Abstract
Objective To evaluate perioperative management, early outcomes and hemocoagulative disorders in infants up to 1 year old, undergoing neurosurgery for brain tumors removal. Design Retrospective evaluation of prospectively collected data regarding all infants aged <1 year admitted to PICU from 1994 to 2004, following intracranial mass removal. Interventions none. Setting University Hospital PICU in a tertiary neurosurgical referral centre. Patients and participants All eligible infants were enrolled in the study. Population was constituted by 43 infants and subdivided in two groups, according to their intra-operative blood loss. Babies having blood loss exceeding the preoperative estimated volemia were classified in group A; the remaining babies were included in group B. Results Intraoperative transfusions, PICU length of stay, need for post-operative mechanical ventilation and cardiovascular support were all significantly higher in group A than in group B. No early postoperative mortality occurred. ROC analysis and multiple logistic regression showed the age as the only variable independently associated with blood loss exceeding preoperative volemia (cut-off 60.3 days; OR = 0.11, CI 0.02–0.55, sensitivity 82.4%; specificity 67%). Postoperatively, platelet count, prothrombin activity and fibrinogen resulted significantly depressed in group A, representing a dilutional coagulopathy. A marked dispersion of aPTT values was recorded in group B, where most infants exhibit aPTT shortening, suggesting a hypercoagulability status. Three episodes of clinical disseminated intravascular coagulation (DIC) were registered in group B. Conclusions We illustrated the relationships between intraoperative blood loss, transfusions and haemostatic impairment in babies following brain tumor removal. Youngest infants had the higher risk to experience hemocoagulative disorders. These infants showed significantly higher impact on the global PICU burden of care, as represented by the need of mechanical ventilation, cardiovascular support and PICU length of stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central nervous system tumors are the second most common malignancy in childhood, with estimated incidence of 1.1/100.000 live births representing 1/3 of the total cancer incidence below 16 years. Approximately 7–17% of pediatric brain tumors occur in children less than 2 years old: survival rate in this age group is significantly worse than in older children [1]. Improved neuroimaging, surgical, neuro-oncological and pediatric intensive care make reasonable the attempt of a more aggressive tumor resection. Hemostatic and coagulative defects are commonly observed in critical patients [2], including those undergoing neurosurgery, ranging from isolated thrombocytopenia through Disseminated Intravascular Coagulation (DIC). In pediatric neurointensive care DIC is often associated with severe head trauma and primary or metastatic brain malignancy. To date, only one infant case of fatal coagulative dysfunction following brain tumor surgery has been described [3]. On the other hand, the occurrence of exsanguinating hemorrhage in infants and young children is well known, as is the related hemostatic impairment. Recently, some authors suggested the utilisation of activated factor VII to control life-threatening bleeding during tumor removal [4, 5].
To date, no surveys are available about the intensive management and perioperative complications in infants undergoing brain tumor removal. Aim of our prospective study was to analyse the early clinical outcome, perioperative complications and haemocoagulative disorders of infants up to 1 year old, undergoing neurosurgery for brain tumors.
Patients and methods
Patients
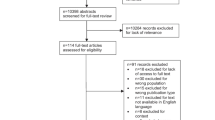
From January 1994 to January 2004 over 250 infants aged <1 year were admitted to the Pediatric Intensive Care Unit (PICU) of the “A. Gemelli” University Hospital at the Catholic University of Rome, following a major neurosurgical procedure. We prospectively collected perioperative data and early clinical outcome of the 43 (17% of all neurosurgical admissions) infants who suffered from cerebral neoplasms. Mortality was defined as early when occurring within 7 days after the surgical procedure and late if between 7 and 30 days. We analyse their intraoperative blood loss as described below and we electively assign patients to group A (babies suffering from massive blood loss) or group B (babies with blood loss smaller than preoperative estimated volemia).
Hematological and coagulative assessment
Hematocrit (Hct), prothrombin activity (PT), activated partial thromboplastin time (aPTT), fibrinogen concentration and platelet count were measured both preoperatively and postoperatively, within 1 h from PICU admission, and every 12 h subsequently. Red cell volume was calculated as follows: estimated red cell volume (ERCV) = [estimated blood volume (EBV) × Hct/100]. Transfused blood volume was estimated as follows: estimated red cell volume transfused (ERCT) = 0.6 (mean hematocrit of packed red cells units) × PBRC, where PBRC is the transfused volume of packed blood red cells.
