Abstract
Purpose
To analyse whether the WHO grade of intracranial meningiomas differs itself depending on patients and meningioma characteristics at diagnosis.
Methods
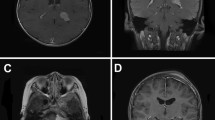
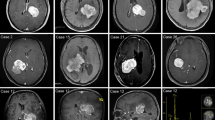
Single center retrospective study of a series of consecutive patients with primary intracranial meningiomas who underwent surgery between January 2007 and March 2014. Patients (age, sex, outcome) and meningioma characteristics (histological diagnosis, tumor location, WHO grading, size, extend of peritumoral edema and tumor recurrence rate) were analysed.
Results
Of 240 included patients, 184 (76.7%) were female and 56 (23.3%) were male. 17 patients (7.1%) were in age group 20–40 years, 112 (46.7%) in group 41–60 years and 111 (46.3%) were in age group > 60 years. 189 patients (78.8%) were diagnosed with WHO grade I, 49 (20.4%) WHO grade II and 2 (0.8%) had a WHO grade III meningioma. WHO grade II meningiomas were significantly more frequent in the age group 20–40 years compared to age group 41–60 years (chi-square p < 0.05). Convexity meningiomas were significantly more frequent classified as WHO grade II meningiomas compared to all other locations (chi-square, p < 0.01). Mean calculated tumor volume and the tumor volume determined by volumetric measurement was significantly larger in grade II meningioma patients compared to grade I (46.3 ± 40.5 cc grade II versus 21.8 ± 27.8 cc grade I and 45.3 ± 38.2 cc versus 23.1 ± 30.0 cc respectively; t test < 0.01). Extend of the peritumoral edema was significantly larger in patients with grade II meningiomas (Wilcoxon test, p < 0.05). Short term outcome did not differ between different age groups nor was it associated with tumor size. During a mean follow up of 49 months (min 3, max 144 months) recurrence rate was significantly higher in WHO grade II (4 out of 49 [8.2]%) compared to WHO grade I patients (3 out if 186, [1.6%]; Chi-square, p < 0.05).
Conclusion
In this series atypical meningioma was associated with younger age, location on the convexity, larger tumor size and more peritumoral edema.



Similar content being viewed by others
Abbreviations
- WHO:
-
World Health Organization
- CSF:
-
Cerebrospinal fluid
- GTR:
-
Gross total resection
- MRI:
-
Magnetic resonance imaging
- mRS:
-
Modified Rankin Scale
- RS:
-
Radiosurgery
- fSRT:
-
Fractionated stereotactic radiotherapy
References
Wiemels J, Wrensch M, Claus EB (2010) Epidemiology and etiology of meningioma. J Neurooncol 99:307–314. https://doi.org/10.1007/s11060-010-0386-3
Davis FG, Kupelian V, Freels S, McCarthy B, Surawicz T (2001) Prevalence estimates for primary brain tumors in the United States by behavior and major histology groups. Neuro-oncology 3:152–158. https://doi.org/10.1093/neuonc/3.3.152
Porter KR, McCarthy BJ, Freels S, Kim Y, Davis FG (2010) Prevalence estimates for primary brain tumors in the United States by age, gender, behavior, and histology. Neuro-oncology 12:520–527. https://doi.org/10.1093/neuonc/nop066
Baldi I, Engelhardt J, Bonnet C, Bauchet L, Berteaud E, Gruber A, Loiseau H (2014) Epidemiology of meningiomas. Neurochirurgie. https://doi.org/10.1016/j.neuchi.2014.05.006
Seifert V (2010) Clinical management of petroclival meningiomas and the eternal quest for preservation of quality of life: personal experiences over a period of 20 years. Acta Neurochir 152:1099–1116. https://doi.org/10.1007/s00701-010-0633-6
Jung HW, Yoo H, Paek SH, Choi KS (2000) Long-term outcome and growth rate of subtotally resected petroclival meningiomas: experience with 38 cases. Neurosurgery 46(3), 567–574, (discussion 574–565)
Couldwell WT, Kan P, Liu JK, Apfelbaum RI (2006) Decompression of cavernous sinus meningioma for preservation and improvement of cranial nerve function. Technical note. J Neurosurg 105:148–152. https://doi.org/10.3171/jns.2006.105.1.148
