regression analysis was limited to the initial phase of rapid titer loss (8 and 4 weeks, respectively) since that region encompassed the defined storage stability limit (1-log reduction in potency). While the two freeze dried formulations had comparable rates of titer loss at 37°C, NASOVAC™ demonstrated superior stability at 4 and 25°C (Table VII). For comparison, the rates of titer loss found here were equivalent to or less than that demonstrated at 25°C by Yannarell et al. (20) for lyophilized formulations of a Type-A strain LAIV.
Based on the lower 95% confidence limit for the rate of titer loss (see Table VIII), neither freeze dried formulation meets the target shelf-life specification at 25 or 37°C (12 and 4 weeks, respectively). However, target specification at 4°C (156 weeks) was currently within the 95% confidence interval of NASOVAC™’s estimated shelf life. Overall, the freeze dried formulations were approximately an order of magnitude less stable than foam dried formulations (Tables V and VI).
Long-term Stability Testing of Spray Dried Formulations
When stored at 37°C, vaccine potency rapidly declined during the first 4 weeks for both formulations, reducing viral titer by 3-log TCID50/mL (Fig. 5). After the first month, the viral titer of SD30LTS appeared to stabilize, but viral titer of SD18LTS fell below the limit of detection. A biphasic reduction in viral titer was also observed for both formulations at 25°C, wherein the viral titer of these formulations was reduced by approximately 2-log TCID50/mL within 8 weeks. The spray dried formulations were much more stable at 4°C, but a slow and steady decline in potency has been observed. After 72 weeks at 4°C, the potency of both formulations had decreased by approximately 1 log TCID50/mL. The stability of these formulations at 37°C was comparable with that observed during formulation screening, demonstrating good batch-to-batch repeatability.
The rate of titer change during storage was estimated by linear regression for each formulation at each storage temperature. At 25 and 37°C, regression analysis was limited to the initial phase of rapid titer loss (8 and 4 weeks, respectively) since that region encompassed the defined storage stability limit (1-log reduction in potency). The two spray dried formulations had comparable rates of titer loss at each storage temperature (Table IX), and were approximately an order of magnitude less stable than foam dried formulations (Table V). Based on the lower 95% confidence limit for the rate of titer loss, neither spray dried formulation achieved the target shelf-life specification at any temperature (Table X).
Comparison of three drying processes for stabilization of LAIV performance
Figure 6 provides a picture of representative stability samples from each drying technology, illustrating the significant differences in the physical form of the final dried product. As can be seen, the larger vial associated with foam drying is needed to provide sufficient head space for the expanded foam.
Figure 7 and Table XI summarize the stability results, which show superior stabilization properties of the foam dried formulation over the other drying approaches across all three storage temperatures, but particularly at 25 and 37°C.
Storage stability at 37°C (a), 25°C (b), and 4°C (c) for H1N1 LAIV formulations manufactured using spray drying (●), foam drying (▼), and freeze drying processes (□), along with a commercial freeze-dried product, NASOVAC™ (◊). Data represents average of three measurements and the error bars the standard deviation.
Figure 8 shows the Arrhenius temperature dependence of the rate of titer loss. The linear dependence of the spray dried and freeze dried formulations is more evident, while the foam dried formulation could be argued to deviate from Arrhenius kinetics, possibly attributable to the closeness of the highest storage temperature (37°C) to the Tg of this formulation.
Immunogenicity
In Vivo Testing in Ferrets
All LAIV formulations exhibited good safety profile. All animals maintained a normal weight and activity level throughout the study. There were no signs of nasal or respiratory distress, or fever associated with any formulation.
All LAIV formulations elicited an immunogenic response after the priming dose. The measured HAI titer in groups receiving the foam dried, freeze dried and spray dried formulations was comparable to the group receiving the frozen LAIV control (Fig. 9). Therefore, it can be concluded that the lead formulations retain complete biological potency. Surprisingly, there was little or no increase in HAI titer after the boosting dose. While the study demonstrated that the dried formulations retained immunogenicity, the resulting HAI titer for all groups (including the control) was lower than predicted by other published studies. Additional dose ranging studies may be necessary to establish the optimum dose.
