Abstract
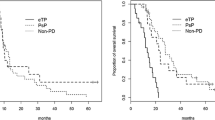
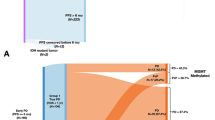
Pseudoprogression (psPD) refers to an increase in size or appearance of new areas of MRI contrast enhancement soon after completing chemoradiation, timely diagnosis of which has been a challenge. Given that tissue sampling of the MRI changes would be expected to accurately distinguish psPD from true progression when MRI changes are first seen, we examined the utility of surgery in diagnosing psPD and influencing patient outcome. We retrospectively reviewed data from adults with GBM who had MRI changes suggestive of progression within 3 months of chemoRT; of these, 34 underwent surgical resection. Three subsets–tumor, psPD or mixed-were identified based on histology and immunohistochemistry in the surgical group and by imaging characteristics in the nonsurgical group. A cohort of patients with stable disease post-chemoRT served as control. PFS and OS were determined using the Kaplan–Meier method and log rank analysis. Concordance for psPD between radiological interpretation and subsequent histological diagnosis was seen in only 32 % of cases (11/34) 95 %CI 19–49 %. A large proportion of patients had a histologically “mixed” pattern with tumor and treatment effect. No significant differences in PFS or OS were seen among the three subtypes. Surgical sampling and histologic review of MRI changes after chemoRT may not serve as a gold standard to distinguish psPD from true progression in GBM patients. Refinement of the histological criteria, careful intraoperative selection of regions of interest and advanced imaging modalities are needed for early differentiation of PsPD from progression to guide clinical management.



Similar content being viewed by others
References
States CBTRotU (2004–2006) CBTRUS Report 2004–2006. http://www.cbtrus.org
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. doi:10.1056/NEJMoa043330
Brandsma D, Stalpers L, Taal W, Sminia P, van den Bent MJ (2008) Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol 9:453–461. doi:10.1016/S1470-2045(08)70125-6
de Wit MC, de Bruin HG, Eijkenboom W, Sillevis Smitt PA, van den Bent MJ (2004) Immediate post-radiotherapy changes in malignant glioma can mimic tumor progression. Neurology 63:535–537
Hoffman WF, Levin VA, Wilson CB (1979) Evaluation of malignant glioma patients during the postirradiation period. J Neurosurg 50:624–628. doi:10.3171/jns.1979.50.5.0624
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, Degroot J, Wick W, Gilbert MR, Lassman AB, Tsien C, Mikkelsen T, Wong ET, Chamberlain MC, Stupp R, Lamborn KR, Vogelbaum MA, van den Bent MJ, Chang SM (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972. doi:10.1200/JCO.2009.26.3541
Clarke JL, Chang S (2009) Pseudoprogression and pseudoresponse: challenges in brain tumor imaging. Curr Neurol Neurosci Rep 9:241–246
Taal W, Brandsma D, de Bruin HG, Bromberg JE, Swaak-Kragten AT, Smitt PA, van Es CA, van den Bent MJ (2008) Incidence of early pseudo-progression in a cohort of malignant glioma patients treated with chemoirradiation with temozolomide. Cancer 113:405–410. doi:10.1002/cncr.23562
Brandes AA, Franceschi E, Tosoni A, Blatt V, Pession A, Tallini G, Bertorelle R, Bartolini S, Calbucci F, Andreoli A, Frezza G, Leonardi M, Spagnolli F, Ermani M (2008) MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J Clin Oncol 26:2192–2197. doi:10.1200/JCO.2007.14.8163
Chamberlain MC, Glantz MJ, Chalmers L, Van Horn A, Sloan AE (2007) Early necrosis following concurrent Temodar and radiotherapy in patients with glioblastoma. J Neurooncol 82:81–83. doi:10.1007/s11060-006-9241-y
Kumar AJ, Leeds NE, Fuller GN, Van Tassel P, Maor MH, Sawaya RE, Levin VA (2000) Malignant gliomas: MR imaging spectrum of radiation therapy- and chemotherapy-induced necrosis of the brain after treatment. Radiology 217:377–384
Mullins ME, Barest GD, Schaefer PW, Hochberg FH, Gonzalez RG, Lev MH (2005) Radiation necrosis versus glioma recurrence: conventional MR imaging clues to diagnosis. Am J Neuroradiol 26:1967–1972
Kleihues PBP, Aldape KD (2007) Glioblastoma. In: Louis DNOH, Wiestler OD, Webster KC (eds) who classification for tumours of the central nervous system. International Agency for Research on Cancer, Lyon, pp 33–49
Perry A, Schmidt RE (2006) Cancer therapy-associated CNS neuropathology: an update and review of the literature. Acta Neuropathol 111:197–212. doi:10.1007/s00401-005-0023-y
Shah A, Young R, Beal K, Karimi S, Shi W, Zhang Z, Holodny A (2009) Identifying pseudoprogression in glioblastoma: utility of conventional MR findings. Neuro-oncology 11:563
Young RJ, Gupta A, Shah AD, Graber JJ, Zhang Z, Shi W, Holodny AI, Omuro AM (2011) Potential utility of conventional MRI signs in diagnosing pseudoprogression in glioblastoma. Neurology 76:1918–1924. doi:10.1212/WNL.0b013e31821d74e7
Nobusawa S, Watanabe T, Kleihues P, Ohgaki H (2009) IDH1 mutations as molecular signature and predictive factor of secondary glioblastomas. Clin Cancer Res 15:6002–6007. doi:10.1158/1078-0432.CCR-09-0715
