Abstract
Obesity is considered to be the leading metabolic disease in the world. The coincidence of postoperative complications is higher in obese individuals; thus, laparoscopic techniques due to their minimally invasive character became a standard in the surgical treatment of obesity. The proper function of peritoneal tissue is essential for the response to surgical trauma. Therefore, understanding the alterations of peritoneal tissue of obese individuals might explain the increased number of postoperative complications observed in obese patients. The study aimed to assess whether the stability of peritoneum is altered in obese patients and whether it corresponds to early postoperative complications in obese patients. Samples of parietal peritoneal tissue were collected at the beginning of the laparoscopic cholecystectomy from 80 patients. Differential scanning calorimetry was performed on samples defrosted at room temperature. Patients were divided into three groups according to the BMI value. For statistical analysis, ANOVA, Chi-square, Student’s t test, and correlations with Pearson test were used. Significantly lower ΔH and higher Tm were in patients in whom intraperitoneal adhesions were reported. Lower ΔH was reported in samples obtained from patients with temperature above 37 °C in the first 24 h postoperatively. Enthalpy of thermal transition (ΔH) in peritoneum obtained from parous was significantly lower in comparison with the samples from nullipara. It can be concluded that DSC parameters correlated with parameters related to the early postoperative period. Occurrence of adhesions was reported more frequently in the group of obese and overweight individuals and correlated with lower change in enthalpy of collagen denaturation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is considered to be the most prominent metabolic disease in the world. Because the occurrence of postoperative complications is significantly higher in obese individuals, laparoscopic surgical techniques have become a standard in the surgical treatment of obesity due to their minimally invasive nature. Additionally, adequately functioning peritoneal tissue is essential for the proper response to surgical trauma. It is possible that an understanding of alterations of peritoneal tissue in obese individuals may explain the increased number of postoperative complications observed in obese patients [1–3].
The peritoneal basal network is primarily formed by collagen. The overall status of the collagen structure and its interactions with the surrounding molecules are necessary for the physiological physical status of the tissue and the response to surgery.
Differential scanning calorimetry (DSC), an experimental thermoanalytical technique, has been used to examine the integrity of collagen-based structures [4–7]. The DSC method has proven to be a valuable tool in assessing the role of collagen in structural alterations of several cardiovascular and musculoskeletal diseases [8–11]. Our previous study showed that DSC was the appropriate method for investigation of subtle changes in physicochemical conditions of peritoneum using tissues obtained during surgical procedures [12].
Aim
The study aimed to assess the presence of alteration in the stability of peritoneum in obese patients and its subsequent correlation with early postoperative complications in obese patients.
Materials and methods
Eighty patients operated on due to cholelithiasis at the General and Oncological Surgery Department of the District Specialist Hospital in Lublin, Poland, were enrolled in this study. Patients were informed about the aim of the study and signed written consent forms prior to the study. The Ethical Committee of the Medical University of Lublin in Poland approved the study (decision no KE-0254/240/2008).
Cholelithiasis was confirmed by ultrasound examination in every patient. Patients with symptoms of inflammation (clinical or biochemical) were excluded from the study. Exclusion criteria also included acute cholecystitis due to gallbladder stones, diabetes, connective tissue disorders, and previous surgical interventions. The presence of varicose veins, cigarette smoking, and parity was recorded.
All patients underwent scheduled laparoscopic cholecystectomy performed in a standard four-trocar technique, using standard values (12–14 mmHg) of carbon dioxide pneumoperitoneum. The same team of surgeons operated on all the patients. Samples of peritoneal tissue from the parietal peritoneum (about 2.5 cm2) were collected at the beginning of surgery. The presence of intraperitoneal adhesions was reported during the surgery and classified according to Coccolini et al. [13]. No complications were reported during the surgeries, and no malignancies were reported in the pathological examination of the removed gallbladders.
During the early postoperative period, body temperature was taken and the intensity of postoperative pain was measured by visual analogue scale (VAS). On the third day after the surgery, analgesic administration during the first 24 postoperative hours, occurrence of postoperative nausea and vomiting (PONV), and WBC levels were assessed.