Application to LAIV Type B
The foam drying process and lead formulations were applied to the LAIV Type-B strain from SII. The TCID50 assay was qualified to measure the potency of LAIV Type-B. Two batches of foam dried LAIV Type-B were manufactured for each formulation. Virus stability through the foam drying process and during storage at 4, 25, and 37°C was assessed using the TCID50 assay. Figure 10 and Table XII show that a lead foam dried formulation applied to a Type-B LAIV strain imparts comparable stabilization to the H1N1 strain. While the addition of gelatin seemed to improve the stabilization of the H1N1 strain, no measurable improvement was observed for the Type-B strain (Table XII).
Discussion
Initial screening of foam dried and spray dried formulations indicated a significant amount of variability in both process loss and accelerated storage stability with different excipient combinations. These results demonstrated the important role excipient selection had on achieving good LAIV stability in the dried state. Arginine and gelatin in foam dried formulations stood out as providing a significant stabilizing effect on the formulations, while for the spray dried formulations no benefit from either gelatin or arginine was noted; instead some improvement in stability with the addition of Pluronic-F68 was observed for the spray dried formulations. These results point to the fact that there are unique excipient/drying method combinations that optimize stability.
Although moisture content of the dried formulations varied (2–5% for foam dried and 1–5% for spray dried) there was no measurable correlation of either process loss or storage stability with moisture content over this range. If there was some stability dependency on moisture content, they were not strong enough for these studies to reveal. In further support of the apparent weak effect of moisture content in this range on stability, the highest moisture content dried product was produced by foam drying, which had greater viral stability than freeze dried product having an order of magnitude lower moisture content. Despite the fact that the moisture content may be correlated with the glass transition temperature of the formulations, higher glass transition temperature was not correlated with improved stability across the different drying methods. A direct comparison of formulation FM18LTS with Lyo(FM18LTS), having essential the same composition in the dried state, illustrates this observation. FM18LTS with 2.9% moisture and Tg of 40.1°C would be expected to have a far inferior stability to Lyo(FM18LTS) with 0.3% moisture and Tg of 48.5°C. Clearly thermal history has far greater impact on stability than the often monitored moisture or Tg. And yet the superior stability performance of the foam dried product at 37°C, only about 3°C below the formulation’s Tg, seems to defy the conventional wisdom with regard to stability in the dried state.
As indicated above, the low specific surface area provided by foam drying may be the factor that is responsible for the improved stability, possibly through reduced air/solid interface exposure for the virus (17). Other factors that could be at play in contributing to this enhanced stabilization have been investigated in other studies, which found correlation between the reduced or dampened molecular motion (both global molecular mobility and the fast dynamics associated with local atomic vibrations) measured in foam dried solids relative to either spray dried or freeze dried solid formulations (21).
With the large number of excipients evaluated in these studies, it is very possible the particular formulations tested here did not include the fully optimized composition. It is also possible there is/are some other excipient(s) that could further improve stability of the formulations. However, given the order of magnitude difference in the stability results for LAIV, it is expected the trend here would be reproduced with regard to the superiority of foam drying over the other methods even with fully optimized formulation compositions. Without the appropriate drying technology, it does not appear possible to reach this marked storage stability improvement with excipient selection alone. Other researchers have made similar findings that thermal history and drying process stresses can have a significant influence on the physicochemical properties of the formulation impacting product stability (22). Comparing similar formulations under foam versus freeze drying clearly demonstrates the sometime dominant role the drying process itself imparts to the formulation’s effective storage stability. Comparison to the stability performance of the commercial freeze dried product NASOVAC™ (with its own level formulation optimization) further demonstrates the superiority of foam drying as process technology, particularly for elevated temperatures.
