No Heading
Purpose.
We propose a novel method to evaluate the efficacy of a pressurized metered dose inhaler (pMDI) in combination with a spacer, by not only considering the total dose extractable from the spacer but also the dependence of dose on the volume available for aerosol inhalation.
Methods.
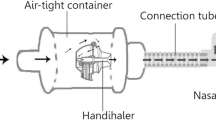
We studied volume-dependence of aerosol concentration during extraction from two commonly used plastic spacers (150 ml AerochamberPlus; 750 ml Volumatic) after a single puff of a 100 μg salbutamol pMDI (HFA-Ventolin), using laser photometric measurements.
Results.
After a delay of 1s in each spacer, the aerosol peak dose for AerochamberPlus was 2-fold that for Volumatic (p < 0.001), with the peak appearing well within the first 0.5 L even for the largest spacer. The opposite dose relationship is reached when considering total cumulative dose, which was 2-fold higher for Volumatic than for AerochamberPlus (p < 0.001); >95% of total cumulative dose was extracted well within 3 L for the largest spacer. The 2-fold cumulative dose relationship was confirmed by chemical assay on an absolute filter [AerochamberPlus: 21.4 ± 3.2 (SD) μg; Volumatic: 43.8 ± 9.1 (SD) μg].
Conclusions.
Actual aerosol dose available to patients during inhalation via spacers can only be done on the basis of a quantification of aerosol peak dose and cumulative dose as a function of extracted volume.
Similar content being viewed by others
References
1. P. W. Barry and C. O’Callaghan. In vitro comparison of the amount of salbutamol available for inhalation from different formulations used with different spacer devices. Eur. Respir. J. 10:1345–1348 (1997).
2. W. D. Bennett, J. S. Brown, K. L. Zeman, S. C. Hu, G. Scheuch, and K. Sommerer. Targeting delivery of aerosols to different lung regions. J. Aerosol Med. 15:179–188 (2002).
3. J. B. West. Respiratory Physiology: The Essentials. Lippincott Williams & Wilkins, Philadelphia, 2000.
4. J. P. Mitchell, M. W. Nagel, and J. L. Rau. Performance of large-volume versus small volume holding chambers with chlorofluorocarbon-albuterol and hydrofluoroalkane-albuterol sulfate. Respir. Care 44:38–44 (1999).
5. J. H. Wildhaber, M. J. Hayden, N. D. Dore, S. G. Devadason, and P. N. LeSouef. Salbutamol delivery from a hydrofluoroalkane pressurized metered-dose inhaler in pediatric ventilator circuits: an in vitro study. Chest 113:186–191 (1998).
6. J. H. Wildhaber, S. G. Devadason, E. Eber, M. J. Hayden, M. L. Everard, Q. A. Summers, and P. N. LeSouef. Effect of electrostatic charge, flow, delay and multiple actuations on the in vitro delivery of salbutamol from different small volume spacers for infants. Thorax 51:985–988 (1996).
7. F. Pierart, J. H. Wildhaber, I. Vrancken, S. G. Devadason, and P. N. Le Souef. Washing plastic spacers in household detergent reduces electrostatic charge and greatly improves delivery. Eur. Respir. J. 13:673–678 (1999).
8. E. Berg. In vitro properties of pressurized metered dose inhalers with and without spacer devices. J. Aerosol Med. 8(Suppl 3):S3–10 (1995).
9. M. J. Clarke, J. Peart, S. Cagnani, and P. R. Byron. Adhesion of powders for inhalation: an evaluation of drug detachment from surfaces following deposition from aerosol streams. Pharm. Res. 19:322–329 (2002).
10. J. H. Wildhaber, S. G. Devadason, M. J. Hayden, R. James, A. P. Dufty, R. A. Fox, Q. A. Summers, and P. N. LeSouef. Electrostatic charge on a plastic spacer device influences the delivery of salbutamol. Eur. Respir. J. 9:1943–1946 (1996).
11. E. Dompeling, A. M. Oudesluys-Murphy, H. M. Janssens, W. Hop, J. G. Brinkman, R. N. Sukhai, and J. C. de Jongste. Randomised controlled study of clinical efficacy of spacer therapy in asthma with regard to electrostatic charge. Arch. Dis. Child. 4:178–182 (2001).
12. J. Heyder. Gravitational deposition of aerosol particles within a system of randomly oriented tubes. Aerosol Sci. 6:133–137 (1976).
13. H. Bisgaard, J. Anhoj, B. Klug, and E. Berg. A non-electrostatic spacer for aerosol delivery. Arch. Dis. Child. 73:226–230 (1995).
14. E. Berg, J. Madsen, and H. Bisgaard. In vitro performance of three combinations of spacers and pressurized metered dose inhalers for treatment in children. Eur. Respir. J. 12:472–476 (1998).
15. C. O’Callaghan, J. Lynch, M. Cant, and C. Robertson. Improvement in sodium cromoglycate delivery from a spacer device by use of an antistatic lining, immediate inhalation, and avoiding multiple actuations of drug. Thorax 48:603–606 (1993).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Verbanck, S., Vervaet, C., Schuermans, D. et al. Aerosol Profile Extracted from Spacers as a Determinant of Actual Dose. Pharm Res 21, 2213–2218 (2004). https://doi.org/10.1007/s11095-004-7673-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-004-7673-7