The samples of peritoneum collected during surgery were immersed in 0.9% NaCl and frozen to −16 °C. Differential scanning calorimetry (Q200 calorimeter, TA Instruments) was performed on samples defrosted at room temperature. Hermetic aluminum pans with 5–7 mg of peritoneal tissue were filled with 10–20 μl of saline and scanned from 40 to 85 °C at heating rate 5 °C min−1. A pan filled with 0.9% NaCl was used as a reference. From curves recorded during measurement, the initial temperature of transition (the onset temperature, Ton) that could indicate the temperature of protein denaturation, the peak temperature of transition (Tm) corresponding to the temperature of protein denaturation, and the energy absorbed by the sample during transition were determined using software integrated with the calorimeter. Change in enthalpy (ΔH) during the process was expressed as energy of transition for one gram of dry mass from the sample. The dry mass from the sample was measured following the calorimetry and the 24-hour drying period. This was done at room temperature in an exsicator.
Patients were divided into three groups according to BMI (body mass index) values: Group N (normal weight patients, BMI values less or equal 25 kg m−2) consisted of 18 patients (male/female M:F = 1:17). Group H (overweight patients, BMI values between 25 and 30 kg m−2) consisted of 27 patients (M:F = 7:20), and group O (obese patients, with BMI values equal or above 30 kg m−2) consisted of 35 patients (M:F = 6:29).
Differences between the study groups were accessed using the ANOVA test with Tuckey’s post hoc analysis, Student’s t test, Chi-square test, and correlations with Pearson test. The results were presented as mean ± standard deviation (SD) and percentages. Data were analyzed using SPSS Statistics version 16 software, with p value of less than of 0.05 considered to be significant.
Results
The patients’ mean demographic and clinical data are presented in Table 1. Statistically significant differences were observed regarding BMI values. Before the surgery, each patient was assessed according to the ASA scale with no significant differences between groups.
The calorimetric parameters of the peritoneum in the three studied groups are presented in Table 2. No significant differences of DSC parameters were observed between the studied groups. Additionally, calorimetric parameters were analyzed in terms of correlation with gender and BMI values, but no significant results were found.
In total, 11.4% of patients reported cigarette smoking. Statistical analysis of the calorimetric parameters did not show any significant differences between smoking and non-smoking patients. The mean length of smoking was 27 ± 8.72 years, and the mean number of cigarettes smoked daily was 17.4 ± 10.19.
Additionally, the calorimetric parameters were compared between parous and nulliparous patients. Enthalpy of thermal transition (ΔH) in the samples of peritoneum obtained from parous was significantly (p = 0.004) lower in comparison with the samples from nullipara (18.57 ± 6.26 vs. 29.95 ± 11.30 J g−1). No significant differences were observed when calorimetric parameters of the peritoneum were compared between pre- and postmenopausal patients in respective BMI groups and when only postmenopausal patients were analyzed in regard to BMI group.
Varicose veins were reported in 20% of the total population. No influence of this clinical feature and calorimetric parameter was observed.
The evaluation of adhesions revealed a presence of intraperitoneal adhesions in 39% (n = 31) of the studied population. Statistical analysis of calorimetric parameters showed significantly (p = 0.035) lower changes in enthalpy (ΔH) in patients in whom intraperitoneal adhesions were reported during surgery in comparison with those without adhesions (16.56 ± 5.32 vs. 20.02 ± 7.27 J g−1). The results are presented in Fig. 1. The temperature of thermal transition (Tm) was higher in patients with intraperitoneal adhesions than in patients without them; however, there were no significant differences (68.25 ± 0.93 vs. 67.81 ± 1.12 °C).
