Abstract
Breastfeeding self-efficacy interventions are important for improving breastfeeding outcomes. However, the circumstances that may influence the effectiveness of the interventions are unclear, especially in the context of hospitals with suboptimal infant feeding practices. Thus, we aimed to evaluate the effect of a self-efficacy intervention on breastfeeding self-efficacy and exclusive breastfeeding, and further assessed the difference in its effect by hospital-routine type. In this intervention study with a control group, 781 pregnant women were recruited from 2 “Baby-Friendly”-certified hospitals (BFH) and 2 non-Baby-Friendly Hospitals (nBFH) in Japan, and were allocated to an intervention or control group. Participants in the intervention group were provided with a breastfeeding self-efficacy workbook in their third trimester. The primary outcome was breastfeeding self-efficacy and the secondary outcome was infant feeding status. All analyses were stratified by the type of hospital, BFH or nBFH. In BFHs, the intervention improved both breastfeeding self-efficacy through 4 weeks postpartum (p = 0.037) and the exclusive breastfeeding rate at 4 weeks postpartum (AOR 2.32, 95 % CI 1.01–5.33). In nBFHs, however, no positive effect was observed on breastfeeding self-efficacy (p = 0.982) or on the exclusive breastfeeding rate at 4 weeks postpartum (AOR 0.97, 95 % CI 0.52–1.81); in nBFHs, supplementation was provided for breastfed infants and the mother and infant were separated in the vast majority of cases. Infant feeding status at 12 weeks was not improved in either hospital type. The intervention improved breastfeeding self-efficacy and exclusive breastfeeding at 4 weeks postpartum only in BFHs. When breastfeeding self-efficacy interventions are implemented, hospital infant feeding practices may need to be optimized beforehand.
Similar content being viewed by others
Background
Breastfeeding is the normative standard for infant feeding and is beneficial to the health of both mother and infant. In developed and developing countries alike, numerous studies provide strong evidence that breastfeeding decreases the incidence and/or severity of a wide range of diseases in infants and mothers [1, 2]. Thus, international and national organizations have been promoting exclusive breastfeeding for the first 6 months of life [2–4].
Similar to many countries in the world [5], in Japan, many mothers prematurely discontinue exclusive breastfeeding against their prenatal intention to breastfeed. Although a nationwide survey reported that 96 % of Japanese women intend to breastfeed prenatally [6], many of them start supplementation with infant formula after delivery. According to a Japanese national report published in 2010, while the rate for any breastfeeding during the first 8 weeks of life was 95 %, 44 % of infants under 8 weeks of age received infant formula in addition to breast milk [7]. A literature review of 12 breastfeeding studies in Japan found that maternal psychometric factors, including breastfeeding confidence, are associated with breastfeeding outcomes [8]. Thus, interventions are warranted to promote exclusive breastfeeding through influencing maternal psychometric factors.
Recently, maternal breastfeeding self-efficacy has been highlighted as an important psychometric factor for improving breastfeeding outcomes [9]. Breastfeeding self-efficacy is defined as a mother’s confidence in her ability to breastfeed her new infant [10] and has been positively associated with breastfeeding duration and exclusivity in various cultures and age groups [11–15]. Theoretically, breastfeeding self-efficacy is influenced by the following four main sources of information: (a) performance accomplishments (e.g., past breastfeeding experiences), (b) vicarious experiences (e.g., watching other women breastfeed, peer counseling), (c) verbal persuasion (e.g., encouragement from influential others such as friends, family, and lactation consultants), and (d) influence of one’s physiological and/or affective states (e.g., pain, fatigue, anxiety, stress) [10, 16].
Various studies have been conducted to evaluate interventions based on self-efficacy theory [17–20]. In a randomized controlled trial involving 90 pregnant women in Australia, a self-efficacy theory-based workbook improved breastfeeding exclusivity at 4 weeks postpartum by enhancing breastfeeding self-efficacy [17]. Similarly, in two other Canadian studies, breastfeeding self-efficacy and exclusivity improved following implementation of self-efficacy interventions [18, 20]. These results provide evidence that self-efficacy is an important variable and that interventions based on self-efficacy theory can enhance breastfeeding outcomes.
