Abstract
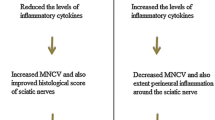
Diabetic neuropathy is one of the common complications of type 2 diabetes mellitus (T2DM) with severe outcomes. The mechanisms of physiopathology of diabetic neuropathy are not well elucidated. Inflammation and inflammatory macrophages are recognized to be crucial in diabetic neuropathy. Toll-like receptor 2 (TLR2) is an important factor in innate immune response which could promote the polarization of inflammatory macrophages. In present study, we evaluated the effects of a TLR2 antagonist CU-CPT22 on diabetic neuropathy. We induced T2DM in mice by feeding with high fat diet (HFD). We measured the body weight, blood glucose level, paw withdrawal threshold, inflammatory cytokine production, and macrophages infiltration in T2DM mice. We evaluated the effects of CU-CPT22 on pro-inflammatory cytokines production, macrophage marker expression in lipopolysaccharides (LPS)-treated BMDMs. We administrated CU-CPT22 in T2DM mice and measured the pro-inflammatory cytokines levels, expression of macrophages markers in sciatic nerve (SCN), and paw withdrawal threshold. T2DM mice had significantly increased body weight and blood glucose, and had significantly decreased paw withdrawal threshold. Obvious increased pro-inflammatory cytokine level and infiltration of M1 phenotype macrophages was observed in SCN from T2DM mice. CU-CPT22 prevented pro-inflammatory cytokine production in LPS-treated BMDMs and re-polarized them to M2 phenotype. CU-CPT22 suppressed the inflammation and induced M2 macrophages in SCN from T2DM mice, and ameliorated the paw withdrawal threshold in T2DM mice. CU-CPT22 ameliorates neuropathic pain in T2DM by promoting M2 phenotype macrophages.




Similar content being viewed by others
Data Availability
Data will be made available on reasonable request.
References
Boulton AJ, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, Malik RA, Maser RE, Sosenko JM, Ziegler D, American Diabetes A (2005) Diabetic neuropathies: a statement by the American Diabetes Association. Diabetes Care 28:956–962
Selvin E, Parrinello CM, Sacks DB, Coresh J (2014) Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med 160:517–525
Donath MY, Shoelson SE (2011) Type 2 diabetes as an inflammatory disease. Nat Rev Immunol 11:98–107
Pop-Busui R, Ang L, Holmes C, Gallagher K, Feldman EL (2016) Inflammation as a therapeutic target for diabetic neuropathies. Curr Diab Rep 16:29
Mirza S, Hossain M, Mathews C, Martinez P, Pino P, Gay JL, Rentfro A, McCormick JB, Fisher-Hoch SP (2012) Type 2-diabetes is associated with elevated levels of TNF-alpha, IL-6 and adiponectin and low levels of leptin in a population of Mexican Americans: a cross-sectional study. Cytokine 57:136–142
Schenk S, Saberi M, Olefsky JM (2008) Insulin sensitivity: modulation by nutrients and inflammation. J Clin Invest 118:2992–3002
Mora C, Navarro JF (2006) Inflammation and diabetic nephropathy. Curr Diab Rep 6:463–468
Navarro JF, Mora C (2006) Diabetes, inflammation, proinflammatory cytokines, and diabetic nephropathy. Scientific World J 6:908–917
Shi X, Chen Y, Nadeem L, Xu G (2013) Beneficial effect of TNF-alpha inhibition on diabetic peripheral neuropathy. J Neuroinflammation 10:69
Davies LC, Jenkins SJ, Allen JE, Taylor PR (2013) Tissue-resident macrophages. Nat Immunol 14:986–995
Biswas SK, Mantovani A (2010) Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol 11:889–896
Gordon S, Martinez FO (2010) Alternative activation of macrophages: mechanism and functions. Immunity 32:593–604
Kiguchi N, Kobayashi D, Saika F, Matsuzaki S, Kishioka S (2017) Pharmacological Regulation of Neuropathic Pain Driven by Inflammatory Macrophages. Int J Mol Sci. https://doi.org/10.3390/ijms18112296
Kraakman MJ, Murphy AJ, Jandeleit-Dahm K, Kammoun HL (2014) Macrophage polarization in obesity and type 2 diabetes: weighing down our understanding of macrophage function? Front Immunol 5:470
DiPenta JM, Green-Johnson JM, Murphy RJ (2007) Type 2 diabetes mellitus, resistance training, and innate immunity: is there a common link? Appl Physiol Nutr Metab 32:1025–1035
Ahmad R, Al-Mass A, Atizado V, Al-Hubail A, Al-Ghimlas F, Al-Arouj M, Bennakhi A, Dermime S, Behbehani K (2012) Elevated expression of the toll like receptors 2 and 4 in obese individuals: its significance for obesity-induced inflammation. J Inflamm (Lond) 9:48
Creely SJ, McTernan PG, Kusminski CM, Fisher FM, Da Silva NF, Khanolkar M, Evans M, Harte AL, Kumar S (2007) Lipopolysaccharide activates an innate immune system response in human adipose tissue in obesity and type 2 diabetes. Am J Physiol Endocrinol Metab 292:E740-747
