Abstract
Bisphenol A (BPA) is an estrogenic environmental toxin widely used for the production of plastics. Frequent human exposure to this chemical has been proposed to be a potential public health risk. The objective of this study was to assess the effects of BPA on germ cell cyst breakdown and primordial follicle formation. Pregnant mice were treated with BPA at doses of 0, 0.02, 0.04, 0.08 mg/kg body weight/day from 12.5 day postcoitum. BPA was delivered orally to pregnant female mice. A dose–response relationship was observed with increased BPA exposure level associated with more oocytes in germ cell cyst and less primordial follicle at postnatal day 3 (P < 0.01). Progression to meiosis prophase I of oocytes was delayed in the 0.08 mg/kg bw/day treated group (P < 0.01). Decreased mRNA expression of specific meiotic genes including Stra8, Dmc1, Rec8 and Scp3 were observed. In conclusion, BPA exposure can affect the formation of primordial follicle by inhibiting meiotic progression of oocytes.




Similar content being viewed by others
References
Pepling ME, Spradling AC (1998) Female mouse germ cells form synchronously dividing cysts. Development 125:3323–3328
Borum K (1961) Oogenesis in the mouse. A study of the meiotic prophase. Exp Cell Res 24:495–507
Pepling ME, Spradling AC (2001) Mouse ovarian germ cell cysts undergo programmed breakdown to form primordial follicles. Dev Biol 234:339–351
Roy D, Palangat M, Chen CW, Thomas RD, Colerangle J, Atkinson A, Yan ZJ (1997) Biochemical and molecular changes at the cellular level in response to exposure to environmental estrogen-like chemicals. J Toxicol Environ Health 50:1–29
Gilbert J, Startin JR, Wallwork MA (1978) Gas chromatographic determination of 1,1,1-trichloroethane in vinyl chloride polymers and in foods. J Chromatogr 160:127–132
Fung EY, Ewoldsen NO, St. Germain HA, Marx DB, Miaw CL, Siew C, Chou HN, Gruninger SE, Meyer DM (2000) Pharmacokinetics of bisphenol A released from a dental sealant. J Am Dent Assoc 131:51–58
Brotons JA, Olea-Serrano MF, Villalobos M, Pedraza V, Olea N (1995) Xenoestrogens released from lacquer coatings in food cans. Environ Health Perspect 103:608–612
Krishnan AV, Stathis P, Permuth SF, Tokes L, Feldman D (1993) Bisphenol-A: an estrogenic substance is released from polycarbonate flasks during autoclaving. Endocrinology 132:2279–2286
NTP-CERHR (2008) Monograph on the potential human reproductive and developmental effects of bisphenol A, NTP CERHR MON i-III1
Kim HS, Han SY, Yoo SD, Lee BM, Park KL (2001) Potential estrogenic effects of bisphenol-A estimated by in vitro and in vivo combination assays. J Toxicol Sci 26:111–118
Laws SC, Carey SA, Ferrell JM, Bodman GJ, Cooper RL (2000) Estrogenic activity of octylphenol, nonylphenol, bisphenol A and methoxychlor in rats. Toxicol Sci 54:154–167
Nakamura K, Itoh K, Sugimoto T, Fushiki S (2007) Prenatal exposure to bisphenol A affects adult murine neocortical structure. Neurosci Lett 420:100–105
Nakamura K, Itoh K, Yaoi T, Fujiwara Y, Sugimoto T, Fushiki S (2006) Murine neocortical histogenesis is perturbed by prenatal exposure to low doses of bisphenol A. J Neurosci Res 84:1197–1205
Hunt PA, Koehler KE, Susiarjo M, Hodges CA, Ilagan A, Voigt RC, Thomas S, Thomas BF, Hassold TJ (2003) Bisphenol a exposure causes meiotic aneuploidy in the female mouse. Curr Biol 13:546–553
Can A, Semiz O, Cinar O (2005) Bisphenol-A induces cell cycle delay and alters centrosome and spindle microtubular organization in oocytes during meiosis. Mol Hum Reprod 11:389–396
Pacchierotti F, Ranaldi R, Eichenlaub-Ritter U, Attia S, Adler ID (2008) Evaluation of aneugenic effects of bisphenol A in somatic and germ cells of the mouse. Mutat Res 651:64–70
Eichenlaub-Ritter U, Vogt E, Cukurcam S, Sun F, Pacchierotti F, Parry J (2008) Exposure of mouse oocytes to bisphenol A causes meiotic arrest but not aneuploidy. Mutat Res 651:82–92
Susiarjo M, Hassold TJ, Freeman E, Hunt PA (2007) Bisphenol A exposure in utero disrupts early oogenesis in the mouse. PLoS Genet 3:e5
Menke DB, Koubova J, Page DC (2003) Sexual differentiation of germ cells in XX mouse gonads occurs in an anterior-to-posterior wave. Dev Biol 262:303–312
Baltus AE, Menke DB, Hu YC, Goodheart ML, Carpenter AE, de Rooij DG, Page DC (2006) In germ cells of mouse embryonic ovaries, the decision to enter meiosis precedes premeiotic DNA replication. Nat Genet 38:1430–1434
Murphy K, Carvajal L, Medico L, Pepling M (2005) Expression of Stat3 in germ cells of developing and adult mouse ovaries and testes. Gene Expr Patterns 5:475–482
Zuccotti M, Monk M (1995) Methylation of the mouse Xist gene in sperm and eggs correlates with imprinted Xist expression and paternal X-inactivation. Nat Genet 9:316–320
SAS Institute (1996) SAS user’s guide: statistics, version 7.0 edn. SAS Institute, Cary
