Abstract
Purpose
To build a physiologically based pharmacokinetic model describing drug kinetics in interstitial fluid in case of hemorrhagic shock, and to propose a simple method to determine the subset of influential parameters that may be estimated with the data at hand.
Methods
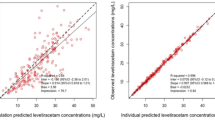
The model, which accounts for alterations of regional blood flows and body water distribution, was fitted to amoxicillin and clavulanate kinetic data, assessed in 12 trauma patients with hemorrhagic shock by comparison with 12 healthy volunteers. The predictions were the free concentrations of amoxicillin and clavulanate in 14 organs.
Results
In all tissues of trauma patients, the rate of distribution was lower, but the steady-state level was higher than those in healthy participants. Blood volume was reduced by 25% and blood flow in organs other than lung, brain, and heart were reduced by 18%. Compared with healthy subjects, the time that free amoxicillin concentration remained above 8 mg/L in the interstitial fluid of trauma patients was higher in blood and muscles, and lower in the tendon compartment.
Conclusions
The results and predictions were consistent with the knowledge in this field. The model may be useful to optimize clinical trial designs and drug dosing regimens.



Similar content being viewed by others
REFERENCES
T. D. Egan, S. Kuramkote, G. Gong, J. Zhang, S. W. McJames, and P. L. Bailey. Fentanyl pharmacokinetics in hemorrhagic shock: a porcine model. Anesthesiology 91:156–166 (1999).
K. B. Johnson, S. E. Kern, E. A. Hamber, S. W. McJames, K. M. Kohnstamm, and T. D. Egan. Influence of hemorrhagic shock on remifentanil: A pharmacokinetic and pharmacodynamic analysis. Anesthesiology 94:322–332 (2001).
K. B. Johnson, T. D. Egan, J. Layman, S. E. Kern, J. L. White, and S. W. McJames. The influence of hemorrhagic shock on etomidate: A pharmacokinetic and pharmacodynamic analysis. Anesth. Analg. 96:1360–1368 (2003).
K. B. Johnson, T. D. Egan, S. E. Kern, J. L. White, S. W. McJames, N. Syroid, D. Whiddon, and T. Church. The influence of hemorrhagic shock on propofol: A pharmacokinetic and pharmacodynamic analysis. Anesthesiology 99:409–420 (2003).
T. Kazama, K. Ikeda, K. Morita, T. Ikeda, M. Kikura, S. Sato. Relation between initial blood distribution volume and propofol induction dose requirement. Anesthesiology 94:205–210 (2001).
T. Kurita, K. Morita, T. Kazama, and S. Sato. Influence of cardiac output on plasma propofol concentrations during constant infusion in swine. Anesthesiology 96:1498–1503 (2002).
R. N. Upton, G. L. Ludbrook, C. Grant, and A. M. Martinez. Cardiac output is a determinant of the initial concentrations of propofol after short-infusion administration. Anesth. Analg. 89:545–552 (1999).
A. R. Edouard, A. C. Degremont, J. Duranteau et al. Heterogeneous regional vascular responses to simulated transient hypovolemia in man. Intensive Care Med. 20:414–420 (1994).
W. C. Schoemaker. Circulatory mechanisms of shock and their mediators. Crit. Care Med. 15:787–794 (1987).
S. L. Shafer. Shock values. Anesthesiology 101:567–568 (2004).
K. B. Johnson, T. D. Egan, S. E. Kern, M. L. Cluff, and N. L. Pace. Influence of hemorrhagic shock followed by crystalloid resuscitation on propofol: A pharmacokinetic and pharmacodynamic analysis. Anesthesiology 101:647–659 (2004).
S. Bjorkman, D. R. Wada, and D. R. Stanski. Application of physiologic models to predict the influence of changes in body composition and blood flows on the pharmacokinetics of fentanyl and alfentanil in patients. Anesthesiology 88(3):657–667 (1998).
D. R. Wada, S. Bjorkman, W. F. Ebling, H. Harashima, S. R. Harapat, and D. R. Stanski. Computer simulation of the effects of alterations in blood flows and body composition on thiopental pharmacokinetics in humans. Anesthesiology 87(4):884–899 (1997).
R. N. Upton, and G. Ludbrook. A physiologically based, recirculatory model of the kinetics and dynamics of propofol in man. Anesthesiology 103(2):344–352 (2005).
F. Lagneau, J. Marty, P. Beyne, and M. Tod. Pharmacokinetic evaluation of the french recommended protocol for antibioprophylaxis during liver surgery: A physiological modeling approach. J. Pharmacokinet. Pharmacodyn. 32(1):1–32 (2005).
O. Mimoz, V. Schaeffer, P. Incagnoli, K. Louchahi, A. Edouard, O. Petitjean, and M. Tod. Co-amoxiclav pharmacokinetics during post-traumatic hemorrhagic shock. Crit. Care Med. 29:1350–1355 (2001).
