Abstract
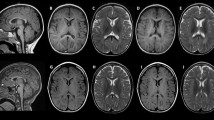
The mitochondrial encephalomyopathies represent a clinically heterogeneous group of neurodegenerative disorders. The clinical phenotype of patients could be explained by mutations of mitochondria-related genes, notably SUCLG1 and SUCLA2. Here, we presented a 5-year-old boy with clinical features of mitochondrial encephalomyopathy from Iran. Also, a systematic review was performed to explore the involvement of SUCLG1 mutations in published mitochondrial encephalomyopathies cases. Genotyping was performed by implementing whole-exome sequencing. Moreover, quantification of the mtDNA content was performed by real-time qPCR. We identified a novel, homozygote missense variant chr2: 84676796 A > T (hg19) in the SUCLG1 gene. This mutation substitutes Cys with Ser at the 60-position of the SUCLG1 protein. Furthermore, the in-silico analysis revealed that the mutated position in the genome is well conserved in mammalians, that implies mutation in this residue would possibly result in phenotypic consequences. Here, we identified a novel, homozygote missense variant chr2: 84676796 A > T in the SUCLG1 gene. Using a range of experimental and in silico analysis, we found that the mutation might explain the observed phenotype in the family.






Similar content being viewed by others
Data availability
The authors acknowledge that the article incorporates the data supporting the findings of the study.
References
Piña-Garza JE, James KC (2019) 5 - Psychomotor retardation and regression. In: Piña-Garza JE, James KC (eds) Fenichel’s clinical pediatric neurology, 8th edn. Elsevier, Philadelphia, pp 115–149
Hirano M (2007) 86-Metabolic myopathies. In: Gilman S (ed) Neurobiology of Disease. Academic Press, Burlington, pp 947–956
Oldfors A, Tulinius M (2003) Mitochondrial encephalomyopathies. J Neuropathol Exp Neurol 62(3):217–227
Rouzier C, Le Guedard-Mereuze S, Fragaki K, Serre V, Miro J, Tuffery-Giraud S et al (2010) The severity of phenotype linked to SUCLG1 mutations could be correlated with residual amount of SUCLG1 protein. J Med Genet 47(10):670–676
Landsverk ML, Zhang VW, Wong LC, Andersson HC (2014) A SUCLG1 mutation in a patient with mitochondrial DNA depletion and congenital anomalies. Mol Genet Metab Rep 1:451–454
Johnson JD, Mehus JG, Tews K, Milavetz BI, Lambeth DO (1998) Genetic evidence for the expression of ATP- and GTP-specific succinyl-CoA synthetases in multicellular eucaryotes. J Biol Chem 273(42):27580–27586
Valayannopoulos V, Haudry C, Serre V, Barth M, Boddaert N, Arnoux JB et al (2010) New SUCLG1 patients expanding the phenotypic spectrum of this rare cause of mild methylmalonic aciduria. Mitochondrion 10(4):335–341
Ostergaard E (2008) Disorders caused by deficiency of succinate-CoA ligase. J Inherit Metab Dis 31(2):226–229
Wang K, Li M, Hakonarson H (2010) ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res 38(16):e164
Wheeler DL, Barrett T, Benson DA, Bryant SH, Canese K, Chetvernin V et al (2007) Database resources of the national center for biotechnology information. Nucleic Acids Res 35:D5–D12
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T et al (2016) Analysis of protein-coding genetic variation in 60,706 humans. Nature 536(7616):285–291
Landrum MJ, Lee JM, Riley GR, Jang W, Rubinstein WS, Church DM et al (2014) ClinVar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res 42:D980–D985
Berman H, Westbrook J, Feng Z, Gilliland G, Bhat T, Weissig H, et al. The protein data bank nucleic acids research, 28, 235–242. URL: www rcsb org Citation. 2000.
