Abstract
Neuroblastoma is the most common extracranial solid tumor of childhood. While survival rates are high for localized disease, treatment response remains poor for a subset of patients with large tumors or disseminated disease. Thus, there remains much room for improvement in treatment strategies for this disease. Using in vitro and in vivo systems, we present glycogen synthase kinase-3β (GSK-3β) inhibition as a potential mechanism to treat neuroblastoma. Using the specific GSK-3β inhibitor SB415286, we demonstrate that GSK-3β inhibition decreases the viability of Neuro-2A cells, as determined by cell proliferation assay and clonogenic survival. Moreover, we show that GSK-3β inhibition induces apoptosis in neuroblastoma cells, as determined by Annexin V staining and confirmed with DAPI staining. Using flow cytometry, we are able to demonstrate that SB415286 induces the accumulation of cells in the G2/M phase of the cell cycle. Finally, we show that these in vitro results translate into delayed tumor growth in vivo using a heterotopic tumor model in nude mice treated with SB415286. These findings suggest that GSK-3β is a potential molecular target for the treatment of neuroblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma is an extracranial solid tumor of childhood, accounting for 7.8% of childhood cancers in the United States with approximately 650 new cases diagnosed per year, according to the Surveillance, Epidemiology, and End Report (SEER). It is a malignancy of the neural crest cells arising from the adrenal medulla and paraspinal sympathetic ganglia. Neuroblastoma accounts for 8–10% of all childhood cancers and for approximately 15% of cancer deaths in children. While localized tumors are often responsive to chemotherapy, patients with high risk phenotypes have long term survival rates of less than 40% despite multi-modality treatment approaches including chemotherapy, radical surgery, and radiation therapy [1, 2]. With only modest improvements in the outcomes of this high risk group during the past few decades, there is clearly a need for new treatment strategies, potentially represented by molecular target-directed drugs.
Glycogen synthase kinase 3 beta (GSK-3β) is a ubiquitously expressed multifunctional serine/threonine kinase [3]. Initially identified as a kinase and inactivator of glycogen synthase, it is now known to have over forty substrates [4] and to regulate a wide range of cellular functions including differentiation, growth, proliferation, motility, cell cycle progression, and apoptosis [5]. Aside from its association with non-insulin dependent diabetes mellitus, it is highly expressed in the brain and contributes to neurologic disorders such as Alzheimer’s disease, schizophrenia, and bipolar disorder [6]. Of special interest is the involvement of GSK-3β in cancer, with data supporting both a role as a tumor suppressor or a tumor promoter, a discrepancy that depends on cell type and conditions. For example, the kinase has been shown to inhibit androgen-receptor stimulated cell growth in prostate cancer, thus acting as a tumor suppressor [7]. In contrast, GSK-3β is highly expressed in colorectal cancer [8, 9] and has been shown to participate in nuclear factor κB (NFκB)-mediated cell survival in pancreatic cancer [10], thus behaving like a tumor promoter. Moreover, the kinase has dual functions in the regulation of cell survival where it can either activate or inhibit apoptosis [4], further complicating its involvement in cancer. Therefore, it is important to carefully study GSK-3β in specific cell types of interest to determine whether potential therapeutic gains can best be made from either the inhibition or activation of this molecular target.
Recent evidence suggests a potential role for GSK-3β inhibition in the treatment of neuroblastoma. In a B65 neuroblastoma cell line, inhibition of the kinase-induced cell cycle arrest that corresponded with reduced cell proliferation in vitro [11]. Similarly, benefits of GSK-3β inhibition have been observed in ovarian [12], pancreatic [10, 13], glioblastoma [14], and colorectal [8, 9] cancer. In the present study, we further investigate the potential benefits of GSK-3β inhibition in neuroblastoma and determine whether these results translate into an in vivo model.
