Abstract
Purpose
Magnetic resonance imaging (MRI) is the current standard for preoperative planning of glioblastoma (GBM) surgery. However, recent data on the use of 11 C-methionine positron emission tomography (11[C]-MET PET) suggest its role in providing additional information beyond MRI. The purpose of this study is to establish if there is a correlation between anatomical and metabolic data.
Methods
We retrieved all GBM cases treated from 2014 to January 2021. Preoperative MRI (Enhancing Nodule -EN-, FLAIR and Total Tumor Volume -TTV-), PET volumes and histological samples obtained from the different tumor regions were evaluated to analyze potential correlations between anatomical, metabolic and pathological data.
Results
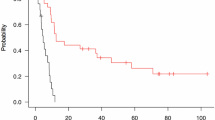
150 patients underwent surgery for GBM and 49 of these were also studied preoperatively with 11[C]-MET PET; PET volume was evaluated in 47 patients. In 33 patients (70.21%) preoperative 11[C]-MET PET volume > preoperative EN volume and in 11 (23.4%) preoperative 11[C]-MET PET volume > preoperative TTV. We found a significant correlation between preoperative TTVs and PET volumes (p = 0.016) as well as between preoperative EN volumes and PET volumes (p = < 0.001). Histologically, 109 samples were evaluated. ENs samples exhibited the conventional GBM morphology while samples from the FLAIR regions showed white matter tissue, with focal to diffuse tumor cells infiltration and areas of reactive astrogliosis.
Conclusion
We submit that 11[C]-MET PET volume generally overcome EN. The presence of neoplastic cells confirm these metabolic data. It should be considered in the surgical planning to achieve a Supra Total Resection (SupTR).



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Altieri R, Barbagallo D, Certo F et al (2021) Peritumoral Microenvironment in High-Grade Gliomas: from FLAIRectomy to Microglia-Glioma Cross-Talk. Brain Sci 11(2). https://doi.org/10.3390/brainsci11020200
D’Alessio A, Proietti G, Sica G, Scicchitano BM (2019) Pathological and molecular features of Glioblastoma and its Peritumoral tissue. Cancers 11(4). https://doi.org/10.3390/cancers11040469
Altieri R, Melcarne A, Soffietti R et al (2019) Supratotal Resection of Glioblastoma: is less more?Surg Technol Int. ; 35
Vivas-Buitrago T, Domingo RA, Tripathi S et al (2021) Influence of supramarginal resection on survival outcomes after gross-total resection of IDH-wild-type glioblastoma. J Neurosurg Published online June 4:1–8. https://doi.org/10.3171/2020.10.JNS203366
Li YM, Suki D, Hess K, Sawaya R (2016) The influence of maximum safe resection of glioblastoma on survival in 1229 patients: can we do better than gross-total resection? J Neurosurg 124(4):977–988. https://doi.org/10.3171/2015.5.JNS142087
Certo F, Altieri R, Maione M et al (2020) FLAIRectomy in Supramarginal Resection of Glioblastoma correlates with clinical outcome and survival analysis: a prospective, single Institution, Case Series. Oper Neurosurg Hagerstown Md. Published online October 9. https://doi.org/10.1093/ons/opaa293
Altieri R, Certo F, Rocca GL et al (2020) Radiological evaluation of ex novo high grade glioma: velocity of diametric expansion and acceleration time study. Radiol Oncol 55(1):26–34. https://doi.org/10.2478/raon-2020-0071
Mampre D, Ehresman J, Pinilla-Monsalve G et al (2018) Extending the resection beyond the contrast-enhancement for glioblastoma: feasibility, efficacy, and outcomes. Br J Neurosurg 32(5):528–535. https://doi.org/10.1080/02688697.2018.1498450
Albert NL, Weller M, Suchorska B et al (2016) Response Assessment in Neuro-Oncology working group and european Association for Neuro-Oncology recommendations for the clinical use of PET imaging in gliomas. Neuro-Oncol 18(9):1199–1208. https://doi.org/10.1093/neuonc/now058
Hirono S, Ozaki K, Kobayashi M et al (2021) Oncological and functional outcomes of supratotal resection of IDH1 wild-type glioblastoma based on 11 C-methionine PET: a retrospective, single-center study. Sci Rep 11(1):14554. https://doi.org/10.1038/s41598-021-93986-z
Barbagallo GMV, Palmucci S, Visocchi M et al (2016) Portable intraoperative computed tomography scan in image-guided surgery for Brain High-grade gliomas: analysis of Technical Feasibility and Impact on Extent of Tumor Resection. Oper Neurosurg Hagerstown Md 12(1):19–30. https://doi.org/10.1227/NEU.0000000000001112
Barbagallo GMV, Altieri R, Garozzo M et al (2020) High Grade Glioma Treatment in Elderly People: is it different than in younger patients? Analysis of Surgical Management guided by an intraoperative Multimodal Approach and its impact on clinical outcome. Front Oncol 10:631255. https://doi.org/10.3389/fonc.2020.631255