We then considered blood loss using the two following formulae: estimated red cell volume loss (ERCL) = [(preoperative ERCV − postoperative ERCV) + ERCT]; ERCL ratio = ERCL/preoperative ERCV. Infants with ERCL ratio >1 were considered to have blood loss exceeding the preoperative estimated volemia and classified in group A; the remaining babies were included in group B.
PICU transfusions in the early postoperative period (within 72 h from admission) were also recorded. Even in the presence of serious bleeding, replacement was aimed to maintain a safe hematocrit level (within 28 and 32%) and a central venous pressure (CVP) within 6 and 8 cm H2O. The impact of neurosurgical procedure and blood transfusions on coagulative status was evaluated through serial platelet counts and coagulation tests.
Treatment protocol/surgical management
All infants received standardised neurosurgical and intensive care management by the same group of neurosurgeons, neuroanesthesists and pediatric intensivists, operating in close coordination.
-
(a)
Anaesthesia management General anaesthesia was induced through a face-mask with sevoflurane (6–8%) and O2 in not cooperating patients, whereas thiopentone (3–4 mg/kg) or propofol (2 mg/kg) were administered to older children. Two lines were positioned into large size peripheral veins (mostly large saphenous vein) together with a central venous line (22 gauges) in the internal jugular vein. Central venous access was always achieved through echo-guided procedures. Heart rate (HR), invasive arterial blood pressure (IABP), CVP, superior vein cava mixed venous saturation (scvSvO2), pulse-oximetry (SpO2), end-tidal halogenated agents concentration (EtHA), EtCO2, spirometry, peripheral versus core temperature, urine output, acid-base status (including arterial lactate concentration) and Hb/Hct/Platelet count, were sistematically monitored. Body temperature was maintained by hot air warming mattress; fluid infusions were warmed by thermostatic system. Muscular relaxation was obtained by vecuronium bromide (0.07 mg/kg) or cisatracurium (0.1 mg/kg bolus, 2 mcg/kg/min continuous infusion). General anaesthesia was maintained by isoflurane (MAC 1) or sevoflurane (MAC 1.5) and fentanyl (1–2 mcg/kg/h) according to patient demand while ventilation was performed through Servo Ventilator 900 C (Maquet Critical Care, Solna, Sweden) or Datex Aestiva (Datex, Helsinki, Finland) on volume controlled mode.
-
(b)
Fluid infusions and transfusions Fluid infusions were maintained at a constant rate (4 ml/kg/h) until dural opening, subsequently infusion rate was modified according to hemodynamic and metabolic data. No hypotonic or glucose solutions were administered during surgery for possible worsening of ischemic perilesional damage. A strict control of fluids input/output and related hemodynamic parameters (HR, IABP, CVP, scvSvO2) was performed: during and after surgery all efforts were made to maintain a satisfying arterial pressure using an aggressive volume management with saline, colloids and blood transfusions (if Hct fell below 28–30%). Colloid solutions (15–20 ml/kg of 6% hydroxyethil starch, then 5% human albumin) were given to replace blood loss and maintain patient volemia. Pharmacological support was frequently titrated using dopamine (3–8 mcg/kg/min) or dobutamine (5–15 mcg/kg/min) and epinephrine (0.1–0.5 mcg/kg/min). In addition, when O2 delivery was deemed insufficient to support tissue metabolism (on the basis of clinical and laboratory data, as scvSvO2 and lactate trend), PBRC were transfused to restore Hct. Fresh frozen plasma (10–15 ml/kg) was given when PT and aPTT were 1.5 longer than normal values, according to international guidelines [6]. ATIII concentrate was administered when its plasma level was <70%, whereas platelet concentrates were given if platelet count fell below 50,000/μl. To prevent venous air embolism head position was carefully assessed during surgery. All children were intubated with cuffed tubes and in all patients EtCO2 was strictly monitored. No patient received N2O administration in order to avoid cuff pressure increases.