Gozal YM, Alzhrani G, Abou-Al-Shaar H, Azab MA, Walsh MT, Couldwell WT (2019) Outcomes of decompressive surgery for cavernous sinus meningiomas: long-term follow-up in 50 patients. J Neurosurg. https://doi.org/10.3171/2018.10.Jns181480
Karsy M, Jensen MR, Guan J, Ravindra VM, Bisson EF, Couldwell WT (2019) EQ-5D quality-of-life analysis and cost-effectiveness after skull base meningioma resection. Neurosurgery. https://doi.org/10.1093/neuros/nyz040
Jenkinson MD, Weber DC, Haylock BJ, Mallucci CL, Zakaria R, Javadpour M (2015) Atypical meningoma: current management dilemmas and prospective clinical trials. J Neurooncol 121:1–7. https://doi.org/10.1007/s11060-014-1620-1
Aghi MK, Carter BS, Cosgrove GR, Ojemann RG, Amin-Hanjani S, Martuza RL, Curry WT, Jr., Barker FG (2009) Long-term recurrence rates of atypical meningiomas after gross total resection with or without postoperative adjuvant radiation. Neurosurgery 64(1), 56–60, (discussion 60)
Jo K, Park HJ, Nam DH, Lee JI, Kong DS, Park K, Kim JH (2010) Treatment of atypical meningioma. J Clin Neurosci 17:1362–1366. https://doi.org/10.1016/j.jocn.2010.03.036
Rogers L, Gilbert M, Vogelbaum MA (2010) Intracranial meningiomas of atypical (WHO grade II) histology. J Neurooncol 99:393–405. https://doi.org/10.1007/s11060-010-0343-1
Gousias K, Schramm J, Simon M (2016) The Simpson grading revisited: aggressive surgery and its place in modern meningioma management. J Neurosurg 125:551–560. https://doi.org/10.3171/2015.9.Jns15754
Adeberg S, Hartmann C, Welzel T, Rieken S, Habermehl D, von Deimling A, Debus J, Combs SE (2012) Long-term outcome after radiotherapy in patients with atypical and malignant meningiomas–clinical results in 85 patients treated in a single institution leading to optimized guidelines for early radiation therapy. Int J Radiat Oncol Biol Phys 83:859–864. https://doi.org/10.1016/j.ijrobp.2011.08.010
Pearson BE, Markert JM, Fisher WS, Guthrie BL, Fiveash JB, Palmer CA, Riley K (2008) Hitting a moving target: evolution of a treatment paradigm for atypical meningiomas amid changing diagnostic criteria. Neurosurg Focus 24:E3. https://doi.org/10.3171/foc/2008/24/5/e3
Backer-Grondahl T, Moen BH, Arnli MB, Torseth K, Torp SH (2014) Immunohistochemical characterization of brain-invasive meningiomas. Int J Clin Exp Pathol 7:7206–7219
Backer-Grondahl T, Moen BH, Torp SH (2012) The histopathological spectrum of human meningiomas. Int J Clin Exp Pathol 5:231–242
Willis J, Smith C, Ironside JW, Erridge S, Whittle IR, Everington D (2005) The accuracy of meningioma grading: a 10-year retrospective audit. Neuropathol Appl Neurobiol 31:141–149. https://doi.org/10.1111/j.1365-2990.2004.00621.x
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39
Hale AT, Wang L, Strother MK, Chambless LB (2018) Differentiating meningioma grade by imaging features on magnetic resonance imaging. J Clin Neurosci 48:71–75. https://doi.org/10.1016/j.jocn.2017.11.013
Hale AT, Stonko DP, Wang L, Strother MK, Chambless LB (2018) Machine learning analyses can differentiate meningioma grade by features on magnetic resonance imaging. Neurosurg Focus 45:E4. https://doi.org/10.3171/2018.8.Focus18191
Goldbrunner R, Minniti G, Preusser M, Jenkinson MD, Sallabanda K, Houdart E, von Deimling A, Stavrinou P, Lefranc F, Lund-Johansen M, Moyal EC, Brandsma D, Henriksson R, Soffietti R, Weller M (2016) EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 17:e383–391. https://doi.org/10.1016/s1470-2045(16)30321-7
Nowak A, Dziedzic T, Krych P, Czernicki T, Kunert P, Marchel A (2015) Benign versus atypical meningiomas: risk factors predicting recurrence. Neurol Neurochir Pol 49:1–10. https://doi.org/10.1016/j.pjnns.2014.11.003