Barbagallo GMV, Certo F, Di Gregorio S, Maione M, Garozzo M, Peschillo S, Altieri R Recurrent high-grade glioma surgery: a multimodal intraoperative protocol to safely increase extent of tumor resection and analysis of its impact on patient outcome. Neurosurg Focus. 2021 Jan;50(1):E20. doi: https://doi.org/10.3171/2020.10.FOCUS20744. PMID: 33386001
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N Engl J Med 352(10):987–996. https://doi.org/10.1056/NEJMoa043330
Brandes AA, Tosoni A, Franceschi E et al (2009) Recurrence pattern after temozolomide concomitant with and adjuvant to radiotherapy in newly diagnosed patients with glioblastoma: correlation with MGMT promoter methylation status. J Clin Oncol 27(8):1275–1279. https://doi.org/10.1200/JCO.2008.19.4969
Brigliadori G, Foca F, Dall M et al (2016) Defining the cutoff value of MGMT gene promoter methylation and its predictive capacity in glioblastoma. J Neurooncol 128(2):333–339. https://doi.org/10.1007/s11060-016-2116-y
Altieri R, Zenga F, Ducati A et al Tumor location and patient age predict biological signatures of high-grade gliomas.Neurosurg Rev. Published online2017:1–6. doi: https://doi.org/10.1007/s10143-017-0899-8
Altieri R, Raimondo S, Tiddia C et al (2019) Glioma surgery: from preservation of motor skills to conservation of cognitive functions. J Clin Neurosci Off J Neurosurg Soc Australas Published online September 16. https://doi.org/10.1016/j.jocn.2019.08.091
Hervey-Jumper SL, Berger MS (2014) Role of surgical resection in low- and high-grade gliomas. Curr Treat Options Neurol 16(4). https://doi.org/10.1007/s11940-014-0284-7
Roh TH, Kang SG, Moon JH et al (2019) Survival benefit of lobectomy over gross-total resection without lobectomy in cases of glioblastoma in the noneloquent area: a retrospective study. J Neurosurg Published online March 1:1–7. https://doi.org/10.3171/2018.12.JNS182558
Schneider M, Ilic I, Potthoff AL et al (2020) Safety metric profiling in surgery for temporal glioblastoma: lobectomy as a supra-total resection regime preserves perioperative standard quality rates. J Neurooncol 149(3):455–461. https://doi.org/10.1007/s11060-020-03629-y
Pessina F, Navarria P, Cozzi L et al (2017) Maximize surgical resection beyond contrast-enhancing boundaries in newly diagnosed glioblastoma multiforme: is it useful and safe? A single institution retrospective experience. J Neurooncol 135(1):129–139. https://doi.org/10.1007/s11060-017-2559-9
Jiang H, Cui Y, Liu X, Ren X, Li M, Lin S (2019) Proliferation-dominant high-grade astrocytoma: survival benefit associated with extensive resection of FLAIR abnormality region. J Neurosurg Published online March 22:1–8. https://doi.org/10.3171/2018.12.JNS182775
Tripathi S, Vivas-Buitrago T, Domingo RA et al (2021) IDH-wild-type glioblastoma cell density and infiltration distribution influence on supramarginal resection and its impact on overall survival: a mathematical model. J Neurosurg Published online October 29:1–9. https://doi.org/10.3171/2021.6.JNS21925
Müther M, Koch R, Weckesser M, Sporns P, Schwindt W, Stummer W (2019) 5-Aminolevulinic acid fluorescence-guided resection of 18F-FET-PET positive tumor beyond Gadolinium Enhancing Tumor improves survival in Glioblastoma. Neurosurgery 85(6):E1020–E1029. https://doi.org/10.1093/neuros/nyz199
Katsanos AH, Alexiou GA, Fotopoulos AD, Jabbour P, Kyritsis AP, Sioka C (2019 Nov) Performance of 18F-FDG, 11 C-Methionine, and 18F-FET PET for Glioma Grading: a Meta-analysis. Clin Nucl Med 44(11):864–869. https://doi.org/10.1097/RLU.0000000000002654
Altieri R, Hirono S, Duffau H et al (2017) Natural history of de novo high Grade Glioma: first description of growth parabola. J Neurosurg Sci Published online July 26. https://doi.org/10.23736/S0390-5616.17.04067-X
Acknowledgements
We thank the Ginetta Ferraguti Association and the Scientific Bureau of the University of Catania for language support.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Study conception was performed by RA and FC. Material preparation and data collection were performed by RA, FC, GA, MG, GB, GR and SC. Data analysis and interpretation was performed by DP and GC. The first draft of the manuscript was written by RA, FC, GC and GB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University of Catania (CE 165/2015/PO).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altieri, R., Certo, F., Pacella, D. et al. Metabolic delineation of IDH1 wild-type glioblastoma surgical anatomy: how to plan the tumor extent of resection. J Neurooncol 162, 417–423 (2023). https://doi.org/10.1007/s11060-023-04305-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04305-7