-
(c)
Respiratory support On PICU admission the infants were electively mechanically ventilated: ventilation mode was always Pressure Regulated Volume Control with tidal volume of 7–8 ml/kg and PEEP level was kept <4 cmH2O; Servo300 and Servo-I (Maquet Critical Care, Solna, Sweden) ventilators were used. Target PaCO2 levels were 38–42 mmHg unless intracranial hypertension was detected on intracranial pressure (ICP) monitoring; CO2 level was always measured with EtCO2 or transcutaneous monitoring. Active humidification was adopted. Mechanical ventilation was electively maintained until the child appeared awake and neurological competent enough to protect the airway and ensure stable respiratory drive (eye opening and gag reflexes presence were mandatory). In selected cases, after extubation, non-invasive ventilation was used to avoid early reintubation or lung atelectasis: a full face mask was used and ventilator settings were on Pressure Control mode to minimize air leaks.
-
(d)
PICU management The treatment protocol is based on the need to ensure an adequate cerebral perfusion pressure (CPP) by sustaining the cerebral circulation and minimizing brain oedema: we adopted the threshold of 45 mmHg. More sophisticated neurophysiological monitoring (e.g., continuous ICP tracing, prolonged EEG recording, somatosensory or auditory evoked potentials, transcranial Doppler ultrasound) have been performed in selected cases. Ventilated infants received an analgesia-sedation scheme including midazolam 1–4 mcg/kg/min and remifentanil 0.25–0.5 mcg/kg/min. Muscle-relaxation has been avoided in the postoperative period. Barbiturate load (phenobarbital 20 mg/kg) and subsequent maintenance therapy was generally indicated in supratentorial tumour surgery. Electrophysiological monitoring was performed in selected cases in order to optimize the anticonvulsant treatment.
Statistical analysis
Proportions were contrasted using Fisher’s test and continuous variables were compared using Student’s t test. Receiver operator characteristic (ROC) analysis were conducted in the whole population to evaluate the reliability of age, body weight and preoperative ERCV in predicting Group A inclusion, i.e. the probability of suffering a massive blood loss. When the area under the ROC curve was >0.5, the best cut-off value was calculated. Logistic regression was also used to detect factors influencing ERCV loss >1 (group A entry). Variables included in the model were patient age, body weight, preoperative ERCV. Multivariate analysis was performed using backward-stepwise technique and goodness of fit was tested using Hosmer and Lemeshow test.
Post-operative ventilation times were analysed using the Kaplan–Mayer method and Tarone–Ware’s test. All statistical analyses were performed using SPSS for Windows rel. 12.0 (SPSS Corp. Ltd., Chicago, IL, USA) and P-values < 0.05 were considered as statistically significant.
Results
Population (mean age 146.37 ± 106.4 days; mean body weight 5.884 ± 2.154 kg; M/F ratio 1.38) data are summarized in Tables 1 and 2. The mean PICU stay was 7.6 ± 8.1 days, whereas the mean duration of respiratory support was 58.5 ± 97.4 h. One patient was discharged home on nocturnal mechanical ventilation. No early postoperative mortality was observed (two infants died before the 30th postoperative day for tumour progression). Clinical DIC (3 cases) were registered in group B only. No correlations were found between tumor histology and both hemocoagulative impairment and PICU burden of care.
Mean age (47.3 ± 33.6 days) and body weight (4.1 ± 0.9 kg) were significantly lower in group A than in group B (both P < 0.01). PICU length of stay, need for POMV, cardiovascular support such as blood loss and transfusion demand were all significantly higher in group A. Mean ERCL Ratio in the whole population was 0.93 ± 1.09 ml, while group A babies showed a mean ERCL Ratio of 2.64 ± 1.33. Group B ERCL ratio was 0.48 ± 0.23. ERCT was significantly higher in group A than in group B (248.7 ± 123.7 vs. 72.33 ± 65.44; P < 0.001).
Haematological and coagulative parameters and their modifications in Group A infants are described in Table 3 .
ROC analysis provided cut-off values of infants’ age, body weight and preoperative ERCV for the group A inclusion being patient age the only variable indipendently associated with ERCL Ratio > 1 (cut-off 60.5 days; OR = 0.11, CI 0.02–0.55; Hosmer and Lemeshow test P = 0.685) (Table 4 ).
Perioperative variations of hemostasis parameters in groups A and B are showed in Fig. 1. A marked dispersion of aPTT values was recorded in group B, where most infants exhibit aPTT shortening (P < 0.05), suggesting a hypercoagulability status (Fig. 1).