To inhibit GSK-3β we studied the anilinomaleimide SB415286, which inhibits GSK-3β in an ATP competitive manner. In previous studies, lithium has been most commonly used to investigate the effects of GSK-3β inhibition, but it is nonspecific and may produce results due to other kinase inhibition [15]. In contrast, the small molecule inhibitor SB415286 is potent and highly specific [16]. Although much less data has been published using this drug, it has been shown to elicit responses attributable to GSK-3β inhibition without affecting other kinases [17]. Thus, it might serve as a better tool to study GSK-3β function in neuroblastoma. We found that GSK-3β inhibition leads to reduced proliferation and increased apoptosis in neuroblastoma cells. Most importantly, we show for the first time that these effects translate into delayed tumor growth in vivo.
Materials and methods
Cell culture and GSK-3β inhibitor
Neuro-2A mouse neuroblastoma cells were established by R. J. klebe and F. H. Ruddle from a spontaneous tumor in albino strain A mice and were obtained from ATCC. The SK-N-BE (2) neuroblastoma cell line was developed by J. L. Biedler from a bone marrow biopsy. SK-N-BE (2) was obtained from ATCC. These cells express high levels of N-Myc [18, 19]. The SK-N-SH neuroblastoma cell line was developed by J. L. Biedler from a bone marrow biopsy. SK-N-SH was obtained from ATCC. These cells are deficient for N-Myc [18, 19]. Cells were maintained in DMEM with 10% FBS and 1% penicillin/streptomycin (Life Technologies, Gaithersburg, MD) and were grown in a 5% CO2 incubator at 37°C. SB415286 (3-[(3-Chloro-4-hydroxyphenyl)amino]-4-2(nitrophenyl)-(1H-pyrrole-2,5-dione) was purchased from Tocris biosciences, Ellisville, MO.
Colorimetric cell proliferation assay
Cell proliferation was determined using cell titer 96 Aqueous Non-Radioactive Cell Proliferation Assay reagent (Promega). The assay was done following the manufacturers protocol. Briefly equal numbers of Neuro-2A cells were plated into different wells of a 96-well plate and were treated with various concentrations of SB415286 for 24, 48, 72, or 96 h. Cell viability was determined colorimetrically by measuring absorbance at 490 nm. Experiments were done in triplicate and average fold changes relative to control and standard errors were calculated.
Colony formation assay
Equal amounts of Neuro-2A cells were plated on 6 cm dishes. After 4–5 h, cells were treated with either DMSO control or 25 μM SB415286. Colonies were allowed to form for 10 days after which cells were fixed with 70% ethanol and stained with 1% methylene blue. Colonies having greater than 50 cells were counted under a microscope and plotted. Experiments were repeated in triplicate and means and standard error were calculated.
Apoptosis assays
Apoptosis was measured using Annexin V-APC/propidium iodide detection kit (BD PharMingen, San Diego, CA) following the manufacturer’s protocol. Briefly, 105 Neuro-2A cells treated with DMSO or 25 μM SB415286 for 24, 28, 72, or 96 h were incubated with Annexin V-APC/propidium iodide and analyzed by flow cytometry using a two-color FACS analysis (BD LSR II). The percentage of cells staining positive for Annexin V was calculated, and means and standard error were plotted. Alternatively, apoptosis was also determined using 4′,6-diamidino-2-phenylindole (DAPI) staining. Neuro-2A cells were grown on slides and treated with either DMSO or 25 μM SB415286 for 24, 48, 72, or 96 h. After treatment, cells were washed with PBS, fixed with 4% paraformaldehyde and stained with 5 μg/ml of DAPI at room temperature for 10 min. Nuclear morphology was observed using a fluorescent microscope equipped with a digital camera. Apoptosis was quantified by counting the percentage of cells in 5–7 randomly selected high power fields (HPF) with apoptotic nuclear morphology at the single cell level. Mean and standard error were calculated for each time point and treatment group.
