Abstract
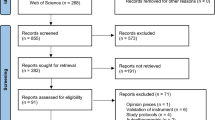
The availability of safe and effective non-pharmacological therapies for pain is an important unmet medical need. Prayer may be considered as an effective adjunctive therapy for pain and this systematic review aims to clarify this association. Pertinent databases were searched for English language publications, dated 2000–2019. Inclusion criteria involved prayer as an on-site or personal intervention and at least one pre-specified pain-related outcome. We evaluated 411 abstracts. Nine studies met criteria. Active prayer to God emerged as a preferred beneficial intervention for religious patients undergoing surgery or a painful procedure. Prayer effect does not seem to be opioid mediated. Improved trial design will facilitate the study of prayer as an adjuvant therapy for pain.

Similar content being viewed by others
References
Andersson, G. (2008). Chronic pain and praying to a higher power: Useful or useless? Journal of Religion and Health,47(2), 176–187.
Beiranvand, S., Noparast, M., Eslamizade, N., & Saeedikia, S. (2014). The effects of religion and spirituality on postoperative pain, hemodynamic functioning and anxiety after cesarean section. Acta Medica Iranica,52(12), 909–915.
Black, L. I., Clarke, T. C., Barnes, P. M., Stussman, B. J., & Nahin, R. L. (2015). Use of complementary health approaches among children aged 4–17 years in the United States: National Health Interview Survey, 2007–2012. National Health Statistics Reports,10(78), 1–19.
Clarke, T. C., Black, L. I., Stussman, B. J., Barnes, P. M., & Nahin, R. L. (2015). Trends in the use of complementary health approaches among adults: United States, 2002–2012. National Health Statistics Reports,10(79), 1–16.
Dahlhamer, J., Lucas, J., Zelaya, C., Nahin, R., Mackey, S., DeBar, L., et al. (2018). Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. Morbidity and Mortality Weekly Report,67(36), 1001–1006.
Dezutter, J., Wachholtz, A., & Corveleyn, J. (2011). Prayer and pain: The mediating role of positive re-appraisal. Journal of Behavioral Medicine,34(6), 542–549.
Eilami, O., Moslemirad, M., Naimi, E., Babuei, A., & Rezaei, K. (2019). The effect of religious psychotherapy emphasizing the importance of prayers on mental health and pain in cancer patients. Journal of Religion and Health,58(2), 444–451.
Elmholdt, E., Skewes, J., Dietz, M., Møller, A., Jensen, M. S., Roepstorff, A., et al. (2017). Reduced pain sensation and reduced BOLD signal in parietofrontal networks during religious prayer. Frontiers in Human Neuroscience,11, 337.
Hamman, A. G. (2015). Prayer. In Encyclopaedia Britannica. Retrieved October 23, 2019 from https://www.britannica.com/topic/prayer
Hassanpour-Dehkordi, A., Fatehi, D., & Solati, K. (2016). Analgesic plus prayer versus analgesic alone. Effect of prayer on intensity of postoperative pain, anxiety and physiological indices in surgical patients. A randomized clinical trial. Heroin Addiction and Related Clinical Problems,18(6), 13–20.
Jegindø, E. M. E., Vase, L., Skewes, J. C., Terkelsen, A. J., Hansen, J., Geertz, A. W., et al. (2013). Expectations contribute to reduced pain levels during prayer in highly religious participants. Journal of Behavioral Medicine,36(4), 413–426.
Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology,4, 863.
Masters, K. S., & Spielmans, G. I. (2007). Prayer and health: Review, meta-analysis, and research agenda. Journal of Behavioral Medicine,30(4), 329–338.
Meints, S. M., & Hirsh, A. T. (2015). In vivo praying and catastrophizing mediate the race differences in experimental pain sensitivity. The Journal of Pain,16(5), 491–497.
Meints, S. M., Mosher, C., Rand, K. L., Ashburn-Nardo, L., & Hirsh, A. T. (2018). An experimental investigation of the relationships among race, prayer, and pain. Scandinavian Journal of Pain,18(3), 545–553.
Merskey, H., Albe-Fessard, D. G., Bonica, J. J., Carmen, A., Dubner, R., Kerr, F. W. L., et al. (1979). IASP sub-committee on taxonomy. Pain,6(3), 249–252.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). The PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med.,6(6), e1000097.
Rahman, F. S., Yahya, N., Din, N. M. M., Izaham, A., & Mat, W. R. W. (2018). The comparative effects of listening to prayer recitation and music therapy intraoperatively on postoperative pain. International Medical Journal Malaysia,17(2), 107–115.
Robles, B., Upchurch, D. M., & Kuo, T. (2017). Comparing complementary and alternative medicine use with or without including prayer as a modality in a local and diverse United States jurisdiction. Frontiers in Public Health,5, 56.
Rosenstiel, A. K., & Keefe, F. J. (1983). The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain,17(1), 33–44.
Wachholtz, A. B., Pearce, M. J., & Koenig, H. (2007). Exploring the relationship between spirituality, coping, and pain. Journal of Behavioral Medicine,30(4), 311–318.
Wilson, D. (2001). Effect Size Calculator. Retrieved November 28, 2019 from http://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-Home.php
Acknowledgements
This paper was written in fulfillment of the Capstone requirement for the degree of Master of Science in Pain Research, Education and Policy (PREP) at Tufts University School of Medicine Public Health and Professional Degree Programs, Boston, MA. The authors wish to thank Dr. Ylisabyth (Libby) Bradshaw, DO, MS, Academic Advisor and Dr. Daniel Carr, Program Director at Tufts University School of Medicine PREP Program for their support of this project. Special thanks to Ms. Amy Lapidow, Librarian at the Hirsh Medical Library, Tufts University School of Medicine, for technical assistance, and Dr. Samantha Meints, Post-doctoral Fellow, Brigham and Women’s Hospital, Boston, MA for research consulting.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Illueca, M., Doolittle, B.R. The Use of Prayer in the Management of Pain: A Systematic Review. J Relig Health 59, 681–699 (2020). https://doi.org/10.1007/s10943-019-00967-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-019-00967-8