Abstract
Background and purpose
Post-operative SRS (stereotactic radiosurgery) for large brain metastases is challenged by risks of radiation necrosis that limit SRS dose. Intraoperative radiotherapy (IORT) is a potential alternative, however standard dose recommendations are lacking.
Methods and materials
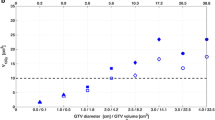
Twenty consecutive brain metastases treated with post-operative SRS were retrospectively compared to IORT plans generated for 10–30 Gy in 1 fraction to 0–5 mm by estimating the applicator size and distance from critical organs using pre-operative and post-operative MRI. Additionally, 7 consecutive patients treated with IORT 30 Gy to surface were compared to retrospectively generated SRS plans using the post-operative MRI to 15–20 Gy and 30 Gy in 1 fraction marginal dose.
Results
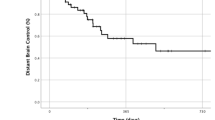
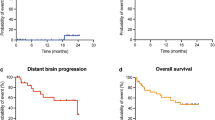
For the 20 resection cavities treated with SRS and retrospectively compared to IORT, IORT from 10 to 30Gy resulted in lower or not significantly different doses to the optic apparatus and brainstem. Comparatively for the 7 patients treated with IORT 30 Gy to retrospective SRS plans to standard 15–20 Gy and 30 Gy marginal dose, IORT resulted in significantly lower doses to the optic apparatus and brainstem. At a median follow-up of 6.2 months, 86% of patients treated with surgery and IORT achieved local control and 0% developed radiographic or symptomatic radiation necrosis.
Conclusions
Critical organ dosimetry for IORT remains generally lower than that achieved with single fraction SRS following resection of large brain metastases. We recommend 30 Gy to surface as the preferred prescription, consistent with the dose recommendation for IORT in glioblastoma used in the ongoing INTRAGO-II phase-III trial. Early clinical outcomes appear promising for surgery and IORT.




Similar content being viewed by others
References
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29:134–141
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316:401–409
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomized contolled trial. Lancet 10:1037–1044
Brown PD, Ballman KV, Cerhan J et al (2017) N107C/CEC.3: a Phase III trial of post-operative stereotactic radiosurgery (SRS) compared with whole brain radiotherapy (WBRT) for resected metastatic brain disease. Lancet Oncol 18:1049–1060
Mahajan A, Ahmed S, McAleer MF et al (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1040–1048
Weil RJ, Mavinkurve CG, Chao ST et al (2015) Intraoperative radiotherapy to treat newly diagnosed solitary brain metastasis: initial experience and long-term outcomes. J Neurosurg 122:825–832
Curry WT Jr, Cosgrove GR, Hochberg FH et al (2005) Stereotactic interstitial radiosurgery for cerebral metastases. J Neurosurg 103:6305
Pantazis G, Trippel M, Birg W et al (2009) Stereotactic interstitial radiosurgery with the photon radiosurgery system (PRS) for metastatic brain tumors: a prospective single-center clinical trial. Int J Radiat Oncol Biol Phys 75:1392–1400
Kalapurakal JA, Goldman S, Stellpfung W et al (2006) Phase I study of intraoperative radiotherapy with photon radiosurgery system in children with recurrent brain tumors: preliminary report of first dose level (10 Gy). Int J Radiat Oncol Biol Phys 65:800–808
Giordano FA, Brehmer S, Abo-Madyan Y et al (2014) INTRAGO: intraoperative radiotherapy in glioblastoma multiforme: a phase I/II dose escalation study. BMC Cancer 14:992
Wernicke AG, Hirschfeld CB, Smith AW et al (2017) Clinical outcomes of large brain metastases treated with neurosurgical resection and intra-operative Cesium-131 brachytherapy: results of a prospective trial. Int J Radiat Oncol Biol Phys 98:1059–1068
Raleigh DR, Seymore ZA, Tomlin B et al (2017) Resection and brain brachytherapy with permanent idodine-125 sources for brain metastasis. J Neurosurg 126:1749–1755
Flickinger JC, Kondziolka D, Maitz AH, Lunsford LD (1998) Analysis of neurological sequelae from radiosurgery of arteriovenous malformations: how location affects outcome. Int J Radiat Oncol Biol Phys 40:273–278
Levegrun S, Hof H, Essig M, Sclegel W, Debus J (2004) Radiation-induced changes of brain tissue after radiosurgery in patients with arteriovenous malformations: correlation with dose distribution parameters. Int J Radiat Oncol Biol Phys 59:796–808
Belletti B, Vaidya JS, D’Andrea S et al (2008) Targeted intraoperative radiotherapy impairs the stimulation of breast cancer cell proliferation and invasion caused by surgical wounding. Clin Cancer Res 14:1325–1332
Di Lorenzo N, Cavedon C, Paier F et al (2004) Interstitial radiosurgery with the photon radiosurgery system in the minimally-invasive treatment of selected deep-seated brain tumors. J Chemother 16:70–74
Gallina P, Franceson P, Cavedon C et al (2002) Stereotactic interstitial radiosurgery with a miniature X-ray device in the minimally invasive treatment of selected tumors in the thalamus and the basal Ganglia. Stereotact Funt Neurosurg 79:202–213
Vaidya JS, Wenz F, Bulsara M et al (2014) Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-A randomised trial. Lancet 383:603–613
Siam L, Bleckmann A, Chaung HN et al (2015) The metastatic infiltration at the metastasis/brain parenchyma-interface is very heterogeneous and has a significant impact on survival in a prospective study. Oncotarget 6:29254–29267
Raore B, Schniederjan M, Prabhu R et al (2011) Metastasis infiltration: an investigation of the postoperative brain-tumor interface. Int J Radiat Oncol Biol Phys 81:1075–1080
Baumert BG, Rutten I, Dehing-Oberije C et al (2006) A pathology-based substrate for target definition in radiosurgery of brain metastases. Int J Radiat Oncol Biol Phys 66:187–194
Brennan C, Yang TJ, Hilden P et al (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys 88:130–136
Choi CY, Chang SD, Gibbs IC et al (2012) Stereotactic radiosurgery of the postoperative resection cavity for brain metastases: prospective evaluation of target margin on tumor control. Int J Radiat Oncol Biol Phys 84:336–342
Chen Y, Souri S, Dian X et al (2016) SU-F-T-56: Dosimetric characterization of the INTRABEAM 50 kV Xray system with a needle applicator in heterogeneous tissues. Med Phys 43:3474
Liu Q, Schneider F, Ma L, Wenz F, Herskind C (2013) Relative biologic effectiveness (RBE) of 50 kV X-rays measured in a phantom for intraoperative tumor-bed irradiation. Int J Radiat Oncol Biol Phys 85:1127–1133
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
John A Vargo, MD receives speaking honoraria from BrainLAB. All remaining authors declare they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study for treatment delivery.
Additional information
Data was accepted for presentation in abstract format at The Annual Meeting of the Leksell GammaKnife Society 2018 (Dubai, UAE), World Congress of Brachytherapy 2018 (San Francisco, USA), and International Society of Intraoperative Radiation Therapy 2018 (Mannheim, Germany).
Rights and permissions
About this article
Cite this article
Vargo, J.A., Sparks, K.M., Singh, R. et al. Feasibility of dose escalation using intraoperative radiotherapy following resection of large brain metastases compared to post-operative stereotactic radiosurgery. J Neurooncol 140, 413–420 (2018). https://doi.org/10.1007/s11060-018-2968-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2968-4