Magill ST, Young JS, Chae R, Aghi MK, Theodosopoulos PV, McDermott MW (2018) Relationship between tumor location, size, and WHO grade in meningioma. Neurosurg Focus 44:E4. https://doi.org/10.3171/2018.1.Focus17752
Sade B, Chahlavi A, Krishnaney A, Nagel S, Choi E, Lee JH (2007) World Health Organization grades II and III meningiomas are rare in the cranial base and spine. Neurosurgery 61(6), 1194–1198.https://doi.org/10.1227/01.neu.0000306097.38141.65, (discussion 1198)
Couldwell WT, MacDonald JD, Taussky P (2014) Complete resection of the cavernous sinus-indications and technique. World Neurosurg 82:1264–1270. https://doi.org/10.1016/j.wneu.2013.08.026
Liang RF, Xiu YJ, Wang X, Li M, Yang Y, Mao Q, Liu YH (2014) The potential risk factors for atypical and anaplastic meningiomas: clinical series of 1239 cases. Int J Clin Exp Med 7:5696–5700
Champeaux C, Weller J, Katsahian S (2019) Epidemiology of meningiomas. A nationwide study of surgically treated tumours on French medico-administrative data. Cancer Epidemiol 58:63–70. https://doi.org/10.1016/j.canep.2018.11.004
Wang DJ, Xie Q, Gong Y, Mao Y, Wang Y, Cheng HX, Zhong P, Che XM, Jiang CC, Huang FP, Zheng K, Li SQ, Gu YX, Bao WM, Yang BJ, Wu JS, Xie LQ, Zheng MZ, Tang HL, Zhu HD, Chen XC, Zhou LF (2013) Histopathological classification and location of consecutively operated meningiomas at a single institution in China from 2001 to 2010. Chin Med J 126:488–493
Sanai N, Sughrue ME, Shangari G, Chung K, Berger MS, McDermott MW (2010) Risk profile associated with convexity meningioma resection in the modern neurosurgical era. J Neurosurg 112:913–919. https://doi.org/10.3171/2009.6.Jns081490
Reinert M, Babey M, Curschmann J, Vajtai I, Seiler RW, Mariani L (2006) Morbidity in 201 patients with small sized meningioma treated by microsurgery. Acta Neurochir 148(12), 1257–1265. https://doi.org/10.1007/s00701-006-0909-z, ( discussion 1266)
Voss KM, Spille DC, Sauerland C, Suero Molina E, Brokinkel C, Paulus W, Stummer W, Holling M, Jeibmann A, Brokinkel B (2017) The Simpson grading in meningioma surgery: does the tumor location influence the prognostic value? J Neurooncol 133:641–651. https://doi.org/10.1007/s11060-017-2481-1
Sindou M (2001) Meningiomas invading the sagittal or transverse sinuses, resection with venous reconstruction. J Clin Neurosci 8(Suppl 1):8–11. https://doi.org/10.1054/jocn.2001.0868
Sindou M (2014) Meningiomas involving major dural sinuses: should we attempt at radical removal and venous repair? World Neurosurg 81:46–47. https://doi.org/10.1016/j.wneu.2013.07.119
Sindou M, Hallacq P (1998) Venous reconstruction in surgery of meningiomas invading the sagittal and transverse sinuses. Skull Base Surg 8:57–64
Caroli E, Orlando ER, Mastronardi L, Ferrante L (2006) Meningiomas infiltrating the superior sagittal sinus: surgical considerations of 328 cases. Neurosurg Rev 29:236–241. https://doi.org/10.1007/s10143-006-0020-1
Tomasello F, Conti A, Cardali S, Angileri FF (2013) Venous preservation-guided resection: a changing paradigm in parasagittal meningioma surgery. J Neurosurg 119:74–81. https://doi.org/10.3171/2012.11.jns112011
Alvernia JE, Dang ND, Sindou MP (2011) Convexity meningiomas: study of recurrence factors with special emphasis on the cleavage plane in a series of 100 consecutive patients. J Neurosurg 115:491–498. https://doi.org/10.3171/2011.4.jns101922
Jadid KD, Feychting M, Hoijer J, Hylin S, Kihlstrom L, Mathiesen T (2015) Long-term follow-up of incidentally discovered meningiomas. Acta Neurochir 157:225–230. https://doi.org/10.1007/s00701-014-2306-3
Sindou M, Nebbal M, Guclu B (2015) Cavernous sinus meningiomas: imaging and surgical strategy. Adv Tech Stand Neurosurg 42:103–121. https://doi.org/10.1007/978-3-319-09066-5_6