However, very few studies have examined the circumstances that may influence the effectiveness of breastfeeding self-efficacy interventions. Specifically, the effectiveness of self-efficacy interventions is unclear in the case of mothers who receive suboptimal infant feeding support in hospitals. Certain routine hospital practices interfere with breastfeeding, such as restricted breastfeeding, separating mothers and newborns, and supplementation of breast milk with infant formula [21–23]. These routine practices probably interfere with development of breastfeeding self-efficacy as well. For example, supplementation provided to a breastfed infant may lead to lower breastfeeding self-efficacy through a mother’s perception of poor performance accomplishment, a factor that can negatively influence an individual’s self-efficacy [10]. Therefore, the effectiveness of self-efficacy interventions may be reduced in the cases of mothers who receive suboptimal infant feeding support in hospitals.
Unfortunately, infant feeding practices are not optimal in the majority of hospitals in Japan. According to a nationwide survey of 1,238 obstetric wards, starting rooming-in within 6 h of birth was a general practice in only 16.7 % of them, while giving supplementation before the first breastfeeding session was a routine practice in 71.6 % of them [24]. To determine the utility of breastfeeding self-efficacy interventions in Japan, interventions should be evaluated in hospitals where routine practices are not optimal for infant feeding.
Thus, we aimed to evaluate the effect of a self-efficacy intervention on breastfeeding self-efficacy and exclusive breastfeeding in two types of hospitals: (a) hospitals in which infant feeding practices are optimized according to World Health Organization (WHO) recommendations, and (b) hospitals in which these practices are not optimized for infant feeding.
Methods
Sample
For this intervention study with a control group, participants were recruited from the antenatal wards of four Japanese hospitals selected by convenience sampling between August 2010 and January 2011. Two hospitals were certified as Baby-Friendly Hospitals (BFH) and two hospitals were non-Baby-Friendly Hospitals (nBFH), according to the criteria established by the United Nations Children’s Fund (UNICEF) and WHO [3]. Eligible participants included all pregnant women in their third trimester who were (a) 16 years of age or older, (b) able to read and write Japanese, and (c) expected to have a singleton birth. Mothers were excluded if they intended to formula feed, had a pregnancy that ended in either miscarriage or stillbirth, or had a medical factor that could significantly interfere with breastfeeding.
Procedure
Figure 1 shows participant flow through the study. Participants were allocated to either the intervention group or the control group. In Japan, women generally stay in hospital for about 5 days after delivery and often share a room with other women. Thus, to avoid contact between women in the intervention group and those in the control group during hospitalization, we employed the following method instead of individual randomization. In two of the hospitals (one BFH, one nBFH) for the first 2 months of recruitment, all eligible women were assigned to the intervention group when they reached the third trimester. After a month’s interval, all eligible women who reached their third trimester and were not in the intervention group were assigned to the control group for the following 2 months of recruitment. In the other two hospitals (one BFH, one nBFH), the order of assignment to the intervention and control groups was reversed.
Participant flow through the study. Note. aExcluded when medical conditions were detected. The medical conditions for exclusion were as follows: stillbirth (n = 1), delivery before 37 weeks of gestation (n = 23), birth weight under 2,500 g (n = 38), admission to NICU (n = 8), cleft palate in the infant (n = 1), transfer to other hospital of the mother (n = 3) or infant (n = 7), being under medical care for depression (n = 1), prevention from breastfeeding (n = 7) and/or separation from infant (n = 4) for more than 24 h. The total numbers do not equal the sum of those in the flow chart because of overlapping conditions
Midwives in the hospitals assessed the eligibility of women and provided a study package to eligible women who were waiting for an antenatal appointment. The study package contained a booklet with a detailed explanation of the study and the first questionnaire to assess baseline breastfeeding self-efficacy. Participants who gave their consent by completing the informed consent procedures, approved by the ethical committee of the University of Tokyo and the review boards of the participating hospitals, completed the baseline questionnaire and dropped it in a collection box in the hospitals. Women allocated to the control group had access to the conventional in-hospital and community support services. Women allocated to the intervention group also had access to the conventional support services, in addition to the self-efficacy intervention.