Considering BMI values, intraperitoneal adhesions were present in 28% (n = 5) of patients in group N, and 37% (n = 10) in group H and 46% (n = 16) in group O. According to the Peritoneal Adhesion Index (PAI), filmy adhesions (grade score 1) were observed in group N while strong adhesions (grade score 2) were reported in group H and O. Within the BMI groups, there were no significant differences in calorimetric parameters between patients with or without adhesions. Among the patients with adhesions, no differences of studied DSC parameters were observed.
33.8% of patients had body temperature above 37 °C in the first 24 h postoperatively. Results of DSC analysis showed that enthalpy of thermal transition (ΔH) in samples of peritoneum obtained from these patients was significantly (p = 0.029) lower (16.15 ± 5.25 vs. 20.04 ± 7.28 J g−1) than in samples from patients with normal body temperature. Results are presented in Fig. 2.
Temperature above 37 °C was observed more often in patients from group O (42.9%) than in patients in group N (20%) and H (30.4%); however, the differences were not significant (χ 2).
DSC data obtained from the three BMI groups were analyzed separately (Fig. 3). A significantly higher (p = 0.009) temperature of thermal transition (Tm) of peritoneum was observed in tissue collected from patients in group H with elevated postoperative temperature in comparison with those with normal body temperature (68.83 ± 0.65 vs. 67.78 ± 0.79 °C). In group N and O, no significant differences were observed.
Intensity of the postoperative pain was assessed in the 24th postoperative hour using the visual analogue scale (VAS), in which 0 indicates no pain, and 10 indicates the most severe pain. No significant differences were observed between BMI groups. The highest values (5.10 ± 0.74 cm) of postoperative pain were reported in the normal weight group, while the lowest pain was reported in the obese patients (3.90 ± 1.91 cm). In group H, it was 4.56 ± 1.234 cm. There was a significant correlation between patient BMI values and the value of postoperative pain, which indicates the decrease in pain together with an increase in BMI values (p = 0.035; r = −0.363). There was no significant correlation between postoperative pain and calorimetric parameters. In total, 47.5% of patients reported higher (more than 5 cm on VAS) postoperative pain in the first 24 h after surgery. There were no significant differences in calorimetric parameters between patients reporting postoperative pain in comparison with patients who did not. Postoperative pain was reported with the frequency of 58.8, 38.9, and 46.9% in group N, H, and O, respectively. No differences between the groups were observed. Within the BMI groups, calorimetric parameters did not differ significantly between patients who experienced and who did not experience postoperative pain. There were also no statistically significant differences in calorimetric parameters between BMI groups when only patients reporting postoperative pain were analyzed.
Analgesics were administered to more than 90% of patients in all three studied groups, and the mean analgesics amount was approximately the same. There was a significant correlation between the BMI values and the amount of analgesics in group O, indicating a corresponding increase in analgesics amount alongside increased patient BMI values (p = 0.029; r = 0.386). However, the correlation between BMI values and the amount of analgesics in the total population was insignificant.
There were no statistically significant correlations between calorimetric parameters and amount of administered analgesics in any group.
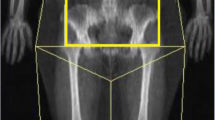
WBC levels were also analyzed on the day before hospital discharge. It was observed that the WBC levels differed (p = 0.008, ANOVA) between BMI groups (Fig. 4). It was significantly (p = 0.007) higher in group O (7.33 ± 2.26 × 103 μL−1) in comparison with group N (5.62 ± 0.95 × 103 μL−1). In group H, the mean WBC level was 6.42 ± 1.07 × 103 μL−1.
On the day of discharge, WBC levels correlated significantly (p < 0.001; r = 0.45) with patient BMI, indicating that the WBC levels increased along with the increase in BMI values. There were no significant correlations between WBC levels and calorimetric parameters in the study groups.
We did not observe any significant differences between wound healing and DSC parameters. Wound healing was assessed twice, during the first 24 postoperative hours and on the day of hospital discharge. There was only one case in group H in which the wound margins revealed symptoms of wound contamination. In all other cases, the process of wound healing was physiological. On the 4th day of hospitalization, there were 2 cases (11%) in group N and 5 (14%) in group O where improper wound healing was reported. At both time periods, no significant differences were observed between groups in the wound healing process. There were no significant differences between calorimetric parameters and the type of wound healing processes in the total population or in each group separately.