Immunoblot analysis
Neuro-2A cells were plated on 10 cm dishes and treated with DMSO or 25 μM SB415286 for 24, 48, 72, or 96 h. After 5 days, cells were lysed and harvested using M-PER mammalian protein extraction reagent (Pierce, Rockford, IL). Protein concentrations were quantified using BCA Reagent (Pierce, Rockford, IL) and equal amounts of protein (40 μg) were subjected to western immunoblot analysis using antibodies to beta-catenin (Cell Signaling), X-linked inhibitor of apoptosis protein (XIAP, BD Transduction Laboratories), and Bcl-2 (Santa Cruz). Antibody to actin was used to evaluate protein loading in each lane. Immunoblots were developed using the Western Lighting Chemiluminescence Plus detection system (PerkinElmer, Wellesley, MA) according to the manufacturer’s protocol.
Cell cycle analysis
Neuro-2A Cells were plated in 10 cm dishes and treated with DMSO or 25 μM SB415286 for 24, 48, 72, or 96 h. Cells were trypsinized, fixed with 70% ethanol, and incubated overnight at −20°C. Cells were pelleted and resuspended in 200 μl of PBS with 50 μl DNAase-free, RNAase A, and incubated at 37°C for 30 min. Propidium iodide (750 μl) was added and cells were incubated at room temperature for 15 min and analyzed by flow cytometry. The flow data obtained from the samples were then analysed using the software for cell cycle, Modfit LT 3.0. The average percentages of cells in G1G0 or G2-M phases of the cell cycle were quantified and standard error was calculated for three experiments.
Silencing of GSK-3β with shRNA
To identify shRNA sequences that could knockdown GSK-3β in neuroblastoma cells, we screened five MISSION shRNA clones NM_019827.2-1527s1c1 (Sigma–Aldrich, St. Louis, MO) targeted against the mouse GSK-3β sequence. MISSION shRNA clones together with packaging and envelope plasmids pUMVC and pCMV-VSV-G (provided by Sheila Stewart, Washington University), were transfected into HEK293T packaging cells using Fugene 6. At 48 h post-transfection, virus-containing media was used to infect neuroblastoma cells. GFP was used to monitor the efficiency of HEK293T transfection and infection. After selection with puromycin (1 μg/ml) for 36–48 h, cells were tested for GSK-3β expression by immunoblotting and then used for clonogenic survival assays and immunoblot analyses.
Mice, treatment, and tumor growth delay
All animal procedures used in this study were approved by the Department of Comparative Medicine (DCM) at Washington University, and the housing and handling of animals followed DCM guidelines. 5 × 106 Neuro-2A cells were injected into the right flank of nude mice. Once tumors were palpable, tumors were measured via calipers and mice were stratified into two treatment groups of 5–6 mice representing similar distributions of tumor sizes. Mice were then treated with DMSO or 1 mg/kg SB415286 i.p. once daily for 5 consecutive days. Tumor volumes were followed every day by external caliper measurements. Tumor volumes for each animal were normalized to the initial tumor volume at the start of treatment, and the mean tumor fold increase and standard error was calculated for each treatment group. The mice on day 6 treatment of DMSO were euthanized as the tumors were larger than 1000 mm3 and were not allowed by the animal protocol.
Results
GSK-3β inhibition decreases cell proliferation in neuroblastoma cell lines
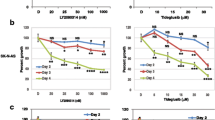
GSK-3β has been described as both a tumor promoter and a tumor suppressor depending on the cancer cell type [5]. To elucidate the role of GSK-3β in neuroblastoma, we investigated how SB415286, a selective GSK-3 inhibitor with Ki of 31 nmol/l [15], affects cell proliferation in Neuro-2a, SK-N-SH and SK-N-BE (2). Equal numbers of cells were plated in a 96 well plate and the following day treated with concentrations of 0, 1, 2.5, 5, 10, 25, 50 and 100 μM SB415286 for 24, 48, 72, or 96 h. The plates were read at 96 h using the colorimetric cell proliferation assay by measuring the absorbance at 490 nm. All three neuroblastoma cell lines showed reduction in cell proliferation after 24 h of treatment with 25 μM SB415286, with a maximum reduction at 96 h (Fig. 1 a, b, c). This anti-proliferative effect was dose and time dependent at 25, 50 and 100 μM at 24, 48, 72 and 96 h. These results indicate that inhibition of GSK-3β by small molecule inhibitors attenuates neuroblastoma cell proliferation. For further assays we used 25 μM of SB415286.