Follow-up surveys were conducted three times in the first 12 weeks postpartum. The first follow-up survey was conducted before hospital discharge to assess breastfeeding self-efficacy and infant feeding practices in the hospitals. The second follow-up survey was conducted when the mothers returned to the hospital for their infants’ 1-month health check-up to assess breastfeeding self-efficacy and infant feeding status at 4 weeks postpartum. The last follow-up survey was conducted to assess infant feeding status at 12 weeks postpartum. For the first and second follow-up surveys, participants received questionnaires from the staff members of the hospital and dropped them in a collection box after completion. For the last follow-up survey, the participants were mailed the questionnaire in a reply-paid envelope.
Intervention
The intervention in this study was to provide a breastfeeding self-efficacy workbook to women in their third trimester. Women in the intervention groups were encouraged to complete the workbook before delivery. The authors developed a Japanese version of the workbook used by Nichols et al. [17] in a self-efficacy enhancing intervention study in Australia. The original workbook was developed to reflect Dennis’s [10] breastfeeding self-efficacy framework and the four sources of self-efficacy information as specified by Bandura [16, 25]. It contained the following six sections: Section 1, “Exploring Aspects of Confidence” (providing an explanation of the workbook); Section 2, “Mastery” (performance accomplishment); Section 3, “Building Confidence by Learning from others” (vicarious experiences); Section 4, “Using Encouragement” (verbal persuasion); Section 5, “Exploring How We Respond to Stress” (physical responses); and Section 6, “Keeping Motivated” (concluding the workbook) [17]. The information in the workbook is solution-oriented to facilitate positive cognitive appraisal [17, 25].
The authors translated the original English workbook into Japanese. Although the concept and the basic structure of the workbook were maintained, several parts were modified to make it more suitable for Japanese mothers. Specifically, the breastfeeding stories from Australia were changed to appeal to Japanese mothers. Additionally, a number of descriptive passages were replaced with illustrations or short comics that Japanese women would readily understand. After these modifications, a panel of three breastfeeding experts, two lactation consultants, and a university professor of nursing evaluated the content of the workbook and judged it to be relevant to mothers in Japan.
The Japanese workbook was then pilot-tested with 18 pregnant or breastfeeding women. Five out of the 18 women had a one-on-one debriefing session with the first author after completing the workbook. The other 13 women participated in a group discussion chaired by the first author after completion of the workbook. Based on their feedback regarding completion time, readability, and comprehension of the workbook, some modifications were made to the expressions, and language used throughout the workbook. Finally, the 22-page Japanese version of the breastfeeding self-efficacy workbook was completed, with more than half of the content described in illustrations or short comics and an average completion time of about 30 min.
Outcome Variables
Breastfeeding Self-Efficacy
This outcome was assessed using the Japanese version of the Breastfeeding Self Efficacy Scale-Short Form (BSES-SF) [14], a 14-item, self-report instrument developed to assess breastfeeding self-efficacy. All items are anchored with a 5-point Likert-type scale where 1 = not at all confident and 5 = very confident. Items are presented positively and summed to produce a total score ranging from 14 to 70, with higher scores indicating higher levels of breastfeeding self-efficacy. In this study, Cronbach’s α coefficient for the Japanese version of the BSES-SF at baseline, before hospital discharge, and at 4 weeks postpartum was 0.95, 0.95, and 0.95, respectively.
Infant Feeding Status
This outcome was measured using two separate methods: 24-h recall and history since discharge. Current infant feeding status was measured by 24-h recall at 4 and 12 weeks and classified into six categories based on Labbok’s breastfeeding classification: (1) full breastfeeding (exclusive and almost exclusive breastfeeding), (2) high partial breastfeeding (breastfeeding for more than 80 % of the time), (3) medium partial breastfeeding (breastfeeding for 20–80 % of the time), (4) low partial breastfeeding (breastfeeding for less than 20 % of the time), (5) token breastfeeding (occasional breastfeeding, not for nutritive purposes), and (6) formula feeding (only formula feeding) [26, 27]. Further, infant feeding history since discharge was measured and classified as (1) exclusive breastfeeding (no liquid or solid foods other than breast milk given to the infant after discharge) and (2) no exclusive breastfeeding (supplementation with formula feeding, or no breastfeeding).