Protein Data Bank (2019) the single global archive for 3D macromolecular structure data. Nucleic Acids Res 47(D1):D520–D528
Venselaar H, Te Beek TA, Kuipers RK, Hekkelman ML, Vriend G (2010) Protein structure analysis of mutations causing inheritable diseases: an e-Science approach with life scientist friendly interfaces. BMC Bioinforms 11:548
Rodrigues CH, Pires DE, Ascher DB (2018) DynaMut: predicting the impact of mutations on protein conformation, flexibility and stability. Nucleic Acids Res 46(W1):W350–W355
DeLano WL (2002) Pymol: an open-source molecular graphics tool. CCP Newslett Protein Crystall 40(1):82–92
Sadat R, Barca E, Masand R, Donti TR, Naini A, De Vivo DC et al (2016) Functional cellular analyses reveal energy metabolism defect and mitochondrial DNA depletion in a case of mitochondrial aconitase deficiency. Mol Genet Metab 118(1):28–34
Donti TR, Masand R, Scott DA, Craigen WJ, Graham BH (2016) Expanding the phenotypic spectrum of Succinyl-CoA ligase deficiency through functional validation of a new SUCLG1 variant. Mol Genet Metab 119(1–2):68–74
Fattahi Z, Beheshtian M, Mohseni M, Poustchi H, Sellars E, Nezhadi SH et al (2019) Iranome: A catalog of genomic variations in the Iranian population. Hum Mutat 40(11):1968–1984
Shihab HA, Gough J, Cooper DN, Stenson PD, Barker GL, Edwards KJ et al (2013) Predicting the functional, molecular, and phenotypic consequences of amino acid substitutions using hidden Markov models. Hum Mutat 34(1):57–65
Raimondi D, Tanyalcin I, Ferte J, Gazzo A, Orlando G, Lenaerts T et al (2017) DEOGEN2: prediction and interactive visualization of single amino acid variant deleteriousness in human proteins. Nucleic Acids Res 45(W1):W201–W206
Ng PC, Henikoff S (2003) SIFT: Predicting amino acid changes that affect protein function. Nucleic Acids Res 31(13):3812–3814
Vaser R, Adusumalli S, Leng SN, Sikic M, Ng PC (2016) SIFT missense predictions for genomes. Nat Protoc 11(1):1
Choi Y, Chan AP (2015) PROVEAN web server: a tool to predict the functional effect of amino acid substitutions and indels. Bioinformatics (Oxford, England) 31(16):2745–2747
Sundaram L, Gao H, Padigepati SR, McRae JF, Li Y, Kosmicki JA et al (2018) Predicting the clinical impact of human mutation with deep neural networks. Nat Genet 50(8):1161–1170
Kim S, Jhong JH, Lee J, Koo JY (2017) Meta-analytic support vector machine for integrating multiple omics data. BioData Mining 10:2
Dong C, Wei P, Jian X, Gibbs R, Boerwinkle E, Wang K et al (2015) Comparison and integration of deleteriousness prediction methods for nonsynonymous SNVs in whole exome sequencing studies. Hum Mol Genet 24(8):2125–2137
Chun S, Fay JC (2009) Identification of deleterious mutations within three human genomes. Genome Res 19(9):1553–1561
Guennebaud G, Jacob B, Avery P, Bachrach A, Barthelemy S (2010) Eigen v3
Qi H, Chen C, Zhang H, Long JJ, Chung WK, Guan Y, et al. (2018) MVP: predicting pathogenicity of missense variants by deep learning. bioRxiv. 259390
Ioannidis NM, Rothstein JH, Pejaver V, Middha S, McDonnell SK, Baheti S et al (2016) REVEL: an ensemble method for predicting the pathogenicity of rare missense variants. Am J Hum Genet 99(4):877–885
Dai LF, Fang F, Liu ZM, Shen DM, Ding CH, Li JW et al (2019) Phenotype and genotype of twelve Chinese children with mitochondrial DNA depletion syndromes. Zhonghua er ke za zhi: Chin J Pediatr 57(3):211–216
Maalej M, Tej A, Bouguila J, Tilouche S, Majdoub S, Khabou B et al (2018) Clinical, molecular, and computational analysis in two cases with mitochondrial encephalomyopathy associated with SUCLG1 mutation in a consanguineous family. Biochem Biophys Res Commun 495(2):1730–1737
Fang F, Liu Z, Fang H, Wu J, Shen D, Sun S et al (2017) The clinical and genetic characteristics in children with mitochondrial disease in China. Sci China Life Sci 60(7):746–757