GSK-3β inhibition decreases cell proliferation in neuroblastoma cell lines. Equal numbers of neuroblastoma cells were plated in 96 well plates and treated with various concentrations of GSK-3β inhibitor SB415286 for 24, 48, 72 and 96 h. After 5 days, the cell viability was determined using a colorimetric cell proliferation assay (Promega). Shown are the absorbance at 490 nm of Neuro-2a (a), SK-N-SH (b) and SK-N-BE (2) (c)
GSK-3β inhibition reduces neuroblastoma cell survival
To determine whether GSK-3β inhibition reduces cell viability and survival of neuroblastoma cells, we performed a colony formation assay. Colony formation assay helps us determine if cells are undergoing apoptosis, necrosis, senescence, or mitotic-catastrophe leading to their inability to multiply and form colonies. Equal numbers of Neuro-2A, SK-N-SH and SK-N-BE (2) cells were plated on 6 cm dishes and treated with 25 μM SB415286 or DMSO control. A significant decrease in colony forming units was observed in all the three neuroblastoma cell lines. Specific knockdown of GSK-3β by specific shRNA in Neuro-2a, SK-N-SH and SK-N-BE (2) neuroblastoma cells showed reduced number of colonies compared to cells treated with control shRNA. These results indicate that inhibition of GSK-3β in neuroblastoma led to reduced cell viability.
GSK-3β inhibition induces apoptosis in Neuro-2A
One of the many cellular functions of GSK-3β is the regulation of apoptosis [5]. To determine whether the reduction in Neuro-2A cell proliferation and cell survival observed following GSK-3β inhibition could depend in part on the promotion of apoptosis, we used flow cytometry to stain for the apoptotic marker Annexin V. Neuro-2A cells were treated with 25 μM of SB415286 or DMSO for 24, 48, 72, or 96 h. Cells were stained with Annexin V-APC and propidium iodide, and then analyzed by flow cytometry. Apoptotic cells were identified as those that were Annexin V positive. Consistent with the cell proliferation assay (Fig. 1), no significant effects on apoptosis were observed following treatment with SB415286 for 24 h (Fig. 2b). However, the percentage of cells with apoptotic nuclei increased from 9 to 16% at 48 h, 6.3 to 10.5% at 72 h, and 5.7 to 12.4% at 96 h, illustrating that apoptosis is promoted by GSK-3β inhibition in neuroblastoma. To further confirm that GSK-3β inhibition induced apoptosis in Neuro-2A cells, we studied the nuclear morphology of cells following DAPI staining (Fig. 2c). Slides containing Neuro-2A cells were treated with 25 μM of SB415286 or DMSO for 24, 48, 72, or 96 h and subsequently stained with DAPI. The percentage of cells with apoptotic nuclei increased from 5 to 42% at 48 h, 5 to 38% at 72 h, and 3 to 50% at 96 h (Fig. 2d), confirming the induction of apoptosis following treatment. Together, these results suggest that the reduced cell survival induced during GSK-3β inhibition is associated with increased apoptosis.