Maternal Characteristics
Established correlates of breastfeeding duration and exclusivity were measured as shown in Table 1 [9, 28–30]. In addition to sociodemographic background characteristics, the following maternal psychometric factors were measured: breastfeeding intention, maternal infant feeding attitude (Iowa Infant Feeding Attitude Scale [IIFAS]) [31], family support (Family Apgar) [32, 33], and depression (Edinburgh Postnatal Depression Scale [EPDS]) [34, 35]. Labor and delivery and neonatal information was also collected before hospital discharge.
Infant Feeding Practices at Hospitals
This outcome was measured as maternal perceptions of compliance to the “Ten steps to successful breastfeeding” recommended by WHO and UNICEF, the guidelines meant to facilitate optimal infant feeding practices in hospitals [3]. Mothers answered questions about infant feeding practices at their hospitals before discharge, based on their personal experiences. Data on Step 1, “Have a written breastfeeding policy that is routinely communicated to all health care staff,” and Step 2, “Train all health care staff in skills necessary to implement this policy,” were not available from the mother’s perspective; thus, for the current study, we collected data only on Steps 3 through 10. With regard to Step 6, “Give newborn infants no food or drink other than breast milk, unless medically indicated,” supplementation provided to breastfed infants was measured. If an infant received any supplementation, women further reported the reason given by medical staff. Considering the typical infant feeding practices in Japanese hospitals [24], “Rooming-in” (Step 7) was defined as starting rooming-in within 3 h of delivery and continuing the practice day and night until discharge, and “Fostering the establishment of breastfeeding support groups” (Step 10) was defined by the mother’s knowledge of any breastfeeding support group.
Completion and Use of Workbook
Women in the intervention group reported how much of the content of the workbook they read, and completed the “Q&A” section of the survey before discharge. In the survey at 12 weeks postpartum, they further reported whether they had reviewed the workbook after initiation of breastfeeding and assessed if the workbook was beneficial for breastfeeding.
Data Analysis
A p value of 0.05 or less was considered to indicate significance. All analyses were conducted with SPSS version 21. The data are presented using means and standard deviations for continuous variables, and frequencies and proportions for categorical variables. All variables were examined for normality of distribution. For categorical comparison of data, Chi square or Fisher’s exact tests were used. Differences in the means of continuous variables were tested using independent sample t tests. To avoid breaking the balance of assignment to the two groups, all analysis was made on an intention-to-treat basis, except for 71 cases that were excluded because either the mother or her infant developed some medical condition after enrollment in the study.
To test the effect of the intervention on breastfeeding self-efficacy, a multivariate generalized estimating equation (GEE) analysis was performed. In this study, factors known to be associated with breastfeeding were considered likely to influence the effect of the intervention. Thus, covariates were selected for entry into the model from the variables presented in Table 1 using a forward selection procedure (cutoff for model entry, p < 0.05). The variable “single mother” was excluded from the process because it lacks variability.
To analyze the effect of the intervention on exclusive breastfeeding, multiple logistic regression analysis was performed. Infant feeding and intervention group status were included in the model, and additional variables were selected in a similar manner to the model for breastfeeding self-efficacy.
The study was originally powered to detect a 10 % difference between the 2 groups in the full breastfeeding rate at 12 weeks postpartum, with a power of 80 % and a two-sided statistical significance level of 5 %. Using data from a previous national survey [6], we assumed the full breastfeeding rate of the control group as 20 %. Allowing for potential dropouts, we thus aimed to recruit 900 participants.
All the analyses were stratified by hospital type (BFH or nBFH) after knowing that the impact of the intervention on breastfeeding self-efficacy was quite different across the different types of hospitals. After stratification by hospital type, we ultimately recruited 276 participants in BFHs and 505 participants in nBFHs. This sample size resulted in an effect size that can be detected at a power of 80 % were 20 % in BFH and 14 % in nBFH.