Discussion
The metabolic activity of adipose tissue includes the secretion of proinflammatory cytokines that include, e.g., IL-6 and TNF-α. This process, described as metaflammation, can influence the course of the postoperative period by impairing the inflammatory response to surgical trauma [14–16]. In addition, obese patients undergoing laparoscopic procedures may develop postoperative complications more often due to the parallel release of inflammatory and angiogenic cytokines from peritoneal and adipose tissue. Liu and Hou described changes in peritoneal tissue 30 min after the beginning of the surgery [17]. In our previous study, we did not reveal any changes between samples collected at the beginning and end of the pneumoperitoneum with a mean duration of 42 min. However, the prevalence of enthalpy of collagen denaturation in samples collected at the end of surgery tends to decrease with increased pneumoperitoneum duration [18].
The mechanism of activation of the inflammatory reaction within the peritoneal tissue in obese individuals undergoing laparoscopic surgery remains unclear. Thus, an attempt to evaluate the peritoneal tissue obtained from the obese patients undergoing laparoscopic cholecystectomy was performed in this study using the DSC method.
Heat-induced denaturation of proteins is well understood; however, the heat denaturation of structural proteins within whole tissues remains an area of active research. DSC was described as a sensitive method for evaluation of collagen structure [5, 6, 19, 20]. The stability of peritoneal tissue can influence the activation of inflammatory and angiogenic reactions due to surgical stress. In our study, samples of peritoneal tissue were obtained during the surgery. DSC results showed an irreversible endothermic process starting above 60 °C with the peak temperature of thermal transition ranging from 65 to 70 °C. Such thermal activity can be attributed to denaturation of collagen, which is the main structural protein of peritoneal tissue. The process of thermal activation of collagen involves the rupture of hydrogen bonds coupling the three α-chains and a rearrangement of the triple helix into a random chain configuration [4, 5, 21]. In our samples, the denaturation endotherm was followed by an equilibrium state adequate to the new configuration of the protein molecules at temperatures just above 70 °C. Similar values of denaturation temperatures are reported for samples from other collagen-based tissues [8, 10, 22, 23]. Thermal stability of collagen molecules reflects the overall condition of the structure, cross-links in the collagen network, and its interactions with the surrounding molecules [4, 21, 24–26]. Parameters of thermal transition of collagen in tissues were shown to be sensitive to the number of cross-links as well as to the level of hydration of collagen molecules [21–24, 27, 28]. However, differences in enthalpy of transition for tissue samples may also reflect different amounts of collagen molecules in relation to other, non-collagenous components of the sample.
Obese individuals have increased intra-abdominal pressure, which can influence the condition of the peritoneal tissue. The evaluation of calorimetric parameters did not reveal differences between groups, but a trend toward increasing denaturation temperature and lower enthalpy of denaturation with increasing BMI was observed. Decreased enthalpy of the denaturation process accompanied by rising denaturation temperature was reported to result from gradual dehydration of collagen [27, 28]. In obese individuals, the increased intra-abdominal pressure might alter the flow of lymph and blood of venous and arterial vessels located in the basal lamina of the peritoneal tissue. This phenomenon can lead to postoperative complications including prolonged wound healing and a higher occurrence of adhesions [22, 24]. As DSC results have been proven to be very sensitive to the level of collagen hydration, we plan to evaluate more samples of peritoneal tissue from obese patients that might reveal these differences.
