Abstract
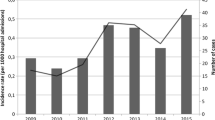
The aims of this study were to evaluate the epidemiology of nosocomial candidemia in a tertiary hospital in South Brazil and the in vitro antifungal susceptibility of isolates. Blood strains from 108 patients were identified by PCR-based method. Some 30.5 % of candidemia were caused by Candida tropicalis, 28.7 % were due to Candida albicans, 24.1 % with Candida parapsilosis sensu stricto, 8.3 % with Candida glabrata sensu lato, 1.8 % involved Candida krusei and 6.6 % with other species. Candidemia was more common in intensive care unit settings (66 %). In vitro susceptibility to antifungal drugs was determined by a microdilution method; and new species-specific clinical breakpoints for fluconazole and voriconazole were applied. Overall susceptibility rates were 100 % for itraconazole, 91 % for fluconazole, 98 % for voriconazole and 99 % for amphotericin B. Fluconazole resistance was mostly among C. parapsilosis sensu stricto isolates (26.9 %). Most of the findings reported here agreed with epidemiological features common to other tertiary hospitals in Brazil; but also revealed some peculiarities, such as a high frequency of C. tropicalis associated with candidemia. Besides, high rate of fluconazole resistance among C. parapsilosis stricto sensu isolates was obtained when applying the new species-specific clinical breakpoints.
Similar content being viewed by others
References
Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. J Clin Microbiol Rev. 2007;20:133–63.
Fortún J, Martín-Dávila P, Gómez-Garcia de la Pedrosa E, Pintado V, Cobo J, Fresco G, Meije Y, Ros L, Alvarez ME, Luengo J, Agundez M, Belso A, Sánchez-Sousa A, Loza E, Moreno S. Emerging trends in candidemia: a higher incidence but a similar outcome. J Infect. 2012;65:64–70.
Cuenca-Estrella M, Gomez-lopez A, Cuesta I, Zaragoza O, Mellado E, Rodriguez-Tudela JL. Frequency of voriconazole resistance in vitro among Spanish clinical isolates of Candida spp. according to breakpoints established by the Antifungal Subcommittee of the European Committee on Antimicrobial Susceptibility Testing. Antimicrob Agents Chemother. 2011;55:1794–7.
Schmalreck AF, Willinger B, Haase G, Blum G, Lass-Flörl C, Fegeler W, Becker K. Antifungal susceptibility testing-AFST study group. Species and susceptibility distribution of 1062 clinical yeast isolates to azoles, echinocandins, flucytosine and amphotericin B from a multi-centre study. Mycoses. 2012;2012(55):e124–37.
Marra AR, Camargo LF, Pignatari AC, Sukiennik T, Behar PR, Medeiros EA, Ribeiro J, Girão E, Correa L, Guerra C, Brites C, Pereira CA, Carneiro I, Reis M, De Souza MA, Tranchesi R, Barata CU, Edmond MB, Brazilian SCOPE Study Group. Nosocomial bloodstream infections in Brazilian Hospitals: analysis of 2,563 cases from a prospective nationwide surveillance study. J Clin Microbiol. 2011;49:1866–71.
Nucci M, Queiroz-Telles F, Tobon AM, Restrepo A, Colombo AL. Epidemiology of opportunistic fungal infections in Latin America. Clin Infect Dis. 2010;51:561–70.
Goldani LZ, Mario PSS. Candida tropicalis fungemia in a tertiary care hospital. J Infect. 2003;46:155–60.
Aquino VR, Lunardi LW, Goldani LZ, Barth AL. Prevalence, susceptibility profile for fluconazole and risk factors for candidemia in a tertiary care hospital in Southern Brazil. Braz J Infect Dis. 2005;9:411–8.
França JCB, Ribeiro CEL, Queiroz-Telles F. Candidemia em um hospital terciário brasileiro: incidência, frequência das diferentes espécies, fatores de risco e suscetibilidade aos antifúngicos. Rev Soc Bras Med Trop. 2008;41:23–8.
Li YL, Leaw SN, Chen JH, Chang HC, Chang TC. Rapid identification of yeasts commonly found in positive blood cultures by amplification of the internal transcribed spacer regions 1 and 2. Eur J Clin Microbiol Infect Dis. 2003;22:693–6.
Williams JGK, Kubelik AR, Livak KJ, Rafalski JA, Tingey AV. DNA polymorphisms amplified by arbitrary primers are useful as genetic markers. Nucleic Acids Res. 1990;18:6531–5.
