Abstract
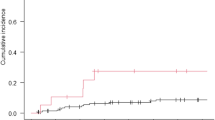
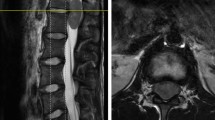
Background Recent reports on large number of patients with brain metastases report that Whole Brain Radiotherapy (WBRT) and Radiosurgery (RS) should be the treatments of choice, particularly in multiple lesions cases. Among the prognostic factors, the cerebellar location was never considered, although this results in hydrocephalus, brain stem compression, ataxia, intracranial hypertension. Materials and methods We evaluated 44 patients with cerebellar metastases operated over 6 years. Primary lesions were: Lung (15), Breast (12), Gastrointestinal (9), Gut (3), Ovary (2), Melanoma (1), Salivary gland carcinoma (1), Unknown (1). Lesions were <3 cm in 11 cases, ≥3 cm in 33. Average KPS scoring at admission was 69.9. Twenty nine scored ≥70, 15 < 70. Results Two patients died for surgical complications, 2 died within 1 months for other causes, 2 were lost to follow up. Eight had postoperative hematoma requiring reoperation, 1 had an occipital infarction. Average KPS scoring at discharge was 76.4, P < 0.002. Those patients that had complications scored less, the difference is significant (P < 0.008). Median survival was 8 months, 1 year survival rate 29.9%. Survival was correlated with either admission or discharge KPS (≥70 vs. <70): P = 0.05 and P = 0.0001 respectively. None of the other parameters considered reached statistical significance. Conclusions Open microneurosurgery is probably still the most effective therapy in improving survival and KPS in patients with large cerebellar metastases, given that the proper surgical technique is used and that complications do not occur. Specific data on cerebellar metastases as an independent subgroup are needed from radiosurgical series.

Similar content being viewed by others
References
Andrews DW, Scott CB, Sperduto PW et al (2004) Whole brain radiation therapy with or without radiosurgery boost for patients with one to three brain metastases: phase III study of the RTOG 9508 randomized trial. Lancet 363:1665–1672
Cairncross JG, Kim JH, Posner JB (1980) Radiation therapy for brain metastases. Ann Neurol 17:529–541
Black PM, Johnson MD (2004) Surgical resection for patients with solid brain metastases: current status. J Neurooncol 69:119–124
Kondziolka D, Lunsford LD (1993) Brain metastases. In: Apuzzo MLJ (ed) Brain surgery, complication avoidance and management, vol 1. Churchill Livingston, New York, pp 615–641
Kondziolka D, Patel A, Lunsford LD et al (1999) Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 45:427–434
Sneed PK, Suh JH, Goetsch SJ et al (2002) A multi-institutional review of radiosurgery alone vs. radiosurgery with whole brain radiotherapy as the initial management of brain metastases. Int J Radiat Oncol Biol Phys 53:519–526
Sanghavi SN, Miranpuri SS, Chappell R et al (2001) Radiosurgery for patients with brain metastases: a multi-istitutional analysis stratifies by the RTOG recursive partitioning analyses method. Int J Radiat Oncol Biol Phys 51:426–434
Gaspar LE, Scott C, Murray K, Curran W (2000) Validation of the RTOG recursive partitioning analysis (RPA) classification for brain metastases. Int J Radiat Oncol Biol Phys 47:745–751
Vecht CJ, Haaxma-Reiche H, Noordijk EM et al (1993) Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 33:583–590
Bindal AK, Bindal RK, Hess KR et al (1996) Surgery versus radiosurgery in the treatment of brain metastases. J Neurosurg 84:748–754
Noordijk EM, Vecht CJ, Haaxma-Reiche H et al (1994) The choice of treatment of single brain metastases should be based on extracranial tumor activity, and age. Int J Radiat Oncol Biol Phys 29:711–717
Patchell R, Tibbs PA, Walsh JW et al (1990) A randomised trial of surgery in the treatment of single metastases to the brain. N Engl J Med 332:494–500
Wronski M, Arbit E, Burt M, Galicich JH (1995) Survival after surgical treatment of brain metastases from lung cancer: a follow up study of 231 patients treated between 1976 and 1991. J Neurosurg 83:605–616
Wronsky M, Arbit E (1999) Resection of brain metastases from colorectal carcinoma in 73 patients. Cancer 85:1677–1685
Ampil FL, Nanda A, Willis BK, Nandy I, Meehan R (1996) Metastatic disease to the cerebellum: the LSU experience in 1981–1993. Am J Clin Oncol 19:509–511
Fadul C, Misulis KE, Wiley RG (1987) Cerebellar metastases: diagnostic and management considerations. J Clin Oncol 5:1107–1115
Weisberg LA (1985) Solitary cerebellar metastases. Arch Neurol 42:336–341
Shirane R, Kumabe T, Yoshida Y et al (2001) Surgical treatment of posterior fossa tumors via the occipital transtentorial approach: evaluation of operative safety and results in 14 patients with anterosuperior cerebellar tumors. J Neurosurg 94:927–935
Pompili A, Pace A, Occhipinti E (2006) Subtemporal transtentorial approach. J Neurosurg 104:854–855 (Letter)
Kuo MF, Tu YK, Lin SM (1992) Solitary cerebellar metastases: analysis of 11 cases. J Formos Med Ass 91:1010–1012
Smalley SR, Schray MF, Laws ER Jr, O’Fallon JR (1987) Adjuvant radiation therapy after surgical resection of solitary brain metastasis: association with pattern of failure and survival. Int J Radiat Oncol Biol Phys 13:1611–1616
Warnick RE, Darakchiev BJ, Breneman JC (2004) Stereotactic radiosurgery for patients with solid brain metastases: current status. J Neurooncol 69:125–137
Rock J, Haines S, Recht L (2000) Practice parameters for the management of single brain metastases. Neurosurg Focus 9:1–9
Auchter RM, Lamond JP, Alexander E et al (1996) A multinstitutional outcome and prognostic factor analysis of radiosurgery for resectable single brain metastases. Int J Radiat Oncol Biol Phys 35:27–35
O’Neill BP, Iturria NJ, Link MJ et al (2003) A comparison of surgical resection and stereotactic radiosurgery in the treatment of solitary brain metastases. Int J Radiat Oncol Biol Phys 55:1169–1176
Gerosa M, Nicolato A, Foroni R, Tomazzoli L, Bricolo A (2005) Analysis of long-term outcomes and prognostic factors in patients with non-small cell lung cancer brain metastases treated by gamma knife radiosurgery. J Neurosurg 102(Suppl):75–80
Pan HC, Sherman J, Stroila M, Steiner M, Steiner L (2005) Gamma Knife surgery for brain metastases from lung cancer. J Neurosurg 102(Suppl):128–133
Yu CP, Cheung JYC, Chan JFK, Leung SCL, Ho RTK (2005) Prolonged survival in a subgroup of patients with brain metastases treated by gamma knife surgery. J Neurosurg 102(Suppl):262–265
Regine WF, Rogozinska A, Kryscio RJ, Tibbs PA, Young AB, Patchell RA (2004) Recursive partitionaning analysis classification I and II: applicability evaluated in a randomized trial for resected single brain metastases. Am J Clin Oncol 27:505–509
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pompili, A., Carapella, C.M., Cattani, F. et al. Metastases to the cerebellum. Results and prognostic factors in a consecutive series of 44 operated patients. J Neurooncol 88, 331–337 (2008). https://doi.org/10.1007/s11060-008-9572-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9572-y