Abstract
Purpose
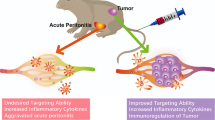
To assess in vivo macrophage targeting potential of PEG-fMLF nanocarriers and to investigate their biodistribution, peritoneal macrophage uptake, and pharmacokinetics.
Methods
Multiple copies of fMLF were conjugated to purchased and novel (branched, peptide-based) PEG nanocarriers. Peritoneal macrophage uptake was evaluated in mice 4 hours after IP administration of fluorescence-labeled PEG-fMLF nanocarriers. Pharmacokinetics and biodistribution were determined in rats after IV administration of tritiated PEG-fMLF nanocarriers.
Results
Attachment of one, two, or four fMLF copies increased uptake in macrophages by 3.8-, 11.3-, and 23.6-fold compared to PEG without fMLF. Pharmacokinetic properties and tissue distribution also differed between nanocarriers with and without fMLF. Attachment of fMLF residues increased the t1/2 of PEG5K by threefold but decreased the t1/2 of PEG20K by 40%. Attachment of fMLF increased accumulation of nanocarriers into macrophages of liver, kidneys and spleen. However, on a molar basis, penetration was equivalent suggesting nanocarrier size and targeting moieties are important determinants.
Conclusions
These results demonstrate the feasibility for targeting macrophages, a primary HIV reservoir site. However, these studies also suggest that balancing peripheral tissue penetration (a size-dependent phenomenon) versus target cell uptake specificity remains a challenge to overcome.






Similar content being viewed by others
References
A. M. Vandamme, K. Van Vaerenbergh, and E. De Clercq. Anti-human immunodeficiency virus drug combination strategies. Antivir. Chem. Chemother. 9:187–203 (1998).
D. R. Bangsberg, F. M. Hecht, E. D. Charlebois, A. R. Zolopa, M. Holodniy, L. Sheiner, J. D. Bamberger, M. A. Chesney, and A. Moss. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS 14:357–366 (2000).
L. K. Schrager and M. P. D’Souza. Cellular and anatomical reservoirs of HIV-1 in patients receiving potent antiretroviral combination therapy. JAMA 280:67–71 (1998).
D. D. Richman. HIV chemotherapy. Nature 410:995–1001 (2001).
R. Langer. Drug delivery and targeting. Nature 392:5–10 (1998).
R. Langer. Drug delivery. Drugs on target. Science 293:58–59 (2001).
V. P. Torchilin. Drug targeting. Eur. J. Pharm. Sci. 11(Suppl 2):S81–S91 (2000).
H. Schuitemaker, N. A. Kootstra, R. E. de Goede, F. de Wolf, F. Miedema, and M. Tersmette. Monocytotropic human immunodeficiency virus type 1 (HIV-1) variants detectable in all stages of HIV-1 infection lack T-cell line tropism and syncytium-inducing ability in primary T-cell culture. J. Virol. 65:356–363 (1991).
S. Aquaro, R. Calio, J. Balzarini, M. C. Bellocchi, E. Garaci, and C. F. Perno. Macrophages and HIV infection: therapeutical approaches toward this strategic virus reservoir. Antiviral Res. 55:209 (2002).
F. Ahsan, I. P. Rivas, M. A. Khan, and A. I. Torres Suarez. Targeting to macrophages: role of physicochemical properties of particulate carriers—liposomes and microspheres—on the phagocytosis by macrophages. J. Control Release. 79:29–40 (2002).
T. Igarashi, C. R. Brown, Y. Endo, A. Buckler-White, R. Plishka, N. Bischofberger, V. Hirsch, and M. A. Martin. Macrophage are the principal reservoir and sustain high virus loads in rhesus macaques after the depletion of CD4+ T cells by a highly pathogenic simian immunodeficiency virus/HIV type 1 chimera (SHIV): Implications for HIV-1 infections of humans. Proc. Natl. Acad. Sci. U S A 98:658 (2001).
D. Marras, L. A. Bruggeman, F. Gao, N. Tanji, M. M. Mansukhani, A. Cara, M. D. Ross, G. L. Gusella, G. Benson, V. D. D’Agati, B. H. Hahn, M. E. Klotman, and P. E. Klotman. Replication and compartmentalization of HIV-1 in kidney epithelium of patients with HIV-associated nephropathy. Nat. Med. 8:522–526 (2002).
R. W. Price, B. Brew, J. Sidtis, M. Rosenblum, A. C. Scheck, and P. Cleary. The brain in AIDS: central nervous system HIV-1 infection and AIDS dementia complex. Science 239:586–592 (1988).
D. D. Ho, T. R. Rota, R. T. Schooley, J. C. Kaplan, J. D. Allan, J. E. Groopman, L. Resnick, D. Felsenstein, C. A. Andrews, and M. S. Hirsch. Isolation of HTLV-III from cerebrospinal fluid and neural tissues of patients with neurologic syndromes related to the acquired immunodeficiency syndrome. N. Engl. J. Med. 313:1493–1497 (1985).
J. Stebbing, B. Gazzard, and D. C. Douek. Where does HIV live? N. Engl. J. Med. 350:1872–1880 (2004).
S. M. Crowe and S. Sonza. HIV-1 can be recovered from a variety of cells including peripheral blood monocytes of patients receiving highly active antiretroviral therapy: a further obstacle to eradication. J. Leukoc. Biol. 68:345–350 (2000).
