Abstract
Introduction
Otomycosis is a superficial infection of the external ear caused by fungal pathogens. The genera Aspergillus and Candida are considered the main fungal causative agents, with the predominance of Aspergillus section Nigri. The present study aimed to evaluate the clinical symptoms of patients with otomycosis and predisposing factors and to identify fungal etiological agents using molecular approaches. We also present an overview of published papers on tympanic membrane perforation (TMP) secondary to otomycosis.
Materials and Methods
An otorhinolaryngologist collected specimens from external ear canals of patients with suspected otomycosis based on the patient’s history and clinical examinations. The specimens were collected using sterile swabs. Fungal isolates were confirmed in clinical specimens by direct microscopy and culture methods. Fungal isolates were identified based on molecular approaches.
Results
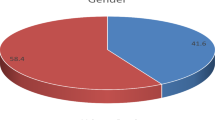
In total, specimens from 211 patients with suspected otomycosis were examined. The presence of fungi was confirmed in about 51% of patients based on fungal elements in direct microscopy and culture-positive fungi. Aspergillus tubingensis was the most commonly isolated species (52.77%), followed by Aspergillus niger (25.92%). Otomycosis due to infection with Candida species was observed in 16% of cases. Of note, in 36.11% of cases, otomycosis was associated with TMP.
Conclusion
A mycological examination is indispensable for a correct diagnosis in patients with otitis extern. TMP should be considered in patients with otomycosis, as it appears to be relatively common in this population.
Similar content being viewed by others
References
García-Agudo L, Aznar-Marín P, Galán-Sánchez F, García-Martos P, Marín-Casanova P, Rodríguez-Iglesias M. Otomycosis due to filamentous fungi. Mycopathologia. 2011;172(4):307.
Aneja KR, Sharma C, Joshi R. Fungal infection of the ear: a common problem in the north eastern part of Haryana. Int J Pediatr Otorhinolaryngol. 2010;74(6):604–7. https://doi.org/10.1016/j.ijporl.2010.03.001.
Munguia R, Daniel SJ. Ototopical antifungals and otomycosis: a review. Int J Pediatr Otorhinolaryngol. 2008;72(4):453–9. https://doi.org/10.1016/j.ijporl.2007.12.005.
Pontes ZB, Silva AD, Lima Ede O, Guerra Mde H, Oliveira NM, Carvalho Mde F, et al. Otomycosis: a retrospective study. Braz J Otorhinolaryngol. 2009;75(3):367–70.
Kaur R, Mittal N, Kakkar M, Aggarwal AK, Mathur MD. Otomycosis: a clinicomycologic study. Ear Nose Throat J. 2000;79(8):606–9.
Gharaghani M, Seifi Z, Zarei MA. Otomycosis in iran: a review. Mycopathologia. 2015;179(5–6):415–24. https://doi.org/10.1007/s11046-015-9864-7.
Ray R, Pal S, Ghosh M, Samaddar D, Banerjee M. Prevalence of fungal infection in chronic otitis media—a study at a tertiary care hospital in Eastern India. Int J Curr Microbiol App Sci. 2015;4:684–90.
Ho T, Vrabec JT, Yoo D, Coker NJ. Otomycosis: clinical features and treatment implications. Otolaryngol Head Neck Surg. 2006;135(5):787–91.
Alshahni MM, Alshahni RZ, Fujisaki R, Tamura T, Shimizu Y, Yamanishi C, et al. A case of topical ofloxacin-induced otomycosis and literature review. Mycopathologia. 2021. https://doi.org/10.1007/s11046-021-00581-x.
Jia X, Liang Q, Chi F, Cao W. Otomycosis in Shanghai: aetiology, clinical features and therapy. Mycoses. 2012;55(5):404–9. https://doi.org/10.1111/j.1439-0507.2011.02132.x.
Nemati S, Hassanzadeh R, Jahromi SK, Abadi ADN. Otomycosis in the north of Iran: common pathogens and resistance to antifungal agents. Eur Arch Otorhinolaryngol. 2014;271(5):953–7.