D. G. Levitt. The pharmacokinetics of the interstitial space in humans. BMC Clin. Pharmacol. 3:3 (2003).
D. Z. D’Argenio, and A. Schumitzky. ADAPT II User’s Guide: Pharmacokinetic/Pharmacodynamic Systems Analysis Software. Biomedical Simulations Resource, Los Angeles, 1997.
C. C. Gyenge, O. Tenstad, and H. Wiig. In vivo determination of steric and electrostatic exclusion of albumin in rat skin and skeletal muscle. J. Physiol. 552(Pt 3):907–916 (2003).
D. Gallagher, M. Visser, D. Sepulveda, R. N. Pierson, T. Harris, and S. B. Heymsfield. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am. J. Epidemiol. 143:228–239 (1996).
G. Gutierrez, H. D. Reines, and M. E. Wulf-Gutierrez. Clinical review: hemorrhagic shock. Crit. Care 8(5):373–381 (2004).
D. Z. D’Argenio, A. Schumitzky, and W. Wolf. Simulation of linear compartment models with application to nuclear medicine kinetic modeling. Comput. Methods Programs Biomed. 27(1):47–54 (1988).
Société Française d’Anesthésie et de Réanimation. Consensus conference. “Antibioprophylaxis in a surgical setting.” 10–11 December 1992, Faculté de Médecine Xavier Bichat. Cah. Anesthesiol. 41:273–280 (1993).
M. Foulstone, and C. Reading. Assay of amoxicillin and clavulanic acid in biological fluids with high-performance liquid chromatography. Antimicrob. Agents Chemother. 22:753–776 (1982).
P. Leroy, C. Gavriloff, A. Nicolas, et al. Comparative assay of amoxicillin by high-performance liquid chromatography and microbiological methods for pharmacokinetic studies in calves. Int. J. Pharm. 82:157–164 (1992).
D. Andes, and W. A. Craig. In vivo activities of amoxicillin and amoxicillin-clavulanate against Streptococcus pneumoniae: application to breakpoint determinations. Antimicrob. Agents Chemother. 42(9):2375–2379 (1998).
S. Bronner, V. Murbach, J. D. Peter, D. Leveque, H. Elkhaili, Y. Salmon, N. Dhoyen, H. Monteil, G. Woodnutt, and F. Jehl. Ex vivo pharmacodynamics of amoxicillin-clavulanate against beta-lactamase-producing Escherichia coli in a yucatan miniature pig model that mimics human pharmacokinetics. Antimicrob. Agents Chemother. 46(12):3782–3789 (2002).
S. Bronner, D. Pompei, H. Elkhaili, N. Dhoyen, H. Monteil, and F. Jehl. Ex vivo 12 h bactericidal activity of oral co-amoxiclav (1.125 g) against beta-lactamase-producing Haemophilus influenzae. J. Antimicrob. Chemother. 48(4):501–506 (2001).
R. Kawai, D. Mathew, C. Tanaka, and M. Rowland. Physiologically based pharmacokinetics of cyclosporine A: extension to tissue distribution kinetics in rats and scale-up to human. J. Pharmacol. Exp. Ther. 287(2):457–468 (1998).
I. A. Nestorov, L. J. Aarons, P. A. Arundel, and M. Rowland. Lumping of whole-body physiologically based pharmacokinetic models. J. Pharmacokinet. Biopharm. 26(1):21–46 (1998).
A. P. MacGowan, A. R. Noel, C. A. Rogers, and K. E. Bowker. Antibacterial effects of amoxicillin-clavulanate against Streptococcus pneumoniae and Haemophilus influenzae strains for which MICs are high, in an in vitro pharmacokinetic model. Antimicrob. Agents Chemother. 48(7):2599–2603 (2004).
L. Heinemann. Glucose Monitoring Study Group: Continuous glucose monitoring by means of the microdialysis technique: Underlying fundamental aspects. Diabetes Technol. Ther. 5:545–561 (2003).
S. H. Khan, and A. Shuaib. The technique of intracerebral microdialysis. Methods 23:3–9 (2001).
D. E. Nix, S. D. Goodwin, C. A. Peloquin, D. L. Rotella, and J. J. Schentag. Antibiotic tissue penetration and its relevance: models of tissue penetration and their meaning. Antimicrob. Agents Chemother. 35(10):1947–1952 (1991).
D. E. Nix, S. D. Goodwin, C. A. Peloquin, D. L. Rotella, and Schentag. Antibiotic tissue penetration and its relevance: impact of tissue penetration on infection response. Antimicrob. Agents Chemother. 35(10):1953–1959 (1991).
M. Brunner, O. Langer, G. Dobrozemsky, U. Muller, M. Zeitlinger, M. Mitterhauser, W. Wadsak, R. Dudczak, K. Kletter, and M. Muller. [18F]Ciprofloxacin, a new positron emission tomography tracer for noninvasive assessment of the tissue distribution and pharmacokinetics of ciprofloxacin in humans. Antimicrob. Agents Chemother. 48(10):3850–3857 (2004).