Perioperative variations of hemostasis parameters in groups A and B. Preoperative and postoperative values are represented by numbers 1 and 2, respectively. Graph (a and b) main coagulative tests modifications in the perioperative period in Group A vs. Group B infants; Graph (c): aPTT shortening or prolongation in the postoperative period; Graph (d) platelet count decrease in Group A vs. Group B infants. (#, n.s.; §, P < 0.01)
Figure 2 shows Kaplan–Mayer analysis of PICU ventilatory support with POMV significantly longer in group A (P = 0.008). Accordingly, post-operative ventilator-free time was significantly larger in group B (P = 0.003).
Mechanical ventilation need in PICU: the full and dashed lines represent group A and group B, respectively. Graph (a) Post-operative mechanical ventilation days (POMVD) (§, P = 0.008). Graph (b) Post-operative mechanical ventilation free days as percent of the total PICU stay (MVfree%) (#, P = 0.003)
Discussion
Our experience shows a high prevalence of massive blood loss in young infants undergoing intracranial tumor surgery, a younger age (<2 months) at intervention being the best predictive factor. Severe bleeding represents a major risk for this patient population. In fact, although in our case series no related mortality has been observed, babies suffering from massive blood loos have a significantly longer PICU stay and a higher need for mechanical ventilation and cardiovascular support. They also have a significantly increased incidence of hemostasis impairment.
Although we have a relatively small population an interesting trend toward a hypercoagulable condition exists for infants having low to moderate degree blood loss.
Survival of infants with brain tumors has increased in the recent years due to advances in surgical techniques, radiotherapy and, where applicable, chemotherapy [1, 7]. Unfortunately, the prognosis under 12 months of age remains severe. In all neurosurgical series, survival depended primarily on the histology, the delay of diagnosis and the possibility of complete resection [8] with a perioperative mortality ranging from 19 to 33% [9, 10]. In the recent years, operative morbidity and mortality, while improving, remain significant and bleeding-related [1, 10–12].
Hemorrhage plays therefore a key role in both perioperative mortality and morbidity and massive blood transfusion is not infrequent. In fact, babies are very sensitive to blood loss and fluid/electrolyte derangements, as well as to hypothermia. All these factors are consistent with such prolonged and invasive surgery, inducing a profound autonomic instability and vasopressors hyporesponsiveness. When blood loss approaches 50–75% of the pre-operative volemia (or 40–60 ml/kg), some coagulative impairment is likely to appear. At this level of loss, serum prothrombin and partial thromboplastin times should be obtained and fresh frozen plasma given if necessary [6]. Regarding coagulative consequences, two distinct and opposite effects on blood coagulation have been described: first, a certain degree of hypercoagulability both in clinical [13] and in laboratory studies [14–16]; second, coagulopathy due to factors depletion invariably occurs when hemorrhage comes close to 100% of EBV [17]. Moreover, also hemodilution-related hypercoagulability may play a role [18, 19]. These effects have been confirmed in adult as well as in pediatric studies [20–22]. It appears that several brain injuries, including brain neoplasms, are able to profoundly influence the coagulation/anticoagulation balance [23–25].
In our 10-year experience we observed 3 (6.5%) cases of clinical DIC, all leading to a marked increase in PICU length of stay. DIC has been rarely reported in association with elective brain tumor surgery [26, 27]. Only one description exists about this association in children [3]. In contrast, DIC is relatively common in head-injured patients also in pediatric age, reflecting the severity of the brain injury [28], as brain is particularly rich in thromboplastin [29, 30]. As a whole, intracranial surgery has been shown to be associated with higher incidence of coagulation disorders compared to general surgical procedures [13, 30, 31].
As illustrated, any brain surgery or trauma with catastrophic blood loss and resultant replacement may cause coagulation abnormalities and impaired thrombin generation especially in young children where blood loss may easily overcome the patient volemia. In our series, 9/43 infants underwent massive blood transfusion i.e., EBL > 1 EBV) within a 24-h period. Massive transfusions have been related to cardiovascular instability, pulmonary dysfunction, metabolic derangements, increased incidence of infections but, most importantly, to perioperative coagulopathy. A DIC may occur in up to 30% of patients during a massive blood transfusion [32].