Fasunla J, Ibekwe T, Onakoya P. Otomycosis in western Nigeria. Mycoses. 2008;51(1):67–70. https://doi.org/10.1111/j.1439-0507.2007.01441.x.
Samson RA, Noonim P, Meijer M, Houbraken J, Frisvad JC, Varga J. Diagnostic tools to identify black aspergilli. Stud Mycol. 2007;59:129–45. https://doi.org/10.3114/sim.2007.59.13.
Jafari Z, Motamedi M, Jalalizand N, Shokoohi GR, Charsizadeh A, Mirhendi H. Comparison of CHROMagar, polymerase chain reaction-restriction fragment length polymorphism, and polymerase chain reaction-fragment size for the identification of Candida species. Curr Med Mycol. 2017;3(3):10–5. https://doi.org/10.29252/cmm.3.3.10.
Shokoohi G, Javidnia J, Mirhendi H, Rasekh-Jahromi A, Rezaei-Matehkolaei A, Ansari S, et al. Molecular identification and antifungal susceptibility profiles of Candida dubliniensis and Candida africana isolated from vulvovaginal candidiasis: A single-centre experience in Iran. Mycoses. 2021;64(7):771–9.
Mirhendi H, Makimura K, Khoramizadeh M, Yamaguchi H. A one-enzyme PCR-RFLP assay for identification of six medically important Candida species. Nippon Ishinkin Gakkai Zasshi. 2006;47(3):225–9. https://doi.org/10.3314/jjmm.47.225.
Shokohi G, Mirhendi H, Kordbacheh P, Nikaeen M, Rezaei-Matehkolaei A, Abastabar M. Morphological and genotypic identification of some environmental isolates of Aspergillus in Iran based on beta-tubulin gene sequencing. J Isfahan Med School. 2012;29:166.
Yoon HJ, Choi HY, Kim YK, Song YJ, Ki M. Prevalence of fungal infections using National Health Insurance data from 2009–2013, South Korea. Epidemiol Health. 2014;36:e2014017.
Jain A, Jain S, Rawat S. Emerging fungal infections among children: a review on its clinical manifestations, diagnosis, and prevention. J Pharmacy Bioallied Sci. 2010;2(4):314.
Barati B, Okhovvat SA, Goljanian A, Omrani MR. Otomycosis in central iran: a clinical and mycological study. Iran Red Crescent Med J. 2011;13(12):873–6.
Saki N, Rafiei A, Nikakhlagh S, Amirrajab N, Saki S. Prevalence of otomycosis in Khouzestan Province, south-west Iran. J Laryngol Otol. 2013;127(1):25–7. https://doi.org/10.1017/S0022215112002277.
Bineshian F, Irajian G, Koochak-Alavi SK, Fredonian MR. A study on the frequency of fungal agents in otitis externa in Semnan. Iran J Pathol. 2006;1(4):141–4.
Farahnaz B, Gholamreza I, Seyed K, Mohammad R. A study on the frequency of fungal agents in otitis externa in Semnan (Iran). Iran J Pathol. 2006;1:141–4.
Sabz G, Gharaghani M, Mirhendi H, Ahmadi B, Gatee MA, Sisakht MT, et al. Clinical and microbial epidemiology of otomycosis in the city of Yasuj, southwest Iran, revealing Aspergillus tubingensis as the dominant causative agent. J Med Microbiol. 2019;68(4):585–90.
Cheraghsahar S, Kazemi S, Birjandi M, Yarahmadi M, Mahmoudi S, Mohammadi R, et al. Otomycosis in Western Iran: clinical and mycological aspects. Arch Clin Infect Dis. 2017;12(2):e57287.
Desai K, Malek S, Italia I, Jha S, Pandya V, Shah H. Fungal spectrum in otomycosis at tertiary care hospital. Natl J Integr Res Med. 2012;3(5):58–61.
