Abstract
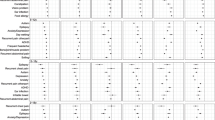
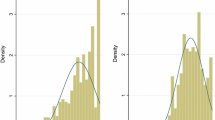
Objectives To estimate the prevalence and losses in quality-adjusted life years (QALYs) associated with 20 child health conditions. Methods Using data from the 2009–2010 National Survey of Children with Special Health Care Needs, preference weights were applied to 14 functional difficulties to summarize the quality of life burden of 20 health conditions. Results Among the 14 functional difficulties, “a little trouble with breathing” had the highest prevalence (37.1 %), but amounted to a loss of just 0.16 QALYs from the perspective of US adults. Though less prevalent, “a lot of behavioral problems” and “chronic pain” were associated with the greatest losses (1.86 and 3.43 QALYs). Among the 20 conditions, allergies and asthma were the most prevalent but were associated with the least burden. Muscular dystrophy and cerebral palsy were among the least prevalent and most burdensome. Furthermore, a scatterplot shows the association between condition prevalence and burden. Conclusions In child health, condition prevalence is negatively associated with quality of life burden from the perspective of US adults. Both should be considered carefully when evaluating the appropriate role for public health prevention and interventions.

Similar content being viewed by others
References
Bumbalo, J., Ustinich, L., Ramcharran, D., et al. (2005). Economic impact on families caring for children with special health care needs in New Hampshire: The effect of socioeconomic and health-related factors. Maternal and Child Health Journal, 9(2), S3–S11. doi:10.1007/s10995-005-4350-3.
DeRigne, L. (2012). The employment and financial effects on families raising children with special health care needs: An examination of the evidence. Journal of Pediatric Health Care, 26(4), 283–290. doi:10.1016/j.pedhc.2010.12.006.
McIntyre, L. L., Blacher, J., & Baker, B. L. (2002). Behaviour/mental health problems in young adults with intellectual disability: The impact on families. Journal of Intellectual Disability Research, 46, 239–249. doi:10.1046/j.1365-2788.2002.00371.x.
Quach, J., Oberklaid, F., Gold, L., et al. (2014). Primary health-care costs associated with special health care needs up to age 7 years: Australian population-based study. Journal of Paediatrics and Child Health, 50(10), 768–774. doi:10.1111/jpc.12649.
McPherson, M., Arango, P., Fox, H., et al. (1998). A new definition of children with special health care needs. Pediatrics, 102(1), 137–140. doi:10.1542/peds.102.1.137.
Centers for Disease Control and Prevention (CDC). State and Local Area Integrated Telephone Survey-National Survey of Children with Special Health Care Needs. CDC/National Center for Health Statistics http://www.cdc.gov/nchs/slaits/cshcn.htm. Access: 9/5/2014).
Child and Adolescent Health Measurement Initiative (2012). “2009/10 NS-CSHCN: Health conditions and functional difficulties.” Data resource center, supported by cooperative agreement 1-U59-MC06980-01 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Available at www.childhealthdata.org. Revised 01/27/2012.
Gold, M. R., Siegel, J. E., Russell, L. B., & Weinstein, M. C. (Eds.). (1996). Cost-effectivenss in health and medicine. New York: Oxford University Press.
Stabile, M., & Allin, S. (2012). The economic costs of childhood disability. Future of Children, 22(1), 65–96.
Kuo, D. Z., Cohen, E., Agrawal, R., et al. (2011). A national profile of caregiver challenges among more medically complex children with special health care needs. Archives of Pediatrics and Adolescent Medicine, 165(11), 1020–1026.
Smith, A. L., Romski, M., Sevcik, R. A., et al. (2014). Parent stress and perceptions of language development: Comparing down syndrome and other developmental disabilities. Family Relations, 63(1), 71–84. doi:10.1111/fare.12048.
Szilagyi, P. G. (2012). Health insurance and children with disabilities. Future of Children, 22(1), 123–148.
Viana, M. C., Gruber, M. J., Shahly, V., et al. (2013). Family burden related to mental and physical disorders in the world: Results from the WHO World Mental Health (WMH) surveys. Revista Brasileira de Psiquiatria, 35(2), 115–125.
Drummond, M., Brixner, D., Gold, M., et al. (2009). Toward a consensus on the QALY. Value Health, 12, S31–S35. doi:10.1111/j.1524-4733.2009.00522.x.
Fryback, D. G., & Lawrence, W. F, Jr. (1997). Dollars may not buy as many QALYs as we think: a problem with defining quality-of-life adjustments. Medical Decision Making, 17(3), 276–284.
World Health Organization (WHO) Essential medicines and health products information portal. Introduction to Drug Utilization Research 2003.
Griebsch, I., Coast, J., & Brown, J. (2005). Quality-adjusted life-years lack quality in pediatric care: A critical review of published cost-utility studies in child health. Pediatrics, 115(5), E600–E614. doi:10.1542/peds.2004-2127.
Carroll, A. E., & Downs, S. M. (2009). Improving decision analyses: Parent preferences (utility values) for pediatric health outcomes. Journal of Pediatrics, 155(1), 21–25. doi:10.1016/j.jpeds.2009.01.040.
Friedman, J. Y., Reed, S. D., Weinfurt, K. P., et al. (2004). Parents’ reported preference scores for childhood atopic dermatitis disease states. BMC Pediatrics, 4(1), 21. doi:10.1186/1471-2431-4-21.
Hauber, A. B., Itzler, R., Johnson, F. R., et al. (2011). Healthy-days time equivalents for outcomes of acute rotavirus infections. Vaccine, 29(45), 8086–8093. doi:10.1016/j.vaccine.2011.08.041.