The LTS studies revealed the thermal stability of both H1N1 and Type-B LAIV strains were significantly enhanced through application of plasticizer technology. The foam dried formulations stood out by providing a significant improvement in the state-of-the-art of solid-stabilized live flu vaccines, potentially rivalling known inactivated or subunit flu vaccine formulations at elevated temperatures (23). The application of this technology to commercial products can expand the access of life-saving vaccines to larger regions of the globe through reduced cold chain requirements. It should be recognized that realizing this potential does have its hurdles in terms of process scale-up (e.g. maintaining container closure integrity against possible formulation splatter during primary drying, homogeneity of moisture within the vial, consistency of product appearance, etc.) (3) in addition to controlling other product properties such as reconstitution time. Clearly developing a robust manufacturing process for a new technology such as foam drying represents a significant challenge. The benefits, however, could very well be worth the effort.
Conclusions
The main finding of this research with regard to solid dosage form stabilization of LAIV is that the choice of drying method has a major impact on stability, despite efforts to similarly optimize the final formulation for the particular drying method. The data indicated an order of magnitude improvement in storage stability shown for foam drying over freeze drying or spray drying when compared across the different formulations tested. Additionally, for a given drying process, the appropriate selection of excipients also plays a significant role in achieving optimal storage stability while minimizing process loss. Although not specifically tested in this study, sensitivity of the stability of the foam dried and spray dried formulations to moisture content between 2 and 5 wt% could not be detected. The superiority of the foam dried formulations existed despite the fact that the freeze dried formulations had an order of magnitude lower moisture content. The optimized formulation composition/dry method combination for the Type-A strain LAIV when applied to a Type-B strain also provided similar benefits in terms of storage stability, indicating the possible wider range applicability of the plasticizer/foam drying technology to other live virus vaccine candidates and even biologics in general.
Notes
The CDC and WHO maintains guidelines on the stability evaluation of vaccines, e.g. http://www.who.int/biologicals/publications/trs/areas/vaccines/stability/en/
Throughout the text, “wet blend” will refer to the fully formulated liquid to be directly spray dried, foam dried or freeze dried into the final product.
Abbreviations
- BARDA:
-
Biomedical advanced research and development authority
- CPE:
-
CytoPathic effect
- DSC:
-
Differential scanning calorimetry
- ECACC:
-
European collection of cell cultures
- HAI:
-
Hemagglutination inhibition
- IEM:
-
Institute of experimental medicine (Russia)
- KF:
-
Karl Fischer titration
- LAIV:
-
Live attenuated influenza vaccine
- LTS:
-
Long term stability
- MDCK:
-
Madin Darby canine kidney cells
- MTT:
-
[3-{4,5-dimethyliazol-yl)-2,5 diphenyltetrazolium bromide] dye
- SII:
-
Serum institute of India
- TCID_50:
-
50% Tissue culture infective dose
- Tg:
-
Glass transition temperature
- WHO:
-
World health organization
References
Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO. World Health Organization (WHO) website. Available at: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2009_11_27/en/index.html. Accessed December 9, 2009.
Homeland Security Council. National Strategy for Pandemic Influenza: Implementation Plan. Homeland Security Council: Washington, DC; 2006. Available at: http://georgewbush-whitehouse.archives.gov/homeland/nspi_implementation.pdf.
Ohtake S, Lechuga-Ballesteros D, Truong-Le V, Patzer EJ. Strategies for heat-stable vaccines. In: Wen EP, Ellis R, Pujar NS, editors. Vaccine Development and Manufacturing. Hoboken: Wiley; 2015.
The Congress of the United States Congressional Budget Office (CBO). Stockpiling vaccine. In: Orszag PR, ed. US Policy Regarding Pandemic-Influenza Vaccines. Washington, DC: CBO; 2008:25–28. Available at: http://www.cbo.gov/ftpdocs/95xx/doc9573/Chapter4.8.1.shtml.
The Department of Health and Human Services (DHHS). Pandemic Influenza Preparedness Spending. Washington, DC: HHS; 2009. Available at: http://www.hhs.gov/aspr/barda/mcm/panflu/hhspanflu-spending-0901.pdf.
Dormitzer PR, Mandl CW, Rappuoli R. Replicating Vaccines: A New Generation. Basel: Springer; 2011.
Kumru OS, Joshi SB, Smith DE, Middaugh CR, Prusik T, Volkin DB. Vaccine instability in the cold chain: Mechanisms, analysis and formulation strategies. Biologicals. 2014;42:237–59.