Author information
Authors and Affiliations
Corresponding author
Additional information
Sources of financial support: EA3738, université Lyon 1, Lyon, F-69003, France
Work attributed to: Université de Lyon, Lyon, F-69003, France; université Lyon 1, ISPB, Lyon, F-69008, France
Appendix: Equations of the Model
Appendix: Equations of the Model
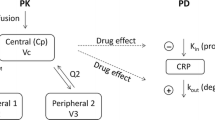
Base Model
A description of the model equations is presented here. More details and explainations may be found in the article of Levitt (17). The model is written as set of differential equations. Each equation describes the variation of the free drug concentration in the interstitial fluid of an organ (compartment). Each organ i is characterized by its mass Vi (kg), extracellular water fraction wecfi (L/kg), ratio of interstitial to plasma albumin concentration rcPi, permeability–surface area product PSi for free drug (L/min per kg of organ), and blood flow Qi (L/min per kg of organ).
The unbound fraction of drug in the volume of interstitial fluid (assimilated to the EDTA space) of each organ, fuTi, is calculated as :
where Kass is the association constant for drug binding to albumin measured in plasma (L/mol), Prot is albumin concentration in plasma (mol/L), and αi is the fraction of EDTA interstitial space accessible to the drug in organ i. This parameter allows to take into account steric of electrostatic exclusion of the drug from the interstitial space.
In case of permeability-limited diffusion of the drug into the interstitial space of an organ, the fraction of the arterial drug concentration that diffuses into interstitial fluid during a single pass is calculated as:
where fub is the free fraction of drug in the blood, wecfb the water fraction of blood in L/kg, and 1.06 is the density of blood in kilograms per liter.
The rate constant for free drug diffusion from blood to interstitial space of each organ, in 1/min, is calculated as:
This equation may be viewed as the ratio of an unbound drug distribution clerarance \(1.06{\text{wecf}}_{\text{b}} \cdot {\text{Q}}_{\text{i}} \cdot {{{\text{V}}_{\text{i}} } \mathord{\left/ {\vphantom {{{\text{V}}_{\text{i}} } {{\text{fu}}_{\text{b}} }}} \right. \kern-\nulldelimiterspace} {{\text{fu}}_{\text{b}} }}\) to an unbound drug volume of distribution \({\text{V}}_{\text{i}} \cdot {{{\text{wecf}}_{\text{i}} } \mathord{\left/ {\vphantom {{{\text{wecf}}_{\text{i}} } {{\text{fu}}_{{\text{Ti}}} }}} \right. \kern-\nulldelimiterspace} {{\text{fu}}_{{\text{Ti}}} }}\)
The generic equation describing the variation of the free drug concentration in the interstitial fluid of an organ (CuTi) is:
where CuA is the free drug concentration in arterial blood, and ke is an elimination rate constant, if any. This rate constant is calculated as the ratio of an unbound drug elimination clerarance (\(1.06\;{\text{wecf}}_{\text{b}} \cdot {{{\text{CLi}}} \mathord{\left/ {\vphantom {{{\text{CLi}}} {{\text{fu}}_{\text{b}} }}} \right. \kern-\nulldelimiterspace} {{\text{fu}}_{\text{b}} }}\)) to an unbound drug volume of distribution (\({\text{V}}_{\text{i}} \cdot {{{\text{wecf}}_{\text{i}} } \mathord{\left/ {\vphantom {{{\text{wecf}}_{\text{i}} } {{\text{fu}}_{{\text{Ti}}} }}} \right. \kern-\nulldelimiterspace} {{\text{fu}}_{{\text{Ti}}} }}\)). CLi is the intrinsic clearance of total drug, related to the organ clearance CLorg by a clearance model. In the simple case of a well mixed model, the relationship is:
The tissue-to-plasma total drug concentration ratios (Kpi) are calculated as:
where 0.94 is the water fraction of plasma in liters per kilogram.
The volume of distribution of total drug at steady-state is calculated as:
where Vp is the volume of water in plasma, λE is the fraction of interstitial volume (EDTA space) accessible to albumin (λE = 0.45), and the sum is over the n organs.
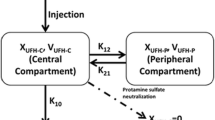
Characterization of Hemorrhagic Shock and Fluid Resuscitation
The following changes are made to the base model. The volumes (Vi) of venous and arterial blood are multiplied by the factor of variation of blood volume (fbl). The extracellular water fractions (wecfi) are multiplied by the factor of variation of the water fraction of blood fwbl (venous and arterial blood) or the factor of variation of extracellular water volume fecw (other tissues). The ratios of albumin concentration (rcPi) are multiplied by a factor fwbl/fecw. The blood flows (Qi) are multiplied by the factor of reduction of blood flow (fq) in all organs except brain, heart, and lung.
Rights and permissions
About this article
Cite this article
Tod, M., Lagneau, F., Jullien, V. et al. A Physiological Model to Evaluate Drug Kinetics in Patients with Hemorrhagic Shock Followed by Fluid Resuscitation. Pharm Res 25, 1431–1439 (2008). https://doi.org/10.1007/s11095-008-9546-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-008-9546-y