GSK-3β inhibition induces cell death and apoptosis in Neuro-2A. Colony formation assay. a Neuro-2a, SK-N-SH and SK-N-BE (2) cells were inhibited for GSK-3β either using a small molecule inhibitor of GSK-3β SB415286 (25 μM) or by a specific shRNA for GSK-3β. Equal numbers of cells were plated and were stained with 1% methylene blue after 10–15 days and colonies were counted. Shown is the bar graph depicting the colony forming units (cfu). Annexin V staining. b Neuro-2A cells were treated with GSK-3β inhibitor SB415286 (25 μM) or DMSO for 24, 48, 72 or 96 h. Cells were stained with Annexin V-APC/propidium iodide and analyzed by flow cytometry. Shown is the bar graph of average percent of apoptotic cells for each treatment with SEM from three experiments; *P < 0.05. DAPI staining. c, d Neuro-2A cells were fixed and stained with DAPI, and apoptotic cells indicated by arrows were counted in multiple randomly selected fields. Shown are representative microscopic photographs (c) and a bar graph (d) of average percent of apoptotic cells vs. total cell number for each treatment with SEM from three experiments; *P < 0.05
GSK-3β reduces the expression of anti-apoptotic proteins
Neuroblastoma cell proliferation and differentiation is regulated by the induction of apoptosis [20]. It has been documented in renal cell carcinoma that GSK-3β may inhibit apoptosis by inducing the expression of anti-apoptotic proteins XIAP and Bcl-2 [21]. Immunoblotting was performed to determine if GSK-3β inhibition-induces apoptosis in Neuro-2A cells and if so whether XIAP and Bcl-2 plays a role. GSK-3β in Neuro-2A cells was inhibited either by 25 μM SB415286 or by specific shRNA to GSK-3β. The treated cell lysates were probed for XIAP and Bcl-2 using western immunoblot. Following inhibition of GSK-3β in Neuro-2A, protein levels of both of XIAP and Bcl-2 were reduced (Fig. 3a, b). This suggests that GSK-3β inhibition might induce apoptosis in neuroblastoma in part by reducing expression of the anti-apoptotic proteins XIAP and Bcl-2.
GSK-3β inhibition alters the expression of anti-apoptotic proteins. GSK-3β was inhibited in Neuro-2A cells either by treating with a small molecule inhibitor of GSK-3β SB415286 (25 μM) or with a specific shRNA for GSK-3β. Western blot analysis was performed to determine the cellular protein levels of β-catenin, XAIP and Bcl-2. Actin was used to assess protein loading in each lane
To confirm that SB415286 and specific shRNA inhibits GSK-3β function, we studied the protein expression of β-catenin, a downstream target of GSK-3β. Active GSK-3β normally phosphorylates β-catenin, leading to its degradation by the ubiquitin–proteasome system. Thus, inhibition of GSK-3β should induce the accumulation of β-catenin. β-catenin was stabilized following treatment with both SB415286 and shRNA specific to GSK-3β, confirming inhibition of GSK-3β.
GSK-3β inhibition induces the accumulation of Neuro-2A cells at G2/M
GSK-3β interacts with proteins that regulate cell cycle progression, further indicating a role for GSK-3β in cancer [11]. In fact GSK-3β inhibition can induce G2/M cell cycle arrest in colon, ovarian, and pancreatic cancer [8, 10, 12, 13]. We therefore investigated the effect of SB415286 on cell cycle parameters. Neuro-2A cells were treated with 25 μM of SB415286 or DMSO for 24, 48, 72, or 96 h. Cells were then stained with propidium iodide and analyzed by flow cytometry. Propidium iodide staining allowed us to determine the DNA content of the cells, which provides information on the percentage of cells in G0G1, S phase, and G2/M. Following GSK-3β inhibition, the percentage of cells at G2/M increased (from 11.9–21.31%, P = 0.0001) at 24 h, and this effect was continued at later time points (Fig. 4). There was also a parallel increase in the percentage of treated cells in the S phase of the cell cycle as compared to control. Conversely, the percentage of treated cells in G0G1 decreased by 24 h after treatment with SB415286 as compared to control (55.4–40.7%, respectively, P < 0.0001). This suggests that GSK-3β plays a role in cell cycle regulation and that GSK-3β inhibition induces an accumulation of Neuro-2A cells at G2/M and in the S phase of the cell cycle.