Schmieder K, Engelhardt M, Wawrzyniak S, Borger S, Becker K, Zimolong A (2010) The impact of microsurgery, stereotactic radiosurgery and radiotherapy in the treatment of meningiomas depending on different localizations. GMS Health Technol Assess. https://doi.org/10.3205/hta000080
Hamm K, Henzel M, Gross MW, Surber G, Kleinert G, Engenhart-Cabillic R (2008) Radiosurgery/stereotactic radiotherapy in the therapeutical concept for skull base meningiomas. Zentralbl Neurochir 69:14–21. https://doi.org/10.1055/s-2007-992138
Combs SE, Ganswindt U, Foote RL, Kondziolka D, Tonn JC (2012) State-of-the-art treatment alternatives for base of skull meningiomas: complementing and controversial indications for neurosurgery, stereotactic and robotic based radiosurgery or modern fractionated radiation techniques. Radiat Oncol 7:226. https://doi.org/10.1186/1748-717x-7-226
Sughrue ME, Rutkowski MJ, Aranda D, Barani IJ, McDermott MW, Parsa AT (2010) Factors affecting outcome following treatment of patients with cavernous sinus meningiomas. J Neurosurg 113:1087–1092. https://doi.org/10.3171/2010.3.jns091807
Cohen-Inbar O, Lee CC, Schlesinger D, Xu Z, Sheehan JP (2015) Long-term results of stereotactic radiosurgery for skull base meningiomas. Neurosurgery. https://doi.org/10.1227/neu.0000000000001045
Zhou P, Ma W, Yin S, Li Y, Jiang S (2013) Three risk factors for WHO grade II and III meningiomas: a study of 1737 cases from a single center. Neurol India 61:40–44. https://doi.org/10.4103/0028-3886.107928
Kane AJ, Sughrue ME, Rutkowski MJ, Shangari G, Fang S, McDermott MW, Berger MS, Parsa AT (2011) Anatomic location is a risk factor for atypical and malignant meningiomas. Cancer 117:1272–1278. https://doi.org/10.1002/cncr.25591
Mahmood A, Caccamo DV, Tomecek FJ, Malik GM (1993) Atypical and malignant meningiomas: a clinicopathological review. Neurosurgery 33:955–963
Maier H, Ofner D, Hittmair A, Kitz K, Budka H (1992) Classic, atypical, and anaplastic meningioma: three histopathological subtypes of clinical relevance. J Neurosurg 77:616–623. https://doi.org/10.3171/jns.1992.77.4.0616
Zaher A, Abdelbari Mattar M, Zayed DH, Ellatif RA, Ashamallah SA (2013) Atypical meningioma: a study of prognostic factors. World Neurosurg 80:549–553. https://doi.org/10.1016/j.wneu.2013.07.001
Budohoski KP, Clerkin J, Millward CP, O'Halloran PJ, Waqar M, Looby S, Young AMH, Guilfoyle MR, Fitzroll D, Devadass A, Allinson K, Farrell M, Javadpour M, Jenkinson MD, Santarius T, Kirollos RW (2018) Predictors of early progression of surgically treated atypical meningiomas. Acta Neurochir 160:1813–1822. https://doi.org/10.1007/s00701-018-3593-x
Aboukais R, Baroncini M, Zairi F, Reyns N, Lejeune JP (2013) Early postoperative radiotherapy improves progression free survival in patients with grade 2 meningioma. Acta Neurochir 155(8), 1385–1390. https://doi.org/10.1007/s00701-013-1775-0, (discussion 1390)
Bagshaw HP, Burt LM, Jensen RL, Suneja G, Palmer CA, Couldwell WT, Shrieve DC (2017) Adjuvant radiotherapy for atypical meningiomas. J Neurosurg 126:1822–1828. https://doi.org/10.3171/2016.5.Jns152809
Hasan S, Young M, Albert T, Shah AH, Okoye C, Bregy A, Lo SS, Ishkanian F, Komotar RJ (2014) The role of adjuvant radiotherapy following gross total resection of atypical meningiomas. World Neurosurg. https://doi.org/10.1016/j.wneu.2014.12.037
Jenkinson MD, Javadpour M, Haylock BJ, Young B, Gillard H, Vinten J, Bulbeck H, Das K, Farrell M, Looby S, Hickey H, Preusser M, Mallucci CL, Hughes D, Gamble C, Weber DC (2015) The ROAM/EORTC-1308 trial: radiation versus observation following surgical resection of atypical meningioma: study protocol for a randomised controlled trial. Trials 16:519. https://doi.org/10.1186/s13063-015-1040-3
Narayan V, Bir SC, Mohammed N, Savardekar AR, Patra DP, Nanda A (2018) Surgical management of giant intracranial meningioma: operative nuances, challenges, and outcome. World Neurosurg 110:e32–e41. https://doi.org/10.1016/j.wneu.2017.09.184