Results
Baseline characteristics of the participants were not significantly different between the intervention group and the control group in either the BFHs or the nBFHs, with the exception of birth weight and previous experience of breastfeeding for more than 3 months in nBFHs (Table 1).
Completion and Use of Workbook
The majority of the participants in the intervention group read most of the contents of the workbook in both the BFHs (n = 72, 72.0 %) and the nBFHs (n = 121, 71.2 %). Among them, 42 (58.3 %) in the BFHs and 79 (65.3 %) in the nBFHs also responded to the questions in the workbook. While 35.4 % (n = 35) of the women who received the workbook in the BFHs reviewed the workbook after they initiated breastfeeding, 39.9 % (n = 63) did so in the nBFHs (p = 0.468). Among the women who returned the evaluation of the workbook, the majority assessed the workbook as being beneficial for breastfeeding in both the BFHs (n = 68, 72.4 %) and the nBFHs (n = 112, 71.3 %, p = 0.960).
Breastfeeding Self-Efficacy
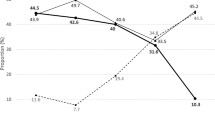
Figure 2 shows the changes in BSES-SF scores from baseline to 4 weeks postpartum in the intervention and control groups in both types of hospitals. BESE-SF score increased with time within all groups. While the increase was larger in the intervention group than in the control group in BFHs, it was similar between the two groups in nBFHs. After controlling for potential confounding factors and time, the intervention resulted in an increase in the BSES-SF total score through 4 weeks postpartum in BFHs, but it had no effect on breastfeeding self-efficacy in nBFHs (Table 2).
Breastfeeding self-efficacy scores from baseline to 4 weeks postpartum in intervention and control groups. aThe Japanese version of the Breastfeeding Self-Efficacy Scale-Short Form, ranges from 14 to 70, with higher scores indicating higher levels of breastfeeding self-efficacy. Solid line with diamond indicates Baby-Friendly Hospitals, intervention, dotted line with diamond indicates Baby-Friendly Hospitals, control, solid line with triangle indicates non-Baby-Friendly Hospitals, intervention, dotted line with triangle indicates non-Baby-Friendly Hospitals, control
Infant Feeding Status
Table 3 shows infant feeding status distribution in intervention and control groups. Infant feeding status was substantially different between mothers in BFHs and those in nBFHs at 4 and 12 weeks postpartum. The impact of the intervention on infant feeding status was also remarkably different between mothers in BFHs and those in nBFHs. The intervention improved the exclusive breastfeeding rate at 4 weeks postpartum in BFHs. Also, the full breastfeeding rate at 4 weeks postpartum was higher in the intervention group than in the control group; however, the difference was not statistically significant. In nBFHs, no positive effect of the intervention was observed in infant feeding status at 4 weeks postpartum. In addition, the intervention had no effect at 12 weeks postpartum in either BFH or nBFH hospitals.
Infant Feeding Practices at Hospitals
All the infant feeding practices investigated were significantly different between the BFHs and nBFHs, with the exception of Step 10. Most importantly, while the majority of participants in BFHs reported giving no supplementation to breastfed infants and rooming-in, only a few reported giving no supplementation and rooming-in in nBFHs (Table 4).
The main reason given by mothers in nBFHs for supplementation was staff members’ perception of insufficient milk supply. Out of 427 women who participated in the survey before discharge in nBFHs, 68.1 % (n = 291) of the women reported that the hospital staff members assessed their infants as needing supplementation because of insufficient milk supply. Insufficient milk supply was significantly less common in BFHs [n = 25 (10.9 %), p < 0.001].
Discussion
Overall, our study had three major findings. First, the self-efficacy intervention enhanced breastfeeding self-efficacy and improved the exclusive breastfeeding rate at 4 weeks postpartum in BFHs. Second, such positive effects through the intervention were not observed in nBFHs. Finally, breastfeeding exclusivity at 12 weeks postpartum was not improved following the intervention, even in BFHs.