Alterations of the hemostatic network are commonly reported in intensive care patients (somehow independently from the cause of ICU admission) [2]. Therefore it is not surprising that a well defined subset of infants undergoing simultaneously a major intracranial surgery and an important blood loss, can undergo serious hemocoagulative derangements. Hemostatic imbalances are likely to occur because of the excessive bleeding or multiple activation of inflammatory pathways with subsequent shift towards procoagulation and down-regulation of anticoagulant pathways.
In our series, DIC was observed only in three babies who did not experience massive blood loos and so a link between DIC triggering and the extent of intraoperative blood loss could not be established. We can suppose that, under certain conditions, the reduction of the platelet count and coagulation factors can be due not only to hemodilution but to the tumor itself which can trigger the clotting dysfunction; tumor-related hypercoagulability is often difficult to declare and may be self-limiting. The net effect of the balance between hypocoagulability and hypercoagulability is unpredictable in the individual patient. It could also be argued that infants undergoing moderate to severe blood losses (as in group B) can be more exposed to prothrombotic events and, eventually, can be more prone to develop DIC. The tendency towards an aPTT shortening seems to confirm this hypothesis [13, 16]. Further multicentric studies are warranted to confirm these preliminary data and to identify a possible patient subset at higher risk for prothrombotic events.
The issue of antithrombotic therapy (i.e. antithrombin supplementation), mostly in the presence of deep hemodilution, is currently debated. Ruttmann recommended its use when plasma level is <70% to prevent thrombotic intravascular phenomena [33–36]. More recently, Nishiyama confirmed that antithrombin could decrease hypercoagulation and inflammatory activation response during major surgery leading to a decrease of the adverse events [36]: these considerations may support the use of other and more effective antithrombotic agents.
Recommendations
Circulating blood volume control
An adequate control of the patient volemia is crucial for the perioperative management of these young patients: it is based on the careful evaluation of instrumental, laboratoristic and clinical data such as HR, IBP and SpO2 values and waveform, CVP, EtCO2, ABS, fluid balance. Infants must be well oxygenated, with body temperature and pain stress under control. Rapid access to a reliable estimate of Hb/Hct and to PBRC and blood products, when required, must be guaranteed. ABS should be determined repeatedly to detect increased concentrations of lactic acid and metabolic acidosis (pH < 7.3; base excess < − 6), both revealing inadequate DO2. The serial control of SVCSvO2 and its comparison with arterial gas analysis can help to assess the patient metabolic status. Blood loss evaluation by surgical drains and draps is poorly related to the Hb/Hct values: when signs of inadequate DO2 appear, a PRBC trasfusion is mandatory to guarantee tissue oxygen demand. At the end of the surgical procedure, the infant is referred to PICU so that all vital parameters can be monitored closely until stabilization. Beyond the above measures, an early transthoracic 2D-echocardiogram assessment is obtained.
Coagulation assessment practice
Preoperative coagulation screening is mandatory, including antithrombin and D-dimer levels: a subclinical coagulative dysfunction should be evidenced early, before the masquerading effect of IOBL. Of particular importance, even minor aPTT prolongation should be studied in depth, as some possibly severe conditions can be diagnosed in advance (e.g., factor VII deficiency, anticardiolipin antibodies, lupus anticoagulant).
The key point is the “monitoring of the clotting function” in the perioperative period As coagulative derangement is strictly dependent on the degree of blood loss, the anesthesiologist should be able to assess it over time (i.e. ERCL ratio while maintaining normovolemia). According to international guidelines [6, 37] critical time points should be considered when EBL approaches 70% (early laboratory signs), 100% (likely to require FFP supply) and 150% (PLT need) of patient EBV, respectively. A timely diagnosis/treatment of clotting dysfunction is crucial for a successful management strategy.
Our practice includes the early intraoperative correction of ongoing antithrombin deficits [34–36], contributing to platelets circulating pool preservation. As a clinical rule, coagulation factors replacement is performed when PT or aPTT exceed 1.5 times the normal range, then FFP is supplied yet intraoperatively (10–15 ml Kg−1 see Table 3) [6]. A rapid coagulation overview can be obtained using thromboelastography, which is increasingly used at our institution [16]. In all cases, a coagulation check is obtained before RBC concentrate transfusion (when necessary), at dural closure (end of surgery) and soon after PICU admission. In selected cases, when a massive platelet consumption occurs, coagulation protein C and protein S levels are detected, and a protein C concentrate supply can be required.