Yegane Mogadam A, Asadi MA, Dehghani R, Hooshyar H. The prevalence of otomycosis in Kashan, Iran, during 2001–2003. Jundishapur J Microbiol. 2009;2(1):18–21.
Loh K, Tan K, Kumarasinghe G, Leong H, Yeoh K. Otitis externa—the clinical pattern in a tertiary institution in Singapore. Ann Acad Med Singap. 1998;27(2):215.
Prasad SC, Kotigadde S, Shekhar M, Thada ND, Prabhu P, T DS, et al. Primary otomycosis in the Indian subcontinent: predisposing factors, microbiology, and classification. Int J Microbiol. 2014;204:636493. https://doi.org/10.1155/2014/636493.
Abou-Halawa AS, Khan MA, Alrobaee AA, Alzolibani AA, Alshobaili HA. Otomycosis with perforated tympanic membrane: self medication with topical antifungal solution versus medicated ear wick. Int J Health Sci (Qassim). 2012;6(1):73–7. https://doi.org/10.12816/0005975.
Kurnatowski P, Filipiak A. Otomycosis: prevalence, clinical symptoms, therapeutic procedure. Mycoses. 2001;44(11–12):472–9. https://doi.org/10.1046/j.1439-0507.2001.00689.x.
Pradhan B, Tuladhar NR, Amatya RM. Prevalence of otomycosis in outpatient department of otolaryngology in Tribhuvan University Teaching Hospital, Kathmandu. Nepal Ann Otol Rhinol Laryngol. 2003;112(4):384–7. https://doi.org/10.1177/000348940311200416.
Ozcan KM, Ozcan M, Karaarslan A, Karaarslan F. Otomycosis in Turkey: predisposing factors, aetiology and therapy. J Laryngol Otol. 2003;117(1):39–42. https://doi.org/10.1258/002221503321046621.
Viswanatha B, Sumatha D, Vijayashree MS. Otomycosis in immunocompetent and immunocompromised patients: comparative study and literature review. Ear Nose Throat J. 2012;91(3):114–21. https://doi.org/10.1177/014556131209100308.
Anwar K, Gohar MS. Otomycosis; clinical features, predisposing factors and treatment implications. Pak J Med Sci. 2014;30(3):564–7. https://doi.org/10.12669/pjms.303.4106.
Aboutalebian S, Mahmoudi S, Mirhendi H, Okhovat A, Abtahi H, Chabavizadeh J. Molecular epidemiology of otomycosis in Isfahan revealed a large diversity in causative agents. J Med Microbiol. 2019;68(6):918–23. https://doi.org/10.1099/jmm.0.000985.
Kiakojuri K, Mahdavi Omran S, Roodgari S, Taghizadeh Armaki M, Hedayati MT, Shokohi T, et al. Molecular identification and antifungal susceptibility of yeasts and molds isolated from patients with otomycosis. Mycopathologia. 2021;186(2):245–57. https://doi.org/10.1007/s11046-021-00537-1.
Hurst WB. Outcome of 22 cases of perforated tympanic membrane caused by otomycosis. J Laryngol Otol. 2001;115(11):879–80. https://doi.org/10.1258/0022215011909486.
Kiakojori K, Bagherpour Jamnani N, Khafri S, Mahdavi OS. Assessment of response to treatment in patients with otomycosis. Iran J Otorhinolaryngol. 2018;30(96):41–7.
Sarwestani ZK, Hashemi S, Rezaie S, Shoar MG, Mahmoudi S, Elahi M, et al. Species identification and in vitro antifungal susceptibility testing of Aspergillus section Nigri strains isolated from otomycosis patients. J Mycol Med. 2018;28(2):279–84.
Kamali Sarwestani H, Daie Ghazvini R, Hashemi SJ, Rezaie S, Gerami Shoar M, Mahmoudi S, et al. Investigation of etiologic agents and clinical presentations of otomycosis at a tertiary referral center in Tehran. Iran Iran J Public Health. 2019;48(2):331–7.