Capper D, Sahm F, Hartmann C, Meyermann R, von Deimling A, Schittenhelm J (2010) Application of mutant IDH1 antibody to differentiate diffuse glioma from nonneoplastic central nervous system lesions and therapy-induced changes. Am J Surg Pathol 34:1199–1204. doi:10.1097/PAS.0b013e3181e7740d
Motegi H, Kamoshima Y, Terasaka S, Kobayashi H, Yamaguchi S, Tanino M, Murata J, Houkin K (2012) IDH1 mutation as a potential novel biomarker for distinguishing pseudoprogression from true progression in patients with glioblastoma treated with temozolomide and radiotherapy. Brain Tumor Pathol. doi:10.1007/s10014-012-0109-x
Juratli TA, Engellandt K, Lautenschlaeger T, Geiger KD, von Kummer R, Cerhova J, Chakravarti A, Krex D, Schackert G (2013) is there pseudoprogression in secondary glioblastomas? Int J Radiat Oncol 87:1094–1099. doi:10.1016/j.ijrobp.2013.09.036
Pouleau HB, Sadeghi N, Baleriaux D, Melot C, De Witte O, Lefranc F (2012) High levels of cellular proliferation predict pseudoprogression in glioblastoma patients. Int J Oncol 40:923–928. doi:10.3892/ijo.2011.1260
Kim JH, Bae Kim Y, Han JH, Cho KG, Kim SH, Sheen SS, Lee HW, Jeong SY, Kim BY, Lee KB (2012) Pathologic diagnosis of recurrent glioblastoma: morphologic, immunohistochemical, and molecular analysis of 20 paired cases. Am J Surg Pathol 36:620–628. doi:10.1097/PAS.0b013e318246040c
Moskowitz SI, Jin T, Prayson RA (2006) Role of MIB1 in predicting survival in patients with glioblastomas. J Neurooncol 76:193–200. doi:10.1007/s11060-005-5262-1
Gerstner ER, McNamara MB, Norden AD, Lafrankie D, Wen PY (2009) Effect of adding temozolomide to radiation therapy on the incidence of pseudo-progression. J Neurooncol 94:97–101. doi:10.1007/s11060-009-9809-4
Alexiou GA, Tsiouris S, Kyritsis AP, Voulgaris S, Argyropoulou MI, Fotopoulos AD (2009) Glioma recurrence versus radiation necrosis: accuracy of current imaging modalities. J Neurooncol 95:1–11. doi:10.1007/s11060-009-9897-1
Hu LS, Baxter LC, Smith KA, Feuerstein BG, Karis JP, Eschbacher JM, Coons SW, Nakaji P, Yeh RF, Debbins J, Heiserman JE (2009) Relative cerebral blood volume values to differentiate high-grade glioma recurrence from posttreatment radiation effect: direct correlation between image-guided tissue histopathology and localized dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging measurements. Am J Neuroradiol 30:552–558. doi:10.3174/ajnr.A1377
Zeng QS, Li CF, Zhang K, Liu H, Kang XS, Zhen JH (2007) Multivoxel 3D proton MR spectroscopy in the distinction of recurrent glioma from radiation injury. J Neurooncol 84:63–69. doi:10.1007/s11060-007-9341-3
Zeng QS, Li CF, Liu H, Zhen JH, Feng DC (2007) Distinction between recurrent glioma and radiation injury using magnetic resonance spectroscopy in combination with diffusion-weighted imaging. Int J Radiat Oncol Biol Phys 68:151–158. doi:10.1016/j.ijrobp.2006.12.001
Gahramanov S, Raslan AM, Muldoon LL, Hamilton BE, Rooney WD, Varallyay CG, Njus JM, Haluska M, Neuwelt EA (2011) Potential for differentiation of pseudoprogression from true tumor progression with dynamic susceptibility-weighted contrast-enhanced magnetic resonance imaging using ferumoxytol vs. gadoteridol: a pilot study. Int J Radiat Oncol Biol Phys 79:514–523. doi:10.1016/j.ijrobp.2009.10.072
Hu X, Wong KK, Young GS, Guo L, Wong ST (2011) Support vector machine multiparametric MRI identification of pseudoprogression from tumor recurrence in patients with resected glioblastoma. J Magn Reson Imaging 33:296–305. doi:10.1002/jmri.22432
Young RJ, Gupta A, Shah AD, Graber JJ, Chan TA, Zhang Z, Shi W, Beal K, Omuro AM (2013) MRI perfusion in determining pseudoprogression in patients with glioblastoma. Clin Imaging 37:41–49. doi:10.1016/j.clinimag.2012.02.016
Gahramanov S, Muldoon LL, Varallyay CG, Li X, Kraemer DF, Fu R, Hamilton BE, Rooney WD, Neuwelt EA (2012) Pseudoprogression of glioblastoma after chemo- and radiation therapy: diagnosis by using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging with ferumoxytol versus gadoteridol and correlation with survival. Radiology. doi:10.1148/radiol.12111472
Hu LS, Eschbacher JM, Heiserman JE, Dueck AC, Shapiro WR, Liu S, Karis JP, Smith KA, Coons SW, Nakaji P, Spetzler RF, Feuerstein BG, Debbins J, Baxter LC (2012) Reevaluating the imaging definition of tumor progression: perfusion MRI quantifies recurrent glioblastoma tumor fraction, pseudoprogression, and radiation necrosis to predict survival. Neuro Oncol 14:919–930. doi:10.1093/neuonc/nos112
Conflict of interest
Funding: VKP was supported by NCI grant K24CA160777. The remaining authors declare that they have no relevant funding sources. None of the authors have any relevant conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Melguizo-Gavilanes, I., Bruner, J.M., Guha-Thakurta, N. et al. Characterization of pseudoprogression in patients with glioblastoma: is histology the gold standard?. J Neurooncol 123, 141–150 (2015). https://doi.org/10.1007/s11060-015-1774-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1774-5