Cicerone MT, Tellington A, Trost L, Sokolov A. Plasticized Hydrophilic Glasses for Improved Stabilization of Biological Agents. US Patent. 2006;7:101,693.
Cicerone MT, Tellington A, Trost L, Sokolov A. Substantially improved stability of biological agents in dried form. BioProc Int. 2003;1:36–47.
Cicerone MT, Soles CL, Chowdhuri Z, Pikal MJ, Chang L. Fast dynamics as a diagnostic for excipients in preservation of dried proteins. Am Pharm Rev. 2005;8(6):22–7.
Abdul-Fattah AM, Truong-Le V, Yee L, Pan E, Ao Y, Kalonia DS, et al. Drying-induced variations in physico-chemical properties of amorphous pharmaceuticals and their impact on Stability II: stability of a vaccine. Pharm Res. 2007;24(4):715–27.
Ohtake S, Martin RA, Yee L, Chen D, Kristensen DD, Lechuga-Ballesteros D, et al. Heat-Stable Measles Vaccine Produced By Spray Drying. Vaccine. 2009;28:1275–84.
Truong-Le V, Ohtake S, Lechuga-Ballesteros D, Martin RA, Pham BV, Saxena A, Chiueh G. Formulation for Room Temperature Stabilization of a Live Attenuated Bacterial Vaccine. Patent WO 2011/032108. 2011.
Ohtake S, Truong-Le V, Yee L, Martin RA, Lechuga-Ballesteros D. Methods and Compositions for Stabilization of a Virus Vaccine. US Patent US 2011/0243988. 2011.
Truong-Le V, Yee L, Lechuga-Ballesteros D, Ohtake S. Formulations for preservation of rotavirus. US Patent US. 2012;8241886.
Maa YF, Ameri M, Shu C, Payne LG, Chen D. Influenza Vaccine Powder Formulation Development: Spray-Freeze-Drying and Stability Evaluation. J Pharm Sci. 2004;93(7):1912–23.
Truong-Le V, Abdul-Fattah AM. The impact of formulation and drying processes on the characteristics and performance of biopharmaceutical powders. In: Jameel F, Hershenson S, editors. Formulation and Process Development Strategies for Manufacturing Biopharmaceuticals. Hoboken: Wiley; 2010.
Truong-Le V, Ohtake S, Martin RA, Pham BV, Yee L. Sonic Low Pressure Spray Drying. US Patent. 2014;8:673,357.
Payment P, Trudel M. Methods and Techniques in Virology. New York: Marcel Dekker; 1993.
Yannarell DA, Goldberg KM, Hjorth RN. Stabilizing cold-adapted influenza virus vaccine under various storage conditions. J Virol Methods. 2002;102:15–25.
Abdul-Fattah AM, Truong-Le V, Yee L, Nguyen L, Kalonia DS, Cicerone MT, et al. Drying-induced variations in physico-chemical properties of amorphous pharmaceuticals and their impact on Stability I: stability of a monoclonal antibody. J Pharm Sci. 2007;96:1983–2008.
Abdul-Fattah AM, Kalonia DS, Pikal MJ. The challenge of drying method selection for protein pharmaceuticals: product quality implications. J Pharm Sci. 2007;96(8):1886–916.
Amorij J-P, Huckriede A, Wilschut J, Frijlink HW, Hinrichs WLJ. Development of Stable Influenza Vaccine Powder Formulations: Challenges and Possibilities. Pharm Res. 2008;25(6):1256–73.
ACKNOWLEDGMENTS AND DISCLOSURES
This work was funded by PATH. The authors would also like to gratefully acknowledge Dr. Alex Flood and Dr. Dexiang Chen of PATH for their contributions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lovalenti, P.M., Anderl, J., Yee, L. et al. Stabilization of Live Attenuated Influenza Vaccines by Freeze Drying, Spray Drying, and Foam Drying. Pharm Res 33, 1144–1160 (2016). https://doi.org/10.1007/s11095-016-1860-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-016-1860-1