Morris J, Williams N, Rush C, Govan B, Sangla K, Norton R, Ketheesan N (2012) Burkholderia pseudomallei triggers altered inflammatory profiles in a whole-blood model of type 2 diabetes-melioidosis comorbidity. Infect Immun 80:2089–2099
Caricilli AM, Nascimento PH, Pauli JR, Tsukumo DM, Velloso LA, Carvalheira JB, Saad MJ (2008) Inhibition of toll-like receptor 2 expression improves insulin sensitivity and signaling in muscle and white adipose tissue of mice fed a high-fat diet. J Endocrinol 199:399–406
Elzinga S, Murdock BJ, Guo K, Hayes JM, Tabbey MA, Hur J, Feldman EL (2019) Toll-like receptors and inflammation in metabolic neuropathy; a role in early versus late disease? Exp Neurol 320:e112967
Gong W, Huang F, Sun L, Yu A, Zhang X, Xu Y, Shen Y, Cao J (2018) Toll-like receptor-2 regulates macrophage polarization induced by excretory-secretory antigens from Schistosoma japonicum eggs and promotes liver pathology in murine schistosomiasis. PLoS Negl Trop Dis 12:e0007000
Quero L, Hanser E, Manigold T, Tiaden AN, Kyburz D (2017) TLR2 stimulation impairs anti-inflammatory activity of M2-like macrophages, generating a chimeric M1/M2 phenotype. Arthritis Res Ther 19:245
Xu L, Tang D, Guan M, Xie C, Xue Y (2014) Effect of high-fat diet on peripheral neuropathy in C57BL/6 mice. Int J Endocrinol: https://doi.org/10.1155/2014/305205
O’Brien PD, Sakowski SA, Feldman EL (2014) Mouse models of diabetic neuropathy. Ilar j 54:259–272
Watcho P, Stavniichuk R, Ribnicky DM, Raskin I, Obrosova IG (2010) High-fat diet-induced neuropathy of prediabetes and obesity: effect of PMI-5011, an ethanolic extract of Artemisia dracunculus L. Mediators Inflamm. https://doi.org/10.1155/2010/268547
Saika F, Kiguchi N, Matsuzaki S, Kobayashi D, Kishioka S (2019) Inflammatory macrophages in the sciatic nerves facilitate neuropathic pain associated with type 2 diabetes mellitus. J Pharmacol Exp Ther 368:535–544
Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63
Weischenfeldt J, Porse B (2008) Bone marrow-derived macrophages (BMM): isolation and applications. CSH Protoc. https://doi.org/10.1101/pdb.prot5080
Mantovani A, Biswas SK, Galdiero MR, Sica A, Locati M (2013) Macrophage plasticity and polarization in tissue repair and remodelling. J Pathol 229:176–185
Martyn JA, Kaneki M, Yasuhara S (2008) Obesity-induced insulin resistance and hyperglycemia: etiologic factors and molecular mechanisms. Anesthesiology 109:137–148
Guilford BL, Ryals JM, Wright DE (2011) Phenotypic changes in diabetic neuropathy induced by a high-fat diet in diabetic C57BL/6 mice. Exp Diabetes Res. https://doi.org/10.1155/2011/848307
Obrosova IG, Ilnytska O, Lyzogubov VV, Pavlov IA, Mashtalir N, Nadler JL, Drel VR (2007) High-fat diet induced neuropathy of pre-diabetes and obesity: effects of “healthy” diet and aldose reductase inhibition. Diabetes 56:2598–2608
Vincent AM, Hayes JM, McLean LL, Vivekanandan-Giri A, Pennathur S, Feldman EL (2009) Dyslipidemia-induced neuropathy in mice: the role of oxLDL/LOX-1. Diabetes 58:2376–2385
Gordon S, Taylor PR (2005) Monocyte and macrophage heterogeneity. Nat Rev Immunol 5:953–964
Murray PJ (2017) Macrophage Polarization. Annu Rev Physiol 79:541–566
Wynn TA, Chawla A, Pollard JW (2013) Macrophage biology in development, homeostasis and disease. Nature 496:445–455
Kiguchi N, Maeda T, Kobayashi Y, Fukazawa Y, Kishioka S (2010) Macrophage inflammatory protein-1alpha mediates the development of neuropathic pain following peripheral nerve injury through interleukin-1beta up-regulation. Pain 149:305–315
Kellogg AP, Wiggin TD, Larkin DD, Hayes JM, Stevens MJ, Pop-Busui R (2007) Protective effects of cyclooxygenase-2 gene inactivation against peripheral nerve dysfunction and intraepidermal nerve fiber loss in experimental diabetes. Diabetes 56:2997–3005
Feng TT, Yang XY, Hao SS, Sun FF, Huang Y, Lin QS, Pan W (2020) TLR-2-mediated metabolic reprogramming participates in polyene phosphatidylcholine-mediated inhibition of M1 macrophage polarization. Immunol Res 68:28–38
Pahwa R, Jialal I (2016) Hyperglycemia Induces Toll-Like Receptor Activity Through Increased Oxidative Stress. Metab Syndr Relat Disord 14:239–241
Acknowledgements
The study was supported by Medical Science Research Project of Hebei Province (20191458).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tian, J., Song, T., Wang, H. et al. Toll-Like Receptor 2 Antagonist Ameliorates Type 2 Diabetes Mellitus Associated Neuropathic Pain by Repolarizing Pro-inflammatory Macrophages. Neurochem Res 46, 2276–2284 (2021). https://doi.org/10.1007/s11064-021-03365-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-021-03365-3