Carrozzo R, Verrigni D, Rasmussen M, de Coo R, Amartino H, Bianchi M et al (2016) Succinate-CoA ligase deficiency due to mutations in SUCLA2 and SUCLG1: phenotype and genotype correlations in 71 patients. J Inherit Metab Dis 39(2):243–252
Liu Y, Li X, Wang Q, Ding Y, Song J, Yang Y (2016) Five novel SUCLG1 mutations in three Chinese patients with succinate-CoA ligase deficiency noticed by mild methylmalonic aciduria. Brain Dev 38(1):61–67
Ostergaard E, Schwartz M, Batbayli M, Christensen E, Hjalmarson O, Kollberg G et al (2010) A novel missense mutation in SUCLG1 associated with mitochondrial DNA depletion, encephalomyopathic form, with methylmalonic aciduria. Eur J Pediatr 169(2):201–205
Navarro-Sastre A, Tort F, Garcia-Villoria J, Pons MR, Nascimento A, Colomer J et al (2012) Mitochondrial DNA depletion syndrome: new descriptions and the use of citrate synthase as a helpful tool to better characterise the patients. Mol Genet Metab 107(3):409–415
Van Hove JL, Saenz MS, Thomas JA, Gallagher RC, Lovell MA, Fenton LZ et al (2010) Succinyl-CoA ligase deficiency: a mitochondrial hepatoencephalomyopathy. Pediatr Res 68(2):159–164
Rivera H, Merinero B, Martinez-Pardo M, Arroyo I, Ruiz-Sala P, Bornstein B et al (2010) Marked mitochondrial DNA depletion associated with a novel SUCLG1 gene mutation resulting in lethal neonatal acidosis, multi-organ failure, and interrupted aortic arch. Mitochondrion 10(4):362–368
Sakamoto O, Ohura T, Murayama K, Ohtake A, Harashima H, Abukawa D et al (2011) Neonatal lactic acidosis with methylmalonic aciduria due to novel mutations in the SUCLG1 gene. Pediatr Int 53(6):921–925
Randolph LM, Jackson HA, Wang J, Shimada H, Sanchez-Lara PA, Wong DA et al (2011) Fatal infantile lactic acidosis and a novel homozygous mutation in the SUCLG1 gene: a mitochondrial DNA depletion disorder. Mol Genet Metab 102(2):149–152
Ostergaard E, Christensen E, Kristensen E, Mogensen B, Duno M, Shoubridge EA et al (2007) Deficiency of the α subunit of succinate–coenzyme a ligase causes fatal infantile lactic acidosis with mitochondrial DNA depletion. Am J Hum Genet 81(2):383–387
Miller C, Wang L, Ostergaard E, Dan P, Saada A (2011) The interplay between SUCLA2, SUCLG2, and mitochondrial DNA depletion. Biochem Biophys Acta 1812(5):625–629
Acknowledgment
The authors thank Shahid Beheshti University of Medical Sciences, for financial support.
Author information
Authors and Affiliations
Contributions
SMR and TAS conducted and analyzed the experiments. MEO was involved in conducting the experiments and drafting the manuscript. MT contributed to the experiment analysis and structural analysis. BA participated in analyzing the experiments and drafting the manuscript. HGH designed the study, analyzed the next-generation sequencing (NGS) data, and participated in structural analysis as well as the writing of the manuscript. All authors reviewed the manuscript and confirmed the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors acknowledged that there is no conflict of interest.
Ethical approval
All procedures conducted in this study involving human participants were following the ethical standards of the Ethical Committee of Shahid Beheshti University of Medical Sciences.
Informed consent
Informed consent was obtained from the patient's parents or legal representative.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Molaei Ramsheh, S., Erfanian Omidvar, M., Tabasinezhad, M. et al. SUCLG1 mutations and mitochondrial encephalomyopathy: a case study and review of the literature. Mol Biol Rep 47, 9699–9714 (2020). https://doi.org/10.1007/s11033-020-05999-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05999-y