The findings suggest that the self-efficacy intervention improved breastfeeding self-efficacy and short-term exclusive breastfeeding in BFHs. After controlling for confounding factors, women in the intervention group were found to have a significantly greater increase in breastfeeding self-efficacy than did women in the control group in BFHs. Equally important is the finding that the exclusive breastfeeding rate at 4 weeks postpartum was improved in BFHs. These positive effects are consistent with other breastfeeding self-efficacy intervention studies which have evaluated interventions based on self-efficacy theory [17–20]. In BFHs, therefore, an intervention to enhance breastfeeding self-efficacy is a promising approach to improve exclusive breastfeeding.
However, the intervention did not have a positive effect on breastfeeding self-efficacy and exclusive breastfeeding in nBFHs. Consistent with the theory that self-efficacy improves with repeated practice of a certain performance [10, 16, 25], the breastfeeding self-efficacy score increased as time passed after the initiation of breastfeeding both in the intervention group and in the control group in BFHs and nBFHs alike. However, although women in nBFHs used the intervention workbook more intensively than did women in BFHs, the intervention did not have a significant effect on breastfeeding self-efficacy scores in nBFHs. This is a clinically important finding, especially for regions where infant feeding practices in hospitals are often suboptimal. It suggests that hospital routine can hinder the development of breastfeeding self-efficacy, despite the willingness of and effort put in by women to improve breastfeeding self-efficacy.
In this study, the following obstacles were found in nBFHs: supplementation to breastfed infants, no rooming-in for the day and night, and provision of artificial teats to breastfed infants. In addition, compared with women in BFHs, significantly fewer women in nBFHs reported receiving information about the benefits and management of breastfeeding, instructions on how to breastfeed, early initiation of breastfeeding, and breastfeeding on demand. To enhance breastfeeding self-efficacy, infant feeding practices at hospitals may need to be reformed as a prerequisite for an effective intervention targeting breastfeeding women.
We found that the intervention was not effective in improving infant feeding status at 12 weeks postpartum in either hospital type. One possible explanation for this is related to the timing of the intervention. In this study, the self-efficacy workbook was provided to women in their third trimester. Additional intervention after mothers initiate breastfeeding may be required to enhance the impact of the intervention to improve exclusive breastfeeding rates after 4 weeks postpartum.
The intervention in this study was to provide an educational workbook; the utilization of the workbook was not considered. Following the principle of intention-to-treat, even a mother who did not read the workbook at all was still included in the intervention group in all analytical processes. In this study, about one fourth of women in the intervention group did not read the workbook at all. In clinical setting, the utilization of the workbook may be different from that observed in this study in ways that may lead to a different magnitude of effectiveness. Therefore, before clinical use of the workbook, best ways to increase utilization of the workbook should be explored.
This study has several limitations. First, although the results indicated a clear difference in the impact of the self-efficacy intervention between BFHs and nBFHs, the study did not directly measure the influence of hospital infant feeding practices on the impact of the intervention. Thus, some unknown factors may possibly have contributed to the difference in the impact of the intervention between the two types of hospitals. Second, the four study sites were not systematically selected. However, hospital practices reported in the two nBFHs were similar to the results of a nationwide survey in 2002 [24]. In addition, the results suggest that the practices in the two BFHs followed the recommendations outlined by the Baby-Friendly Hospital Initiative [3]. Thus, the four hospitals in this study closely reflected the general tendency of hospital practices in both BFHs and nBFHs in Japan. The characteristics of the participants were also not remarkably different from those found in a previous national survey among mothers with infants aged 6 months [29]. Finally, contamination between intervention and control groups cannot be totally ruled out. Although a month interval was set between the recruitment of the two groups, participants might have had the opportunity to observe and influence each other.
Since the intervention was not a double-blinded, randomized controlled study, several additional issues should be considered when implementing the results. First, the characteristics of participants were adjusted statistically; therefore, there might be differences in unmeasured factors between the intervention and control groups. Moreover, intentional and unintentional influence from hospital staff also cannot be excluded because they had the option to know their clients’ intervention group status if they so chose. Despite these limitations, this is an important study for maternal and child health, as it is the first to show that the impact of a breastfeeding self-efficacy intervention for women can differ according to the practices followed in different hospital settings.