GSK-3β inhibition induces G2/M accumulation in Neuro-2A. Neuro-2A cells were treated with GSK-3β inhibitor SB415286 (25 μM) or DMSO and collected after 24, 48, 72 and 96 h, stained with and PI and analyzed by flow cytometry. Shown are a representative diagrams of distribution of stained cells and b bar graph of the average change in the percent G1G0, S-phase and G2M cells in each treatment with SEM of three experiments; *P < 0.05 (h)
GSK-3β inhibition induces neuroblastoma tumor growth delay in mice
To determine the efficacy of GSK-3β inhibition in reducing growth of neuroblastoma in vivo, a tumor growth assay was performed. Even though our in vitro results already showed promising effects of SB415286 in the treatment of Neuro-2A cells, a significant in vivo tumor growth delay provides stronger evidence of therapeutic potential. Neuro-2A cells were injected sub cutaneously into the right flanks of nude mice, and tumor-bearing mice received daily i.p injections of vehicle or SB415286 for 5 days. Tumor volume was determined by caliper measurements. As shown in Fig. 5, GSK-3β inhibition produced a significant tumor growth delay (>2 days), with effects observed by the third day of treatment.
GSK-3β inhibition results in in vivo tumor growth delay. Neuro-2A (5 × 106) were injected in the flank of nude mice and allowed to grow until palpable. Mice bearing the tumors were treated with 1 mg/kg GSK-3β inhibitor SB415286 (dark square) or DMSO (dark circle) as indicated by arrows. Tumor volume was measured every day for 6 days. The mice on day 6 treatment of DMSO were euthanized as the tumors were larger than 1000 mm3 and were not allowed by the animal protocol
Discussion
Neuroblastoma, a neoplasm of the sympathetic nervous system, is the second most common extracranial malignant tumor of childhood and the most common solid tumor of infancy. Understanding the molecular biology of neuroblastoma could help identify key targets that can efficiently be exploited therapeutically.
GSK-3β, a multifaceted kinase that regulates various cellular pathways, has been a target for drug development in the treatment of diabetes, Alzheimer’s disease and various neurological diseases [6], and has also been of interest to use against various cancers. GSK-3β inhibitors are reported to have been used against cancers like human MLL leukemia [20] renal cell carcinoma [22] colorectal cancers [8] ovarian cancer [12] and prostrate cancer [23]. In the present study we show that inhibition of GSK-3β either by small molecule inhibitor SB415286 or by a specific shRNA decreases the cell viability of a neuroblastoma cell lines Neuro-2A, SK-N-SH, and SK-N-BE (2) (Figs. 1a, b, c, 2a). The decreased viability in Neuro-2A cells can be explained by induction of apoptosis (Figs. 2b, c, d, 3 a, b) and cell cycle arrest (Fig. 4 a, b).
We further evaluated the effects of GSK-3β inhibition on cell survival and proliferation in Neuro-2A cancer cells. It has been reported that inhibition of GSK-3β leading to increased levels of β-catenin can antagonize NF-κB activity by stabilizing the β-catenin-p65 complexes that are transcriptionally active. We show that Neuro-2A cells treated with SB415286 induces accumulation of β-catenin compared to untreated controls (Fig. 3a, b), indicating that GSK-3β inhibition leads to stabilization of β-catenin that could potentially inactivate NFκB. Inhibition of GSK-3β leads to suppressed basal NFκB transcriptional activation of a subset of anti-apoptotic proteins like Bcl-2 and XIAP in pancreatic cancer cell proliferation [10]. GSK-3β has paradoxical effects on apoptosis; it inhibits extrinsic death receptor-mediated apoptosis, but promotes the mitochondrial intrinsic apoptotic pathway [24, 25]. XIAP can inhibit apoptosis by directly binding and inhibiting several caspases [26]. It has been reported that XIAP could inhibit the promotion of intrinsic apoptosis signaling by GSK-3 through binding to GSK-3 [25]. In our present study we show that inhibition of GSK-3β with SB415286 reduced Bcl-2 and XIAP proteins in Neuro-2A cancer cells (Fig. 3 a, b) consistent with the promotion of apoptosis. GSK-3β inhibition either by lithium or SB415286 has been shown to increase stabilization of anti apoptotic protein Bcl-2 and decreased amounts of pro-apoptotic protein Bax in normal hippocampal cells (HT-22). This increase in Bcl-2 protected the normal hippocampal cells from radiation induced apoptosis [27].