In our study, a significantly lower change in enthalpy (ΔH) of collagen denaturation was found in samples from patients in whom intraperitoneal adhesions were reported during surgery in comparison with those without adhesions. Intraperitoneal adhesions constitute a common complication after abdominal surgeries [29, 30]. Carbon dioxide pneumoperitoneum affects the intraperitoneal environment and was described as a factor, which in standard conditions during short time laparoscopy, influences the peritoneum and promotes the formation of adhesions. However, heating the gas may limit this process [31–34]. Molinas et al. [35] studied mice peritoneum and observed that an increased formation of adhesions correlates with the duration and pressure of pneumoperitoneum. Additionally, abdominal adhesions were reported more often in obese individuals. These phenomena might suggest alterations in the peritoneal tissue of obese individuals, which can be caused by the metabolic activity of fat tissue as well as increased intra-abdominal pressure. In our study, a higher number of intraperitoneal adhesions were observed in obese patients and are similar to the results of the Weibel and Majno study who examined cadavers and concluded that adhesions are more frequent in females and that the incidence increases with higher body mass [36].
Alterations of the collagen structure found in peritoneum might be connected with other deficits of the connective tissue in different regions of the body and the higher occurrence of hernias and varicose veins [37–39]. Additionally, obesity is a well-known factor influencing venous blood flow from lower limbs and increases the risk of varicose veins, especially in women [40–44]. In our study, varicose veins were observed more frequently in obese patients. However, our study did not reveal any relation between calorimetric parameters and the occurrence of varicose veins.
Differences in the occurrence of increased body temperature and improper wound healing were not observed in the compared groups within early postoperative period. In our study, obese patients were characterized by higher WBC count in comparison with normal and overweighed individuals. Additionally, increase in WBC count at the day of hospital discharge accompanied the increase in patients’ BMI value. Our observations correlate with the epidemiological studies indicating the increase in WBC count in individuals with higher fat storage what probably is the result of obesity-driven inflammation [45, 46].
Obese individuals are more likely to experience pain in comparison with normal-weighted counterparts [47, 48]. However, results of our study showed no significant differences in postoperative pain value between BMI groups. On the other hand, significant positive correlation was found between the BMI values and the amount of analgesics in obese patients. It may suggest a complex and multidirectional mechanism of postoperative pain development. In our previous study, significantly lower onset temperatures (To) and denaturation temperatures (Tm) were observed in the peritoneal samples obtained from patients who underwent plastic repair of inguinal hernias, in comparison with samples from patients who underwent laparoscopic cholecystectomy or who were operated on due to rectal cancer [12]. Such results may suggest a lower physical stability of collagen molecules, which has an impact on the occurrence of hernias. Thus, the coexistence of excessive adipose tissue and collagen structure changes may result in a lower pain threshold and a subsequent increase in the postoperative analgesics intake [37, 38].
In our study, no differences between original BMI groups and studied calorimetric parameters were reported. Therefore, we decided to extend our analysis to other parameters that might suggest changes in the status of collagen within the peritoneum. The structure of connective tissue in pregnancy might be altered [49–51]. Collagen fiber disruption and a decrease in collagen cross-linking may be associated with softening of the uterine cervix [52–54]. Higher hydration and collagen extractability was reported by other authors in parous women [53, 54]. Moreover, increased collagen extractability was reported to be associated with cervical insufficiency. A weaker collagen network was described in correlation with increased parity [53, 55]. Pinherio et al. studied the architecture of collagen fibers in the pubic symphysis and ligaments in pregnant mice and observed a disrupted helical arrangement of the collagen fibers, which can explain the remodeling of these structures at the end of pregnancy [56]. Collagen type I and III is a structural component of articular ligaments [57, 58]. The laxity of ligaments was described to be altered in parous women [59]. Relaxin, estrogen, and progesterone, which have receptors on ligaments and which have increased levels during pregnancy, may influence the status of connective tissue [60, 61].
In our study, an interesting part of the enthalpy of collagen thermal transition finding was reported. In samples obtained from parous patients, the thermal transition of collagen was lower in comparison with the samples from nulliparous patients. This finding requires future study and might be correlated with changes in collagen tissue after pregnancy reported by other authors, but not in peritoneal tissue [49–61].