Paredes A, Garcia-Rudaz C, Kerr B, Tapia V, Dissen GA, Costa ME, Cornea A, Ojeda SR (2005) Loss of synaptonemal complex protein-1, a synaptonemal complex protein, contributes to the initiation of follicular assembly in the developing rat ovary. Endocrinology 146:5267–5277
Bird A (2002) DNA methylation patterns and epigenetic memory. Genes Dev 16:6–21
Li E (2002) Chromatin modification and epigenetic reprogramming in mammalian development. Nat Rev Genet 3:662–673
Reik W (2007) Stability and flexibility of epigenetic gene regulation in mammalian development. Nature 447:425–432
Schaefer CB, Ooi SK, Bestor TH, Bourc’his D (2007) Epigenetic decisions in mammalian germ cells. Science 316:398–399
Jefferson W, Newbold R, Padilla-Banks E, Pepling M (2006) Neonatal genistein treatment alters ovarian differentiation in the mouse: inhibition of oocyte nest breakdown and increased oocyte survival. Biol Reprod 74:161–168
Gould JC, Leonard LS, Maness SC, Wagner BL, Conner K, Zacharewski T, Safe S, McDonnell DP, Gaido KW (1998) Bisphenol A interacts with the estrogen receptor alpha in a distinct manner from estradiol. Mol Cell Endocrinol 142:203–214
Routledge EJ, White R, Parker MG, Sumpter JP (2000) Differential effects of xenoestrogens on coactivator recruitment by estrogen receptor (ER) alpha and ERbeta. J Biol Chem 275:35986–35993
Kuiper GG, Carlsson B, Grandien K, Enmark E, Haggblad J, Nilsson S, Gustafsson JA (1997) Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors alpha and beta. Endocrinology 138:863–870
Enmark E, Gustafsson JA (1999) Oestrogen receptors—an overview. J Intern Med 246:133–138
Nielsen M, Bjornsdottir S, Hoyer PE, Byskov AG (2000) Ontogeny of oestrogen receptor alpha in gonads and sex ducts of fetal and newborn mice. J Reprod Fertil 118:195–204
Jefferson WN, Couse JF, Banks EP, Korach KS, Newbold RR (2000) Expression of estrogen receptor beta is developmentally regulated in reproductive tissues of male and female mice. Biol Reprod 62:310–317
Vaskivuo TE, Maentausta M, Torn S, Oduwole O, Lonnberg A, Herva R, Isomaa V, Tapanainen JS (2005) Estrogen receptors and estrogen-metabolizing enzymes in human ovaries during fetal development. J Clin Endocrinol Metab 90:3752–3756
Beker-van Woudenberg AR, van Tol HT, Roele BA, Colenbrander B, Bevers MM (2004) Estradiol and its membrane-impermeable conjugate (estradiol-bovine serum albumin) during in vitro maturation of bovine oocytes: effects on nuclear and cytoplasmic maturation, cytoskeleton, and embryo quality. Biol Reprod 70:1465–1474
Yang P, Wang J, Shen Y, Roy SK (2004) Developmental expression of estrogen receptor (ER) alpha and ERbeta in the hamster ovary: regulation by follicle-stimulating hormone. Endocrinology 145:5757–5766
Zhou Q, Nie R, Prins GS, Saunders PT, Katzenellenboge BS, Hess RA (2002) Localization of androgen and estrogen receptors in adult male mouse reproductive tract. J Androl 23:870–881
van Pelt AM, de Rooij DG, van der Burg B, van der Saag PT, Gustafsson JA, Kuiper GG (1999) Ontogeny of estrogen receptor-beta expression in rat testis. Endocrinology 140:478–483
Acknowledgments
This work was supported by National Basic Research Program of China (973 Program, 2007CB947401, 2011CB944501 and 2012CB944401), National Nature Science Foundation (31001010), Foundation of Distinguished Young Scholars (JQ201109), Foundation of Education Department (J11LC20) and Taishan Scholar Foundation of Shandong Province.
Author information
Authors and Affiliations
Corresponding author
Additional information
H.-Q. Zhang and X.-F. Zhang both are co-first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11033_2011_1372_MOESM1_ESM.pdf
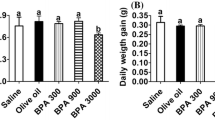
Fig. S1. A, B shows the percentage of oocytes in cyst and different types of follicles in control and different BPA-treated groups at PND 5, PND 7, respectively. Supplementary material 1 (PDF 38 kb)
11033_2011_1372_MOESM2_ESM.pdf
Fig. S2. Infant mouse health check. (A) litter size in control and different BPA groups, (B) sex ratio of infant mouse in control and different BPA groups. Supplementary material 2 (PDF 14 kb)
11033_2011_1372_MOESM3_ESM.pdf
Fig. S3. The mRNA expression of Estrogen Receptors (ERα and ERβ) in control and 0.08 mg/kg bw/day treated group at 17.5 dpc. The results were presented as mean ± SD. * indicates significance of P < 0.05; ** indicates significance of P < 0.01. Supplementary material 3 (PDF 13 kb)
Rights and permissions
About this article
Cite this article
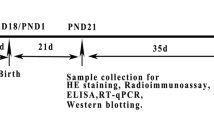
Zhang, HQ., Zhang, XF., Zhang, LJ. et al. Fetal exposure to bisphenol A affects the primordial follicle formation by inhibiting the meiotic progression of oocytes. Mol Biol Rep 39, 5651–5657 (2012). https://doi.org/10.1007/s11033-011-1372-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-011-1372-3