GSK-3β has been shown to regulate cyclin/cyclin-dependent kinases (cdk). The activity of cdks determines cell cycle progression through checkpoints, including the gap1 (G1), synthesis (S) and G2/M checkpoint eventually leading to mitosis. In the present study we also found that Neuro-2A cells, when treated with SB415286, have a prolonged S phase followed by a G2/M cell cycle arrest compared to untreated cells. This could be due to regulation of Cdc2 by GSK-3β which was shown to lead to G2/M arrest in rat B65 neuroblastoma cells.
Recently it has been shown that GSK-3β promotes the survival and proliferation of glioblastoma cells by protecting them from apoptosis [14]. In our studies, the small molecule inhibitor SB415286 repressed the growth of neuroblastoma in tumor growth studies in mice (Fig. 5). Taken together, the present data and previous studies indicate that small molecule inhibitors of GSK-3β could, after obtaining the results of clinical trials, effectively be used to treat neuroblastoma.
References
De Bernardi B, Nicolas B, Boni L, Indolfi P, Carli M, Cordero Di Montezemolo L, Donfrancesco A, Pession A, Provenzi M, di Cataldo A, Rizzo A, Tonini GP, Dallorso S, Conte M, Gambini C, Garaventa A, Bonetti F, Zanazzo A, D’Angelo P, Bruzzi P (2003) Disseminated neuroblastoma in children older than one year at diagnosis: comparable results with three consecutive high-dose protocols adopted by the Italian Co-Operative Group for Neuroblastoma. J Clin Oncol 21:1592–1601
Matthay KK, Villablanca JG, Seeger RC, Stram DO, Harris RE, Ramsay NK, Swift P, Shimada H, Black CT, Brodeur GM, Gerbing RB, Reynolds CP (1999) Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. Children’s Cancer Group. N Engl J Med 341:1165–1173
Martinez A (2008) Preclinical efficacy on GSK-3 inhibitors: towards a future generation of powerful drugs. Med Res Rev 28:773–796
Jope RS, Johnson GV (2004) The glamour and gloom of glycogen synthase kinase-3. Trends Biochem Sci 29:95–102
Luo J (2009) Glycogen synthase kinase 3beta (GSK3beta) in tumorigenesis and cancer chemotherapy. Cancer Lett 273:194–200
Rayasam GV, Tulasi VK, Sodhi R, Davis JA, Ray A (2009) Glycogen synthase kinase 3: more than a namesake. Br J Pharmacol 156:885–898
Wang L, Lin HK, Hu YC, Xie S, Yang L, Chang C (2004) Suppression of androgen receptor-mediated transactivation and cell growth by the glycogen synthase kinase 3 beta in prostate cells. J Biol Chem 279:32444–32452
Shakoori A, Ougolkov A, Yu ZW, Zhang B, Modarressi MH, Billadeau DD, Mai M, Takahashi Y, Minamoto T (2005) Deregulated GSK3beta activity in colorectal cancer: its association with tumor cell survival and proliferation. Biochem Biophys Res Commun 334:1365–1373
Shakoori A, Mai W, Miyashita K, Yasumoto K, Takahashi Y, Ooi A, Kawakami K, Minamoto T (2007) Inhibition of GSK-3 beta activity attenuates proliferation of human colon cancer cells in rodents. Cancer Sci 98:1388–1393
Ougolkov AV, Fernandez-Zapico ME, Savoy DN, Urrutia RA, Billadeau DD (2005) Glycogen synthase kinase-3beta participates in nuclear factor kappaB-mediated gene transcription and cell survival in pancreatic cancer cells. Cancer Res 65:2076–2081
Pizarro JG, Folch J, Esparza JL, Jordan J, Pallas M, Camins A (2009) A molecular study of pathways involved in the inhibition of cell proliferation in neuroblastoma B65 cells by the GSK-3 inhibitors lithium and SB-415286. J Cell Mol Med 13:3906–3917
Cao Q, Lu X, Feng YJ (2006) Glycogen synthase kinase-3beta positively regulates the proliferation of human ovarian cancer cells. Cell Res 16:671–677