Abbreviations
- ABS:
-
Acid-base status
- AT3:
-
Antithrombin III
- CVP:
-
Central venous pressure
- DIC:
-
Disseminated intravascular coagulation
- DO2 :
-
Oxygen delivery
- EBV:
-
Estimated blood volemia
- ERCL:
-
Estimated red cell volume loss
- ERCT:
-
Estimated red cell volume transfused
- ERCV:
-
Estimated red cell volume
- EtCO2:
-
End-tidal CO2
- EtHA:
-
End tidal halogenated agents
- FFP:
-
Fresh frozen plasma
- Fibr:
-
Fibrinogen
- Hb:
-
Hemoglobin
- HR:
-
Heart rate
- Htc:
-
Hematocrit
- IABP:
-
Invasive arterial blood pressure
- MAC:
-
Minimal alveolar concentration
- MBT:
-
Massive blood transfusion
- PBRC:
-
Packed blood red cells
- POMV:
-
Post-operative mechanical ventilation
- PICU:
-
Pediatric intensive care unit
- scvSvO2:
-
Superior caval vein mixed venous saturation
- SpO2:
-
Arterial oxygen saturation
References
Rivera-Luna R, Medina-Sanson A, Leal-Leal C, Pantoja-Guillen F, Zapata-Tarres M, Cardenas-Cardos R (2003) Brain tumors in children under 1 year of age: emphasis on the relationship of prognostic factors. Childs Nerv Syst 19:311–314
Boldt J, Papsdorf M, Rothe A, Kumle B, Piper S (2000) Changes of the hemostatic network in critically ill patients—is there a difference between sepsis, trauma, and neurosurgery patients? Crit Care Med 28:445–450
Huang PS, Koo KE (1990) Diffuse intravascular coagulation associated with brain tumor surgery in children. Pediatr Neurosurg 16:43–47
Hartmann M, Sucker C, Messing M (2006) Recombinant activated factor VII in the treatment of near-fatal bleeding during pediatric brain tumor surgery. Report of two cases and review of the literature. J Neurosurg 104:55–58
Heisel M, Nagib M, Madsen L, Alshiekh M, Bendel A (2004) Use of recombinant factor VIIa (rFVIIa) to control intraoperative bleeding in pediatric brain tumor patients. Pediatr Blood Cancer 43:703–705
O’Shaughnessy DF, Atterbury C, Bolton MP, Murphy M, Thomas D, Yates S (2004) Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol 126:11–28
Duffner PK, Cohen ME (1985) Treatment of brain tumors in babies and very young children. Pediatr Neurosci 12:304–310
Brown K, Mapstone TB, Oakes WJ (1997) A modern analysis of intracranial tumors of infancy. Pediatr Neurosurg 26:25–32
Raimondi AJ, Tomita T (1983) Brain tumors during the first year of life. Childs Brain 10:193–207
Jooma R, Hayward RD, Grant DN (1984) Intracranial neoplasms during the first year of life: analysis of one hundred consecutive cases. Neurosurgery 14:31–41
el Mahdy W, Kane PJ, Powell MP, Crockard HA (1999) Spinal intradural tumours: part I—extramedullary. Br J Neurosurg 13:550–557
Di Rocco C, Ceddia A, Iannelli A (1993) Intracranial tumours in the first year of life A report on 51 cases. Acta Neurochir (Wien) 123:14–24
Iberti TJ, Miller M, Abalos A, Fischer EP, Post KD, Benjamin E (1994) Abnormal coagulation profile in brain tumor patients during surgery. Neurosurgery 34:389–394
Abrahams JM, Torchia MB, McGarvey M, Putt M, Baranov D, Sinson GP (2002) Perioperative assessment of coagulability in neurosurgical patients using thromboelastography. Surg Neurol 58:5–11
Tuman KJ, Spiess BD, McCarthy RJ, Ivankovich AD (1987) Effects of progressive blood loss on coagulation as measured by thrombelastography. Anesth Analg 66:856–863
Goobie SM, Soriano SG, Zurakowski D, McGowan FX, Rockoff MA (2001) Hemostatic changes in pediatric neurosurgical patients as evaluated by thrombelastograph. Anesth Analg 93:887–892
Williams GD, Ellenbogen RG, Gruss JS (2001) Abnormal coagulation during pediatric craniofacial surgery. Pediatr Neurosurg 35:5–12