Tavanti A, Davidson AD, Gow NAR, Maiden MCJ, Odds FC. Candida orthopsilosis and Candida metapsilosis spp. nov. to replace Candida parapsilosis Groups II and III. J Clin Microbiol. 2005;43:284–92.
Furlaneto MC, Rota JF, Quesada RMB, Furlaneto-Maia L, Rodrigues R, Oda S, Oliveira MT, Serpa R, França EJG. Species distribution and in vitro fluconazole susceptibility of clinical Candida isolates in a Brazilian tertiary-care hospital over a 3-year period. Rev Soc Bras Med Trop. 2011;44:595–9.
Subcommittee on Antifungal Susceptibility Testing. (AFST) of the Escmid European Committee for Antimicrobial for Antimicrobial Susceptibility Testing (EUCAST). EUCAST definitive document EDef 7.1: method for the determination of broth dilution MICs of antifungal agents for fermentative yeasts. Clin Microbiol Infect. 2008;14:398–405.
Pfaller MA, Andes D, Diekema DJ, Espinel-Ingroff A, Sheehan D. Wild-type MIC distributions, epidemiological cutoff values and species-specific clinical breakpoints for fluconazole and Candida: time for harmonization of CLSI and EUCAST broth microdilution methods. Drug Res Updates. 2010;13:180–95.
Pfaller MA, Espinel-Ingroff A, Canton E, Castanheira M, Cuenca-Estrella M, Diekema DJ, Fothergill A, Fuller J, Ghannoum M, Jones RN, Lockhart SR, Martin-Mazuelos E, Melhem MS, Ostrosky-Zeichner L, Pappas P, Pelaez T, Peman J, Rex J, Szeszs MW. Wild-type MIC distributions and epidemiological cutoff values for amphotericin B, flucytosine, and itraconazole and Candida spp. as determined by CLSI broth microdilution. J Clin Microbiol. 2012;6:2040–6.
Bruder-Nascimento A, Camargo CH, Sugizaki MF, Sadatsune T, Montelli AC, Mondelli AL, Bagagli E. Species distribution and susceptibility profile of Candida species in a Brazilian public tertiary hospital. Res Notes. 2010;3:1–5.
Passos XS, Costa CR, Araújo CR, Nascimento ES, Souza LKH, Fernandes OFL, Sales WS, Silva MRRS. Species distribution and antifungal susceptibility patterns of Candida spp. bloodstream isolates from a Brazilian tertiary care hospital. Mycopathologia. 2007;163:145–51.
Pereira GH, Müller PR, Szeszs MW, Levin AS, Melhem MSC. Five-year evaluation of bloodstream yeast infection in a tertiary hospital: the predominance of non-C. albicans Candida species. Med Mycol. 2010;48:839–42.
Bonfietti LX, Szeszs MW, Chang MR, Martins MA, Pukinskas SRBS, Nunes MO, Pereira GH, Paniago AMM, Purisco SU, Melhem MSC. Ten-year study of species distribution and antifungal susceptibilities of Candida bloodstream isolates at a Brazilian tertiary hospital. Mycopathologia. 2012;174:389–96.
Moretti ML, Trabasso P, Lyra L, Fagnani R, Resende MR, Cardoso LGO, Schreiber AZ. Is the incidence of candidemia caused by Candida glabrata increasing in Brazil? Five year surveillance of Candida bloodstream infection in a university reference hospital in southeast Brazil. Med Mycol. 2013;51:225–30.
Chang MR, Correia FP, Costa LC, Xavier PC, Palhares DB, Taira DL, Paniago AMM, Pontes ERJ, Machado VE. Candida bloodstream infection: data from a teaching hospital in Mato Grosso do Sul, Brasil. Rev Inst Med Trop. 2008;50:265–8.
Wille MP, Guimarães T, Furtado GHC, Colombo AL. Historical trends in the epidemiology of candidaemia: analysis of an 11-year period in a tertiary care hospital in Brazil. Mem Inst Oswaldo Cruz. 2013;108:288–92.
Chai LYA, Denning DW, Warn P. Candida tropicalis in human disease. Crit Rev Microbiol. 2010;36:282–98.
Lockhart SR, Messer SA, Pfaller MA, Diekema DJ. Geographic distribution and antifungal susceptibility of the newly described species Candida orthopsilosis and Candida metapsilosis in comparison to the closely related species Candida parapsilosis. J Clin Microbiol. 2008;46:2659–64.