Ougolkov AV, Fernandez-Zapico ME, Bilim VN, Smyrk TC, Chari ST, Billadeau DD (2006) Aberrant nuclear accumulation of glycogen synthase kinase-3beta in human pancreatic cancer: association with kinase activity and tumor dedifferentiation. Clin Cancer Res 12:5074–5081
Miyashita K, Kawakami K, Nakada M, Mai W, Shakoori A, Fujisawa H, Hayashi Y, Hamada J, Minamoto T (2009) Potential therapeutic effect of glycogen synthase kinase 3beta inhibition against human glioblastoma. Clin Cancer Res 15:887–897
Coghlan MP, Culbert AA, Cross DAE, Corcoran SL, Yates JW, Pearce NJ, Rausch OL, Murphy GJ, Carter PS, Roxbee Cox L, Mills D, Brown MJ, Haigh D, Ward RW, Smith DG, Murray KJ, Reith AD, Holder JC (2000) Selective small molecule inhibitors of glycogen synthase kinase-3 modulate glycogen metabolism and gene transcription. Chem Biol 7:793–803
Forde J, Dale T (2007) Glycogen synthase kinase 3: a key regulator of cellular fate. Cell Mol Life Sci 64:1930–1944
Martinez A, Castro A, Dorronsoro I, Alonso M (2002) Glycogen synthase kinase 3 (GSK-3) inhibitors as new promising drugs for diabetes, neurodegeneration, cancer, and inflammation. Med Res Rev 22:373–384
Cui H, Hu B, Li T, Ma J, Alam G, Gunning WT, Ding HF (2007) Bmi-1 is essential for the tumorigenicity of neuroblastoma cells. Am J Pathol 170:1370–1378
Shastry P, Basu A, Rajadhyaksha MS (2001) Neuroblastoma cell lines—a versatile in vitro model in neurobiology. Int J Neurosci 108:109–126
Brown A, Jolly P, Wei H (1998) Genistein modulates neuroblastoma cell proliferation and differentiation through induction of apoptosis and regulation of tyrosine kinase activity and N-myc expression. Carcinogenesis 19:991–997
Bilim V, Ougolkov A, Yuuki K, Naito S, Kawazoe H, Muto A, Oya M, Billadeau D, Motoyama T, Tomita Y (2009) Glycogen synthase kinase-3: a new therapeutic target in renal cell carcinoma. Br J Cancer 101:2005–2014
Wensing M, van der Weijden T, Grol R (1998) Implementing guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract 48:991–997
Mazor M, Kawano Y, Zhu H, Waxman J, Kypta RM (2004) Inhibition of glycogen synthase kinase-3 represses androgen receptor activity and prostate cancer cell growth. Oncogene 23:7882–7892
Beurel E, Jope RS (2006) The paradoxical pro- and anti-apoptotic actions of GSK3 in the intrinsic and extrinsic apoptosis signaling pathways. Prog Neurobiol 79:173–189
Sun M, Meares G, Song L, Jope RS (2009) XIAP associates with GSK3 and inhibits the promotion of intrinsic apoptotic signaling by GSK3. Cell Signal 21:1857–1865
Deveraux QL, Roy N, Stennicke HR, Van Arsdale T, Zhou Q, Srinivasula SM, Alnemri ES, Salvesen GS, Reed JC (1998) IAPs block apoptotic events induced by caspase-8 and cytochrome c by direct inhibition of distinct caspases. EMBO J 17:2215–2223
Yazlovitskaya EM, Edwards E, Thotala D, Fu A, Osusky KL, Whetsell WO Jr, Boone B, Shinohara ET, Hallahan DE (2006) Lithium treatment prevents neurocognitive deficit resulting from cranial irradiation. Cancer Res 66:11179–11186
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Amy Dickey and Stephen Schleicher contributed equally to this work.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Dickey, A., Schleicher, S., Leahy, K. et al. GSK-3β inhibition promotes cell death, apoptosis, and in vivo tumor growth delay in neuroblastoma Neuro-2A cell line. J Neurooncol 104, 145–153 (2011). https://doi.org/10.1007/s11060-010-0491-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0491-3