Sahm F, Schrimpf D, Stichel D, Jones DTW, Hielscher T, Schefzyk S, Okonechnikov K, Koelsche C, Reuss DE, Capper D, Sturm D, Wirsching HG, Berghoff AS, Baumgarten P, Kratz A, Huang K, Wefers AK, Hovestadt V, Sill M, Ellis HP, Kurian KM, Okuducu AF, Jungk C, Drueschler K, Schick M, Bewerunge-Hudler M, Mawrin C, Seiz-Rosenhagen M, Ketter R, Simon M, Westphal M, Lamszus K, Becker A, Koch A, Schittenhelm J, Rushing EJ, Collins VP, Brehmer S, Chavez L, Platten M, Hanggi D, Unterberg A, Paulus W, Wick W, Pfister SM, Mittelbronn M, Preusser M, Herold-Mende C, Weller M, von Deimling A (2017) DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol 18:682–694. https://doi.org/10.1016/s1470-2045(17)30155-9
Bi WL, Zhang M, Wu WW, Mei Y, Dunn IF (2016) Meningioma genomics: diagnostic, prognostic, and therapeutic applications. Front Surg 3:40. https://doi.org/10.3389/fsurg.2016.00040
Abedalthagafi M, Bi WL, Aizer AA, Merrill PH, Brewster R, Agarwalla PK, Listewnik ML, Dias-Santagata D, Thorner AR, Van Hummelen P, Brastianos PK, Reardon DA, Wen PY, Al-Mefty O, Ramkissoon SH, Folkerth RD, Ligon KL, Ligon AH, Alexander BM, Dunn IF, Beroukhim R, Santagata S (2016) Oncogenic PI3K mutations are as common as AKT1 and SMO mutations in meningioma. Neuro-oncology 18:649–655. https://doi.org/10.1093/neuonc/nov316
Clark VE, Erson-Omay EZ, Serin A, Yin J, Cotney J, Ozduman K, Avsar T, Li J, Murray PB, Henegariu O, Yilmaz S, Gunel JM, Carrion-Grant G, Yilmaz B, Grady C, Tanrikulu B, Bakircioglu M, Kaymakcalan H, Caglayan AO, Sencar L, Ceyhun E, Atik AF, Bayri Y, Bai H, Kolb LE, Hebert RM, Omay SB, Mishra-Gorur K, Choi M, Overton JD, Holland EC, Mane S, State MW, Bilguvar K, Baehring JM, Gutin PH, Piepmeier JM, Vortmeyer A, Brennan CW, Pamir MN, Kilic T, Lifton RP, Noonan JP, Yasuno K, Gunel M (2013) Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 339:1077–1080. https://doi.org/10.1126/science.1233009
Abedalthagafi MS, Bi WL, Merrill PH, Gibson WJ, Rose MF, Du Z, Francis JM, Du R, Dunn IF, Ligon AH, Beroukhim R, Santagata S (2015) ARID1A and TERT promoter mutations in dedifferentiated meningioma. Cancer Genetics 208:345–350. https://doi.org/10.1016/j.cancergen.2015.03.005
Furtjes G, Kochling M, Peetz-Dienhart S, Wagner A, Hess K, Hasselblatt M, Senner V, Stummer W, Paulus W, Brokinkel B (2016) hTERT promoter methylation in meningiomas and central nervous hemangiopericytomas. J Neurooncol 130:79–87. https://doi.org/10.1007/s11060-016-2226-6
Goutagny S, Nault JC, Mallet M, Henin D, Rossi JZ, Kalamarides M (2014) High incidence of activating TERT promoter mutations in meningiomas undergoing malignant progression. Brain Pathol 24:184–189. https://doi.org/10.1111/bpa.12110
Sahm F, Schrimpf D, Olar A, Koelsche C, Reuss D, Bissel J, Kratz A, Capper D, Schefzyk S, Hielscher T, Wang Q, Sulman EP, Adeberg S, Koch A, Okuducu AF, Brehmer S, Schittenhelm J, Becker A, Brokinkel B, Schmidt M, Ull T, Gousias K, Kessler AF, Lamszus K, Debus J, Mawrin C, Kim YJ, Simon M, Ketter R, Paulus W, Aldape KD, Herold-Mende C, von Deimling A (2016) TERT Promoter Mutations and Risk of Recurrence in Meningioma. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djv377
Acknowledgement
The authors are grateful to Dr. Hanns Ackermann, Goethe University Frankfurt/ Main, Germany for his support and counselling of statistical tests. We thank Dr. Charles L. Rosen, M.D., PhD. for his editorial assistance.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ressel, A., Fichte, S., Brodhun, M. et al. WHO grade of intracranial meningiomas differs with respect to patient’s age, location, tumor size and peritumoral edema. J Neurooncol 145, 277–286 (2019). https://doi.org/10.1007/s11060-019-03293-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03293-x