Conclusion
In conclusion, the intervention improved breastfeeding self-efficacy and exclusive breastfeeding at 4 weeks postpartum only in BFHs. However, no positive effect was observed in nBFHs, where supplementation to breastfed infants and separation of mother and infant are common practices. When breastfeeding self-efficacy interventions are implemented to improve breastfeeding exclusivity, hospital practices may need to be optimized beforehand. Additional studies are warranted to directly measure the influence of hospital practices on the impact of a self-efficacy intervention on breastfeeding outcomes. Furthermore, supplemental intervention may be required to improve exclusive breastfeeding for longer than 4 weeks even in BFHs.
References
Ip, S., Chung, M., & Raman, G., et al. (2007). Breastfeeding and maternal and infant health outcomes in developed countries: Evidence report/technology assessment no. 153. Rockville, MD: Agency for Healthcare research and Quality; AHRQ Publication no. 07-E.
American Academy of Pediatrics, Section on Breastfeeding. (2012). Breastfeeding and the use of human milk. Pediatrics, 129, e827–e841.
WHO & UNICEF. (2009). Baby-Friendly Hospital Initiative-Revised, Updated, and Expanded for Integrated Care, 2009. Available at: http://www.unicef.org/nutrition/index_24850.html. Accessed December 28, 2011.
Mass, S. B. (2011). Supporting breastfeeding in the United States: The Surgeon General’s call to action. Current Opinion in Obstetrics and Gynecology, 23, 460–464.
WHO. (2011). World Health Statistics 2011. Geneva: WHO.
Equal Employment, Children and Families Bureau, Japanese Ministry of Health, Labour and Welfare. (2006). Report on infant feeding in Japan. Tokyo, Japan: Ministry of Health Labour and Welfare (in Japanese).
Equal Employment, Children and Families Bureau, Japanese Ministry of Health Labour and Welfare. (2011). Survey on the growth of infants and preschool children in Japan, 2010. Tokyo, Japan: Equal employment, Children and Families Bureau, Ministry of Health Labour and Welfare (in Japanese).
Inoue, M., Binns, C. W., Otsuka, K., Jimba, M., & Matsubara, M. (2012). Infant feeding practices and breastfeeding duration in Japan: A review. International Breastfeeding Journal, 25, 15.
Meedya, S., Fahy, K., & Kable, A. (2010). Factors that positively influence breastfeeding duration to 6 months: A literature review. Women Birth, 23, 135–145.
Dennis, C. L. (1999). Theoretical underpinnings of breastfeeding confidence: A self-efficacy framework. Journal of Human Lactation, 15, 195–201.
Blyth, R., Creedy, D. K., Dennis, C. L., et al. (2002). Effect of maternal confidence on breastfeeding duration: An application of breastfeeding self-efficacy theory. Birth, 29, 278–284.
Dennis, C. L., Heaman, M., & Mossman, M. (2011). Psychometric testing of the breastfeeding self-efficacy scale-short form among adolescents. Journal of Adolescent Health, 49, 265–271.
Oliver-Roig, A., d’Anglade-González, M. L., García-García, B., et al. (2012). The Spanish version of the Breastfeeding Self-Efficacy Scale-Short Form: reliability and validity assessment. International Journal of Nursing Studies, 49, 169–173.
Otsuka, K., Dennis, C. L., Tatsuoka, H., & Jimba, M. (2008). The relationship between breastfeeding self-efficacy and perceived insufficient milk among Japanese mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 37, 546–555.
Aluş Tokat, M., Okumuş, H., & Dennis, C. L. (2010). Translation and psychometric assessment of the Breast-feeding Self-Efficacy Scale-Short Form among pregnant and postnatal women in Turkey. Midwifery, 26, 101–108.
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–215.
Nichols, J., Schutte, N. S., Brown, R. F., et al. (2009). The impact of a self-efficacy intervention on short-term breast-feeding outcomes. Health Education & Behavior, 36, 250–258.
McQueen, K. A., Dennis, C. L., Stremler, R., & Norman, C. D. (2011). A pilot randomized controlled trial of a breastfeeding self-efficacy intervention with primiparous mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 40, 35–46.