Ng KF, Lam CC, Chan LC (2002) In vivo effect of haemodilution with saline on coagulation: a randomized controlled trial. Br J Anaesth 88:475–480
Ruttmann TG (2002) Haemodilution enhances coagulation. Br J Anaesth 88:470–472
Hsieh V, Molnar I, Ramadan A, Safran AB, Bouvier CA, Berney J (1986) Hypercoagulability syndrome associated with cerebral lesions. Prospective study of coagulation during surgery of primary brain tumors (17 cases). Neurochirurgie 32:404–409
Goh KY, Tsoi WC, Feng CS, Wickham N, Poon WS (1997) Haemostatic changes during surgery for primary brain tumours. J Neurol Neurosurg Psychiatr 63:334–338
Kornowski R, Pines A, Constantini S (1993) Persistent activation of thrombocytes in neurosurgical patients operated for primary brain tumours. Acta Neurochir (Wien) 121:146–148
Goodnight SH, Kenoyer G, Rapaport SI, Patch MJ, Lee JA, Kurze T (1974) Defibrination after brain-tissue destruction: a serious complication of head injury. N Engl J Med 290:1043–1047
Rogers LR (2003) Cerebrovascular complications in cancer patients. Neurol Clin 21:167–192
Sawaya R, Cummins CJ, Kornblith PL (1984) Brain tumors and plasmin inhibitors. Neurosurgery 15:795–800
Berger MM, Ravussin P, Vielle G, Fankhauser H (1995) Life-threatening hemorrhagic diathesis due to disseminated intravascular coagulation during elective brain tumor surgery. J Neurosurg Anesthesiol 7:26–29
Matjasko MJ, Ducker TB (1977) Disseminated intravascular coagulation associated with removal of a primary brain tumor. Case report. J Neurosurg 47:476–480
Miner ME, Kaufman HH, Graham SH, Haar FH, Gildenberg PL (1982) Disseminated intravascular coagulation fibrinolytic syndrome following head injury in children: frequency and prognostic implications. J Pediatr 100:687–691
Astrup T (1965) Assay and content of tissue thromboplastin in different organs. Thromb Diath Haemorrh 14:401–416
Prasad KS, Sharma BS, Marwaha N, Sarode RS, Kak VK (1994) Haemostatic derangement in patients with intracranial tumours. Br J Neurosurg 8:695–702
van der Sande JJ, Veltkamp JJ, Bouwhuis-Hoogerwerf ML (1983) Hemostasis and intracranial surgery. J Neurosurg 58:693–698
Mannucci PM, Federici AB, Sirchia G (1982) Hemostasis testing during massive blood replacement. A study of 172 cases. Vox Sang 42:113–123
Ruttmann TG, Montoya-Pelaez LF, James MF (2007) The coagulation changes induced by rapid in vivo crystalloid infusion are attenuated when magnesium is kept at the upper limit of normal. Anesth Analg 104(6):1475–1480
Nielsen VG, Lyerly RT, Gurley WQ (2004) The effect of dilution on plasma coagulation kinetics determined by thrombelastography is dependent on antithrombin activity and mode of activation. Anesth Analg 99:1587–1592
Ruttmann TG, Jamest MF, Lombard EH (2001) Haemodilution-induced enhancement of coagulation is attenuated in vitro by restoring antithrombin III to pre-dilution concentrations. Anaesth Intensive Care 29:489–493
Nishiyama T (2006) Antithrombin can modulate coagulation, cytokine production, and expression of adhesion molecules in abdominal aortic aneurysm repair surgery. Anesth Analg 102:1007–1011
Task Force on blood component therapy (1996) Practice guidelines for blood component therapy: a report by the American society of anesthesiologists task force on blood component therapy. Anesthesiology 84(3):732–747
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Piastra, M., Di Rocco, C., Caresta, E. et al. Blood loss and short-term outcome of infants undergoing brain tumour removal. J Neurooncol 90, 191–200 (2008). https://doi.org/10.1007/s11060-008-9643-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9643-0