Conclusions
The DSC parameters evaluated in our study correlated with parameters related to the early postoperative period. However, we did not observe differences between the evaluated DSC parameters and BMI values, gender, or age. The occurrence of adhesions was reported more frequently in the group of obese and overweight individuals and correlated with a lower change in enthalpy of collagen denaturation that might suggest weaker binding properties of proteins in peritoneal tissue. This phenomenon can influence the process of wound healing.
Despite the fact that the presented study has limited direct clinical implication, it can explain the postoperative pathophysiology of the peritoneal tissue and influence of excessive adipose tissue that may have a direct influence on the early postoperative period and occurrence of postoperative pain. The authors intend to experiment on broader peritoneal tissue samples and other bioclinical parameters.
References
Formiguera X, Cantón A. Obesity: epidemiology and clinical aspects. Best Pract Res Clin Gastroenterol. 2004;2004(18):1125–46.
Gutt CN, Oniu T, Schemmer P, et al. Fewer adhesions induced by laparoscopic surgery? Surg Endosc. 2004;18:898–906.
van Goor H. Consequences and complications of peritoneal adhesions. Colorectal Dis. 2007;9(S2):25–34.
Bischof JC, He X. Thermal stability of proteins. Ann NY Acad Sci. 2005;1066:12–33.
Bruylants G, Wouters J, Michaux C. Differential scanning calorimetry in life science: thermodynamics, stability, molecular recognition and application in drug design. Curr Med Chem. 2005;12:2011–20.
Wen J, Arthur K, Chemmalil L, et al. Applications of differential scanning calorimetry for thermal stability analysis of proteins: qualification of DSC. J Pharm Sci. 2012;101:955–64.
Onem E, Yorgancioglu A, Karavana HA, et al. Comparison of different tanning agents on the stabilization of collagen via differential scanning calorimetry. J Therm Anal Calorim. 2017.
Hadian M, Corcoran BM, Bradshaw JP. Molecular changes in fibrillar collagen in myxomatous mitral valve disease. Cardiovasc Pathol. 2010;19:141–8.
Samouillan V, Dandurand-Lods J, Lamure A, et al. Thermal analysis characterization of aortic tissues for cardiac valve bioprostheses. J Biomed Mater Res. 1999;46:531–8.
Samouillan V, Dandurand J, Lacabanne C, et al. Characterization of aneurysmal aortas by biochemical, thermal, and dielectric techniques. J Biomed Mater Res A. 2010;95:611–9.
Wiegand N, Vámhidy L, Lőrinczy D. Differential scanning calorimetric examination of ruptured lower limb tendons in human. J Therm Anal Calorim. 2010;101:487–92.
Torres K, Trębacz H, Chrościcki A, et al. Evaluation of peritoneal tissue by means of differential scanning calorimetry (DSC). Folia Histochem Cytobiol. 2011;49:700–5.
Coccolini F, Ansaloni L, Manfredi R, et al. Peritoneal adhesion index (PAI): proposal of a score for the “ignored iceberg” of medicine and surgery. World J Emerg Surg. 2013;31(8):6.
Ferroni P, Basili S, Falco A, et al. Inflammation, insulin resistance, and obesity. Curr Atheroscler Rep. 2004;6:424–31.
Wisse BE. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J Am Soc Nephrol. 2004;15:2792–800.
Womack J, Tien PC, Feldman J, et al. Obesity and immune cell counts in women. Metabolism. 2007;56:998–1004.
Liu Y, Hou QX. Effect of carbon dioxide pneumoperitoneum during laparoscopic surgery on morphology of peritoneum. Zhonghua Yi Xue Za Zhi. 2006;86:164–6.
Torres K, Trębacz H, Bącik-Donica M, et al. Does thermodynamic stability of peritoneal collagen change during laparoscopic cholecystectomies? A differential scanning calorimetry (DSC) study. Surg Endosc. 2014;28:2623–6.
Sillinger T, Lőrinczy D, Kocsis B, et al. Differential scanning calorimetric measurement of cartilage destruction caused by Gram-negative septic arthritis. J Therm Anal Calorim. 2014;116:747–52.