S. Sonza, H. P. Mutimer, R. Oelrichs, D. Jardine, K. Harvey, A. Dunne, D. F. Purcell, C. Birch, and S. M. Crowe. Monocytes harbour replication-competent, non-latent HIV-1 in patients on highly active antiretroviral therapy. AIDS 15:17–22 (2001).
S. Pooyan, B. Qiu, M. M. Chan, D. Fong, P. J. Sinko, M. J. Leibowitz, and S. Stein. Conjugates bearing multiple formyl-methionyl peptides display enhanced binding to but not activation of phagocytic cells. Bioconjug. Chem. 13:216–223 (2002).
E. R. Prossnitz and R. D. Ye. The N-formyl peptide receptor: a model for the study of chemoattractant receptor structure and function. Pharmacol. Ther. 74:73–102 (1997).
B. Burke and C. E. Lewis. The macrophage. Oxford University Press, Oxford, New York, 2002.
B. Vernon-Roberts. The macrophage. University Press, Cambridge [Eng.], 1972.
P. C. Leijh, T. L. van Zwet, M. N. ter Kuile, and R. van Furth. Effect of thioglycolate on phagocytic and microbicidal activities of peritoneal macrophages. Infect. Immun. 46:448–452 (1984).
S. Maesaki. Drug delivery system of anti-fungal and parasitic agents. Curr. Pharm. Des. 8:433–440 (2002).
A. Kozlowski and J. M. Harris. Improvements in protein PEGylation: pegylated interferons for treatment of hepatitis C. J. Control. Release 72:217–224 (2001).
J. M. Harris, N. E. Martin, and M. Modi. Pegylation: a novel process for modifying pharmacokinetics. Clin. Pharmacokinet. 40:539–551 (2001).
A. Kozlowski, S. A. Charles, and J. M. Harris. Development of pegylated interferons for the treatment of chronic hepatitis C. BioDrugs 15:419–429 (2001).
C. D. Conover, R. B. Greenwald, A. Pendri, C. W. Gilbert, and K. L. Shum. Camptothecin delivery systems: enhanced efficacy and tumor accumulation of camptothecin following its conjugation to polyethylene glycol via a glycine linker. Cancer Chemother. Pharmacol. 42:407–414 (1998).
R. B. Greenwald. PEG drugs: an overview. J. Control. Release 74:159–171 (2001).
R. B. Greenwald, Y. H. Choe, J. McGuire, and C. D. Conover. Effective drug delivery by PEGylated drug conjugates. Adv. Drug Deliv. Rev. 55:217–250 (2003).
M. J. Roberts, M. D. Bentley, and J. M. Harris. Chemistry for peptide and protein PEGylation. Adv. Drug Deliv. Rev. 54:459–476 (2002).
P. Caliceti and F. M. Veronese. Pharmacokinetic and biodistribution properties of poly(ethylene glycol)-protein conjugates. Adv. Drug Deliv. Rev. 55:1261–1277 (2003).
J. M. Harris. Poly(ethylene glycol) chemistry: biotechnical and biomedical applications. Plenum, New York, 1991.
M. R. Sherman, L. D. Williams, M. C. P. Saifer, J. A. French, L. W. Kwak, and J. J. Oppenheim. Conjugation of high, molecular weight poly(ethylene glycol) to cytokines: granulocyte-macrophage colony stimulating factors as model substrates. ACS, Washington, DC, 1997.
P. Caliceti, O. Schiavon, and F. M. Veronese. Biopharmaceutical properties of uricase conjugated to neutral and amphiphilic polymers. Bioconjug. Chem. 10:638–646 (1999).
I. L. Koumenis, Z. Shahrokh, S. Leong, V. Hsei, L. Deforge, and G. Zapata. Modulating pharmacokinetics of an anti-interleukin-8 F(ab′)(2) by amine-specific PEGylation with preserved bioactivity. Int. J. Pharm. 198:83–95 (2000).
F. M. Veronese, P. Caliceti, and O. Schiavon. Branched and linear poly(ethylene glycol): Influence of the polymer structure on enzymological, pharmacokinetic, and immunological properties of protein conjugates. J. Bioact. Compat. Polym. 12:196–207 (1997).
C. Monfardini, O. Schiavon, P. Caliceti, M. Morpurgo, J. M. Harris, and F. M. Veronese. A branched monomethoxypoly(ethylene glycol) for protein modification. Bioconjug. Chem. 6:62–69 (1995).
S. Crowe, T. Zhu, and W. A. Muller. The contribution of monocyte infection and trafficking to viral persistence, and maintenance of the viral reservoir in HIV infection. J. Leukoc. Biol. 74:635 (2003).
J. Hu, H. Liu, and L. Wang. Enhanced delivery of AZT to macrophages via acetylated LDL. J. Control. Release 69:327–335 (2000).
Acknowledgements
This work was supported by grants AI 33789 and AI 51214 from National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wan, L., Pooyan, S., Hu, P. et al. Peritoneal Macrophage Uptake, Pharmacokinetics and Biodistribution of Macrophage-Targeted PEG-fMLF (N-Formyl-Methionyl-Leucyl-Phenylalanine) Nanocarriers for Improving HIV Drug Delivery. Pharm Res 24, 2110–2119 (2007). https://doi.org/10.1007/s11095-007-9402-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-007-9402-5