Miranda-Zapico I, Eraso E, Hernandez-Almaraz JL, López-Soria LM, Carrillo-Munoz AJ, Hernández-Molina JM, Quindós G. Prevalence and antifungal susceptibility patterns of new crypto-species inside the species complexes Candida parapsilosis and Candida glabrata among blood isolates from a Spanish tertiary hospital. J Antimicrob Chemother. 2011;66:2315–22.
Colombo AL, Guimarães T, Silva LRBF, Monfardini LPA, Cunha AKB, Rady P, Alves T, Rosas RC. Prospective observational study of candidemia in São Paulo, Brazil: incidence rate, epidemiology, and predictors of mortality. Infect Control Hosp Epidemiol. 2007;28:570–6.
Colombo AL, Garnica M, Aranha Camargo LF, Da Cunha CA, Bandeira AC, Borghi D, Campos T, Senna AL, Didier MEV, Dias VC, Nucci M. Candida glabrata: an emerging pathogen in Brazilian tertiary care hospitals. Med Mycol. 2013;51:38–44.
Pasqualotto AC, Zimerman RA, Alves SH, Aquino VR, Branco D, Wiltgen D, do Amaral A, Cechinel R, Colares SM, da Rocha IG, Severo LC, Sukiennik TCT. Take control over your fluconazole prescriptions: the growing importance of Candida glabrata as an agent of candidemia in Brazil. Infect Control Hosp Epidemiol. 2008;29:898–9.
Clark TA, Slavinski SA, Morgan J, Lott T, Arthington-Skaggs BA, Brandt ME, Webb RM, Currier M, Flowers RH, Fridkin SK, Hajjeh RA. Epidemiologic and molecular characterization of an outbreak of Candida parapsilosis bloodstream infections in a community hospital. J Clin Microbiol. 2004;42:4468–72.
Garey KW, Rege M, Pai MP, Mingo DE, Suda KJ, Turpin RS, Bearden DT. Time to initiation of fluconazole therapy impacts mortality in patients with candidemia: a multiinstitutional study. Clin Infect Dis. 2006;43:25–31.
Pemán J, Cantón E, Quindós G, Eraso E, Alcoba J, Guinea J, Merino P, Ruiz-Pérez-De-Pipaon MT, Pérez-Del-Molino L, Linares-Sicilia MJ, Marco F, García J, Roselló EM, Gómez-G-De-La-Pedrosa E, Borrell N, Porras A, Yagüe G. Epidemiology, species distribution and in vitro antifungal susceptibility of fungaemia in a Spanish multicentre prospective survey. J Antimicrob Chemother. 2012;67:1181–7.
Matta DA, Almeida LP, Machado AM, Azevedo AC, Kusano EJU, Travassos NF, Salomão R, Colombo AL. Antifungal susceptibility of 1000 Candida bloodstream isolates to 5 antifungal drugs: results of a multicenter study conducted in São Paulo, Brazil, 1995–2003. Diagn Microbiol Infect Dis. 2007;57:300–4.
Purisco SU, Martins MA, Szeszs MW, Castro e Silva DM, Pukinskas SRBS, Bonfietti LX, Baez AA, Melhem MSC. Comparison of the microdilution (BMD) method of the European Committee on Antimicrobial Susceptibility Testing and the Clinical Laboratory Standards Institute BMD method for non-Candida albicans and non-C. tropicalis bloodstream isolates from eleven tertiary hospitals in São Paulo state, Brazil. FEMS Yeast Res. 2012;12:890–6.
Colombo AL, Guimarães T, Camargo LFA, Richtmann R, Queiroz-Telles F, Salles MJC, Cunha CA, Yasuda MAS, Moretti MA, Nucci M. Brazilian guidelines for the management of candidiasis—a joint meeting report of three medical societies: Sociedade Brasileira de Infectologia, Sociedade Paulista de Infectologia and Sociedade Brasileira de Medicina Tropical. Braz J Infect Dis. 2013;17:283–312.
Acknowledgments
This work was supported by Fundação Araucária/Governo do Paraná–Brazil and PROPPG/UEL-Brazil. V.G.C. was fellowship-holder of Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES)—Brazil.
Conflict of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
da Costa, V.G., Quesada, R.M.B., Abe, A.T.S. et al. Nosocomial Bloodstream Candida Infections in a Tertiary-Care Hospital in South Brazil: A 4-Year Survey. Mycopathologia 178, 243–250 (2014). https://doi.org/10.1007/s11046-014-9791-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-014-9791-z