Nőt LG, Naumov I, Vámhidy L, Lőrinczy D, Wiegand N. Comparison of thermal characteristics of degenerated and inflamed human collagen structures with differential scanning calorimetry. J Thermal Anal Calorim. 2013;113:273–9.
Bailey AJ. Molecular mechanisms of ageing in connective tissues. Mech Ageing. 2001;122:735–55.
Miles CA. Kinetics of collagen denaturation in mammalian lens capsules studied by differential scanning calorimetry. Int J Biol Macromol. 1993;15:265–71.
Skrzyński S, Sionkowska A, Marciniak A. DSC study of collagen in disc disease. J Biophys 2009;2009:819635.
Knott L, Whitehead CC, Fleming RH, et al. Biochemical changes in the collagenous matrix of osteoporotic avian bone. Biochem J. 1995;310:1045–51.
Pietrucha K. Changes in denaturation and rheological properties of collagen-hyaluronic acid scaffolds as a result of temperature dependencies. Int J Biol Macromol. 2005;36:299–304.
Sohár G, Aigner Z, Gálity H, et al. Calorimetric investigation of normal and pathological human meniscus. J Therm Anal Calorim. 2014;115:2031–5.
Miles CA, Ghelashvili M. Polymer-in-a-box mechanism for the thermal stabilization of collagen molecules in fibres. Biophys J. 1999;76:3243–52.
Trębacz H, Wójtowicz K. Thermal stabilization of collagen molecules in bone tissue. Int J Biol Macromol. 2005;37:257–62.
Boland GM, Weigel RJ. Review formation and prevention of postoperative abdominal adhesions. J Surg Res. 2006;132:3–12.
Jacobi CA, Sterzel A, Braumann C, et al. The impact of conventional and laparoscopic colon resection (CO2 or helium) on intraperitoneal adhesion formation in a rat peritonitis model. Surg Endosc. 2001;15:380–6.
Arung W, Meurisse M, Detry O. Pathophysiology and prevention of postoperative peritoneal adhesions. World J Gastroenterol. 2011;17:4545–53.
Ordoñez JL, Domínguez J, Evrard V, et al. The effect of training and duration of surgery on adhesion formation in the rabbit model. Hum Reprod. 1997;12:2654–7.
Peng Y, Zheng M, Ye Q, et al. Heated and humidified CO2 prevents hypothermia, peritoneal injury, and intra-abdominal adhesions during prolonged laparoscopic insufflations. J Surg Res. 2009;151:40–7.
Rout UK, Diamond MP. Role of plasminogen activators during healing after uterine serosal lesioning in the rat. Fertil Steril. 2003;79:138–45.
Molinas CR, Mynbaev O, Pauwels A, et al. Peritoneal mesothelial hypoxia during pneumoperitoneum is a cofactor in adhesion formation in a laparoscopic mouse model. Fertil Steril. 2001;76:560–7.
Weibel MA, Majno G. Peritoneal adhesions and their relation to abdominal surgery: a postmortem study. Am J Surg. 1973;126:345–53.
Haviarová Z, Weismann P, Stvrtinová V, et al. The determination of the collagen and elastin amount in the human varicose vein by the computer morphometric method. Gen Physiol Biophys. 1999;1:30–3.
Haviarova Z, Janega P, Durdik S, et al. Comparison of collagen subtype I and III presence in varicose and non-varicose vein walls. Bratisl Lek Listy. 2008;109:102–5.
Wali MA, Eid RA. Changes of elastic and collagen fibers in varicose veins. Int Angiol. 2002;21:337–43.
Brand FN, Dannenberg AL, Abbott RD, et al. The epidemiology of varicose veins: the Framingham Study. Am J Prev Med. 1988;4:96–101.
Iannuzzi A, Panico S, Ciardullo AV, et al. Varicose veins of the lower limbs and venous capacitance in postmenopausal women: relationship with obesity. J Vasc Surg. 2002;36:965–8.