Noel-Weiss, J., Bassett, V., & Cragg, B. (2006). Developing a prenatal breastfeeding workshop to support maternal breastfeeding self-efficacy. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 35, 349–357.
Noel-Weiss, J., Rupp, A., Cragg, B., et al. (2006). Randomized controlled trial to determine effects of prenatal breastfeeding workshop on maternal breastfeeding self-efficacy and breastfeeding duration. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 35, 616–624.
Hill, P. D., Humenick, S. S., Brennan, M. L., & Woolley, D. (1997). Does early supplementation affect long-term breastfeeding? Clinical Pediatrics, 36, 345–350.
Renfrew, M. J., Lang, S., Martin, L., & Woolridge, M. W. (2000). Feeding schedules in hospitals for newborn infants. Cochrane Database of Systematic Reviews, 2, CD000090.
Declercq, E., Labbok, M. H., Sakala, C., & O’Hara, M. (2009). Hospital practices and women’s likelihood of fulfilling their intention to exclusively breastfeed. American Journal of Public Health, 99, 929–935.
Takeshi, H., Takeo, S., Taku, Y., & Michiko, N. (2002). Starting prevention of childrearing anxiety in perinatal period. Tokyo: Japanese Ministry of Health, Labour, and Welfare.
Bandura, A. (1997). Self-efficacy: The exercise of control. New York, NY: Worth Publishers.
Labbok, M., & Krasovec, K. (1990). Toward consistency in breastfeeding definitions. Studies in Family Planning, 21, 226–230.
Labbok, M. H., & Coffin, C. J. (1997). A call for consistency in definition of breastfeeding behaviors. Social Science and Medicine, 44, 1931–1932.
Thulier, D., & Mercer, J. (2009). Variables associated with breastfeeding duration. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 38, 259–268.
Kaneko, A., Kaneita, Y., Yokoyama, E., et al. (2006). Factors associated with exclusive breast-feeding in Japan: For activities to support child-rearing with breast-feeding. Journal of Epidemiology, 16, 57–63.
Dennis, C. L., & McQueen, K. (2009). The relationship between infant-feeding outcomes and postpartum depression: A qualitative systematic review. Pediatrics, 123, e736–e751.
de la Mora, A., Russell, D. W., Dungy, C. I., et al. (1999). The Iowa Infant Feeding Attitude Scale: Analysis of Reliability and Validity. Journal of Applied Social of Psychology, 29, 2362–2380.
Smilkstein, G., Ashworth, C., & Montano, D. (1982). Validity and reliability of the family APGAR as a test of family function. Journal of Family Practice, 15, 303–311.
Nagamine, T., Wada, Y., Ishikawa Y., & Maezawa, M. (1988). The explanatory model among patients with asthma. Gekkann Chiiki Iryo, 7, 126–133 (in Japanese).
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150, 782–786.
Okano, T., Murata, M., & Masuji, F. (1996). Validation and reliability of a Japanese version of the EPDS. Archives of Psychiatric Diagnostics and Clinical Evaluation, 7, 525–533.
Acknowledgments
This study was funded by the St. Luke’s Life Science Institute. The authors are most grateful to the women who participated in the survey at a particularly busy time in their lives, and to the staff members of the hospitals who distributed and collected the questionnaires. We also thank the following researchers who contributed to the development of the research protocol and analytic strategy: Colin Binns, Andy Lee, Toshinori Kitamura, Krishna Poudel, Junko Yasuoka, and Akira Shibanuma. Finally, we acknowledge the contribution of the following researchers in the conduct of the survey: Xiu-Fang Wang, Sumiyo Okawa, Yuko Matsuoka, and Kayoko Yoshikawa.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this license, visit (http://creativecommons.org/licenses/by-nc-nd/2.0/)
About this article
Cite this article
Otsuka, K., Taguri, M., Dennis, CL. et al. Effectiveness of a Breastfeeding Self-efficacy Intervention: Do Hospital Practices Make a Difference?. Matern Child Health J 18, 296–306 (2014). https://doi.org/10.1007/s10995-013-1265-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-013-1265-2