Ali K, Hamed MA, Hassan H, Esmail A, Sheneef A. Identification of fungal pathogens in otomycosis and their drug sensitivity: our experience. Int Arch Otorhinolaryngol. 2018;22(04):400–3.
Abdelazeem M, Gamea A, Mubarak H, Elzawawy N. Epidemiology, causative agents, and risk factors affecting humanotomycosis infections. Turk J Med Sci. 2015;45(4):820–6.
Szigeti G, Kocsubé S, Dóczi I, Bereczki L, Vágvölgyi C, Varga J. Molecular identification and antifungal susceptibilities of black Aspergillus isolates from otomycosis cases in Hungary. Mycopathologia. 2012;174(2):143–7.
Howard SJ, Harrison E, Bowyer P, Varga J, Denning DW. Cryptic species and azole resistance in the Aspergillus niger complex. Antimicrob Agents Chemother. 2011;55(10):4802–9. https://doi.org/10.1128/AAC.00304-11.
Li Y, Wan Z, Liu W, Li R. Identification and susceptibility of Aspergillus section Nigri in china: prevalence of species and paradoxical growth in response to echinocandins. J Clin Microbiol. 2015;53(2):702–5. https://doi.org/10.1128/JCM.03233-14.
Shokoohi G, Rouhi Sefidmazgi R, Etehadnezhad M, Ahmadi B, Javidnia J, Nouripour Sisakht S et al. In vitro antifungal activity of luliconazole, efinaconazole, and nine comparators against Aspergillus and Candida strains isolated from otomycosis. Jundishapur J Microbiol. 2021;14(4):e115902.
Badali H, Fakhim H, Zarei F, Nabili M, Vaezi A, Poorzad N, et al. In vitro activities of five antifungal drugs against opportunistic agents of Aspergillus Nigri complex. Mycopathologia. 2016;181(3):235–40.
Zhang L, Wang X, Houbraken J, Mei H, Liao W, Hasimu H, et al. Molecular identification and in vitro antifungal susceptibility of Aspergillus isolates recovered from otomycosis patients in Western China. Mycopathologia. 2020;185(3):527–35.
Verweij PE, Chowdhary A, Melchers WJ, Meis JF. Azole resistance in Aspergillus fumigatus: can we retain the clinical use of mold-active antifungal azoles? Clin Infect Dis. 2016;62(3):362–8.
Iatta R, Nuccio F, Immediato D, Mosca A, De Carlo C, Miragliotta G, et al. Species distribution and in vitro azole susceptibility of Aspergillus section Nigri isolates from clinical and environmental settings. J Clin Microbiol. 2016;54(9):2365–72. https://doi.org/10.1128/JCM.01075-16.
Garcia-Martos P, Delgado D, Marin P, Mira J. Analysis of 40 cases of otomycosis. Enferm Infecc Microbiol Clin. 1993;11(9):487–9.
Acknowledgements
We would like to thank Dr. Reza Rouhi Sefidmazgi from Department of Medical Otorhinolaryngology, Jahrom University of Medical Sciences, Jahrom, Iran for collaborating on this project.
Funding
This work was supported by Jahrom University of Medical Sciences Deputy of Research, Jahrom, Iran (Grant No. 99000344).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest to disclose related to this study.
Ethical Approval
This research was approved by the Ethics Committee of the Jahrom University of Medical Sciences, Jahrom, Iran (Approval Code: IR.JUMS.REC.1397.062).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Handling Editor: Macit Ilkit.
Rights and permissions
About this article
Cite this article
Javidnia, J., Ghotbi, Z., Ghojoghi, A. et al. Otomycosis in the South of Iran with a High Prevalence of Tympanic Membrane Perforation: A Hospital-Based Study. Mycopathologia 187, 225–233 (2022). https://doi.org/10.1007/s11046-022-00626-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-022-00626-9