Jawien A, Grzela T, Ochwat A. Prevalence of chronic venous insufficiency in men and women in Poland: multicenter cross-sectional study in 40095 patients. Phlebology. 2003;18:110–2.
Karathanos Ch, Sfyroeras G, Drakou A, et al. Superficial vein thrombosis in patients with varicose veins: role of thrombophilia factors, age and body mass. Eur J Vasc Endovasc Surg. 2012;43:355–8.
Musil D, Kaletova M, Herman J. Age, body mass index and severity of primary chronic venous disease. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2011;155:367–71.
Farhangi MA, Keshavarz SA, Eshraghian M, et al. White blood cell count in women: relation to inflammatory biomarkers, haematological profiles, visceral adiposity, and other cardiovascular risk factors. J Health Popul Nutr. 2013;31:58–64.
Holz T, Thorand B, Doring A, et al. Markers of inflammation and weight change in middle-aged adults: results from the prospective MONICA/KORA S3/F3 study. Obesity. 2010;18:2347–53.
McCarthy LH, Bigal ME, Katz M, et al. Chronic pain and obesity in elderly people: results from the Einstein aging study. J Am Geriatr Soc. 2009;57:115–9.
Mogil JS, Bailey AL. Sex and gender differences in pain and analgesia. Prog Brain Res. 2010;186:141–57.
Iwahashi M, Muragaki Y, Ooshima A, Umesaki N. Decreased type I collagen expression in human uterine cervix during pregnancy. J Clin Endocrinol Metab. 2003;88:2231–5.
Myers K, Socrate S, Tzeranis D, et al. Changes in the biochemical constituents and morphologic appearance of the human cervical stroma during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2009;144(Suppl1):82–9.
Samuel CS, Coghlan JP, Bateman JF. Effects of relaxin, pregnancy and parturition on collagen metabolism in the rat pubic symphysis. J Endocrinol. 1998;159:117–25.
Danforth DN. The morphology of the human cervix. Clin Obstet Gynecol. 1983;26:7–13.
Petersen LK, Uldbjerg N. Cervical collagen in non-pregnant women with previous cervical incompetence. Eur J Obstet Gynecol Reprod Biol. 1996;67:41–5.
Rechenberger T, Uldbjerg N, Oxlund H. Connective tissue changes in the cervix during normal pregnancy and pregnancy complicated by cervical incompetence. Obstet Gynecol. 1988;71:563–7.
Danforth DN, Veis A, Breen M, et al. The effect of pregnancy and labor on the human cervix: changes in collagen, glycoproteins, and glycosaminoglycans. Am J Obstet Gynecol. 1974;120:641–51.
Pinheiro MC, Moraes SG, Battlehner CN, et al. Histochemical and ultrastructural study of collagen fibers in mouse pubic symphysis during late pregnancy. Micron. 2004;35:685–93.
Buckwalter JA, Woo SL-Y, Goldberg VM, et al. Soft tissue aging and musculoskeletal function. J Bone Joint Surg. 1993;75A:1533–48.
Fu EH, Harner CD, Vince KG. Knee Surgery. Baltimore: Williams and Wilkins; 1994.
Schauberger CW, Rooney BL, Goldsmith L, et al. Peripheral joint laxity increases in pregnancy but does not correlate with serum relaxin levels. An J Obstet Gynecol. 1996;174:667–71.
Liu S, Al-shaikh R, Panossian V, et al. Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament. J Orthop Res. 1996;1996(14):526–33.
Sherwood OD. Relaxin. In: Knobil E, Neill JD, editors. The physiology of reproduction. New York: Raven Press; 1994. pp. 861–1009.
Funding
This work was supported by grant of Medical University of Lublin (Grant # DS205 to K.T.)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Torres, K., Trębacz, H., Pietrzyk, Ł. et al. Stability of peritoneal tissue evaluated by the means of DSC in obese patients undergoing laparoscopic cholecystectomy. J Therm Anal Calorim 130, 2191–2198 (2017). https://doi.org/10.1007/s10973-017-6496-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-017-6496-9