Secnik, K., Matza, L. S., Cottrell, S., et al. (2005). Health state utilities for childhood attention-deficit/hyperactivity-disorder based on parent preferences in the United Kingdom. Medical Decision Making, 25(1), 56–70. doi:10.1177/0272989x04273140.
Ungar, W. (2010). Economic evaluation in child health. Oxford: Oxford University Press.
Craig, B. M., Brown, D. S., & Reeve, B. B. (2015). The value adults place on child health and functional status. Value Health, 18(4), 449–456. doi:10.1016/j.jval.2015.02.012.
Data Resource Center for Child & Adolescent Health. National Surey of Children with Speacial Health Care Needs (2009/10 NS-CSHCN): FAST FACTS about the SURVEY. http://childhealthdata.org/docs/default-document-library/ns-cshcn-fast-facts-2009.pdf. Accessed 26 Sept 2014.
National Center for Health Statistics. Centers for Disease Control and Prevention. 2009-2010 National Survey of Children with Special Health Care Needs. http://www.cdc.gov/nchs/data/slaits/NS_CSHCN_Questionnaire_09_10.pdf. Accessed 26 Sept 2014.
Mulhern, B., Bansback, N., Brazier, J., et al. (2014). Preparatory study for the revaluation of the EQ-5D tariff: Methodology report. Health Technology Assessment, 18(12), 1–191. doi:10.3310/hta18120.
Petrou, S., Kandala, N. B., Robinson, A., et al. (2013). A person trade-off study to estimate age-related weights for health gains in economic evaluation. PharmacoEconomics, 31(10), 893–907. doi:10.1007/s40273-013-0085-y.
Prieto, L., & Sacristan, J. A. (2003). Problems and solutions in calculating quality-adjusted life years (QALYs). Health and Quality of Life Outcomes,. doi:10.1186/1477-7525-1-80.
Lenert, L., & Kaplan, R. M. (2000). Validity and interpretation of preference-based measures of health-related quality of life. Medical Care, 38(9), 138–150.
Torrance, G. W. (1987). Utility approach to measuring health-related quality of life. Journal of Chronic Diseases, 40(6), 593–603.
Craig, B. M., Brown, D. S., Reeve, B. Valuation of Child Behavioral Problems from the Perspective of US Adults. Medical Decision Making (in press).
Craig, B. M., Reeve, B. B., Brown, P. M., et al. (2014). US valuation of health outcomes measured using the PROMIS-29. Value Health, 17(8), 846–853. doi:10.1016/j.jval.2014.09.005.
Bloom, B., Jones, L. I., Freeman, G. (2013). Summary health statistics for U.S. children: National Health Interview Survey, 2012.
Ladapo, J. A., Neumann, P. J., Keren, R., et al. (2007). Valuing children’s health: A comparison of cost-utility analyses for adult and paediatric health interventions in the US. PharmacoEconomics, 25(10), 817–828.
Ungar, W. J. (2011). Challenges in health state valuation in paediatric economic evaluation are QALYs contraindicated? PharmacoEconomics, 29(8), 641–652.
Gerald, J. K., McClure, L. A., Harrington, K. F., et al. (2012). Measurement characteristics of the pediatric asthma health outcome measure. Journal of Asthma, 49(3), 260–266. doi:10.3109/02770903.2012.656863.
Baxter, A. J., Brugha, T. S., Erskine, H. E., et al. (2014). The epidemiology and global burden of autism spectrum disorders. Psychological Medicine,. doi:10.1017/s003329171400172x.
Arbelle, J. E., Chodick, G., Goldstein, A., et al. (2014). Multiple chronic disorders-health care system’s modern challenge in the Maccabi Health Care System. Israel Journal of Health Policy Research, 3, 29. doi:10.1186/2045-4015-3-29.
Bitsko, R. H., Visser, S. N., Schieve, L. A., et al. (2009). Unmet health care needs among CSHCN with neurologic conditions. Pediatrics, 124(Suppl 4), S343–S351. doi:10.1542/peds.2009-1255D.
Zhong, W., Finnie, D. M., Shah, N. D., et al. (2014). Effect of multiple chronic diseases on health care expenditures in childhood. Journal of Primary Care & Community Health,. doi:10.1177/2150131914540916.
Blackman, J. A., Gurka, M. J., Gurka, K. K., et al. (2011). Emotional, developmental and behavioural co-morbidities of children with chronic health conditions. Journal of Paediatrics and Child Health, 47(10), 742–747. doi:10.1111/j.1440-1754.2011.02044.x.
Steele, R., Siden, H., Cadell, S., et al. (2014). Charting the territory: Symptoms and functional assessment in children with progressive, non-curable conditions. Archives of Disease in Childhood, 99(8), 754–762. doi:10.1136/archdischild-2013-305246.
Gortmaker, S. L., Walker, D. K., Weitzman, M., et al. (1990). Chronic conditions, socioeconomic risks, and behavioral problems in children and adolescents. Pediatrics, 85(3), 267–276.
Acknowledgments
The authors thank Catherine Blackburn and Carol Templeton for their contributions to references and editing of this paper, respectively.
Funding
Funding support for this research was provided by a Grant from the National Institutes of Health, Department of Health and Human Services, through the National Cancer Institute (1R01CA160104) and Dr. Craig’s support account at Moffitt Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Craig, B.M., Hartman, J.D., Owens, M.A. et al. Prevalence and Losses in Quality-Adjusted Life Years of Child Health Conditions: A Burden of Disease Analysis. Matern Child Health J 20, 862–869 (2016). https://doi.org/10.1007/s10995-015-1874-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1874-z