Abstract
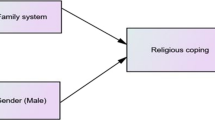
Coping has emerged as a vital indicator among patients in the chronic conditions. The current study examined the role of demographic characteristics (such as age, education, gender, marital status, residential background, family type and number of children) in adoption of coping (emotion-focused, problem-solving, religious–spiritual) strategies for nursing among hepatitis patients. A sample of 500 patients (of hepatitis C) was drawn from five most populous districts (Lahore, Faisalabad, Rawalpindi, Gujranwala and Multan) of Punjab, Pakistan, by using Epi Info software with an alpha level of 0.03. The data were collected using a well-structured multi-sectional interview schedule through multistage proportionate sampling technique. Descriptive analysis, regression analysis and reliability analysis were computed using SPSS (version 21.0). In the overall adoption of coping strategies, lower monthly household income, lower education, rural residences, nuclear family setting and married status were contributing to the adoption of higher coping strategies among Muslim chronic patients with hepatitis C. The results of socio-demographics are also discussed with other coping strategies (such as religious–spiritual coping strategies, problem-solving coping strategies, emotion-focused coping strategies and constructive coping strategies). It was the first quantitative study of adoption of coping strategies among Muslim hepatitis patients in Pakistan. The study highlighted the importance of socio-demographic resources to cope with chronic illness. The empirical findings would start a new discussion from hepatic, counseling and nursing perspective. For terminal patients, these socio-demographic characteristics can serve as a guideline to provide community sources of social support. Medical social workers and healthcare experts need to facilitate the efforts of patients to cope with chronic illness through revision of nursing policy according to the socio-demographic and spiritual–religious needs of the patients.
Similar content being viewed by others
References
Adler, N. E., & Ostrove, J. M. (1999). Socioeconomic status and health: What we know and what we don’t. Annals of the New York Academy of Sciences,896(1), 3–15.
Ano, G. G., & Vasconcelles, E. B. (2005). Religious coping and psychological adjustment to stress: A meta-analysis. Journal of Clinical Psychology,61(4), 461–480.
Bentur, N., Stark, D. Y., Resnizky, S., & Symon, Z. (2014). Coping strategies for existencial and spiritual suffering in Israeli patients with advanced cancer. Israel Journal of Health Policy Research,3(1), 21. https://doi.org/10.1186/2045-4015-3-21.
Bonneville-Roussy, A., Evans, P., Verner-Filion, J., Vallerand, R. J., & Bouffard, T. (2017). Motivation and coping with the stress of assessment: Gender differences in outcomes for university students. Contemporary Educational Psychology,48, 28–42.
Brannon, L., Feist, J., & Updegraff, J. A. (2013). Health psychology: An introduction to behavior and health. Boston: Cengage Learning.
Büssing, A., Ostermann, T., Neugebauer, E. A., & Heusser, P. (2010). Adaptive coping strategies in patients with chronic pain conditions and their interpretation of disease. BMC Public Health,10(1), 507.
Cameron, L. D., & Wally, C. M. (2015). Chronic illness, psychosocial coping with. International Encyclopedia of the Social & Behavioral Sciences,2(3), 549–554.
Caplan, L. J., & Schooler, C. (2007). Socioeconomic status and financial coping strategies: The mediating role of perceived control. Social Psychology Quarterly,70(1), 43–58.
Carroll, L. (2013). Problem-focused coping. In M. D. Gellman & J. R. Turner (Eds.), Encyclopedia of behavioral medicine (pp. 1540–1541). Springer: New York.
Carver, C. S., & Scheier, M. F. (1981). The self-attention-induced feedback loop and social facilitation. Journal of Experimental Social Psychology,17(6), 545–568.
Carver, C. S., & Vargas, S. (2011). Stress, coping, and health. In H. S. Friedman (Ed.), The Oxford handbook of health psychology (pp. 192–198). New York, NY: Oxford University Press.
Chang, S. C., Ko, W. S., Wu, S. S., Peng, C. Y., & Yang, S. S. (2008). Factors associated with quality of life in chronic hepatitis C patients who received interferon plus ribavirin therapy. Journal of the Formosan Medical Association,107(6), 454–462.
Christensen, U., Schmidt, L., Hougaard, C. O., Kriegbaum, M., & Holstein, B. E. (2006). Socioeconomic position and variations in coping strategies in musculoskeletal pain: A cross-sectional study of 1287 40-and 50-year-old men and women. Journal of Rehabilitation Medicine,38(5), 316–321.
Cockerham, W. C. (2005). Health lifestyle theory and the convergence of agency and structure. Journal of Health and Social Behavior,46(1), 51–67.
Connor-Smith, J. K., Compas, B. E., Wadsworth, M. E., Thomsen, A. H., & Saltzman, H. (2000). Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology,68(6), 976.
Constant, A., Castera, L., de Ledinghen, V., Couzigou, P., & Bruchon-Schweitzer, M. (2005). Psychosocial factors associated with perceived disease severity in patients with chronic hepatitis C: Relationship with information sources and attentional coping styles. Psychosomatics,46(1), 25–33.
Cromwell, K. D., Chiang, Y. J., Armer, J., Heppner, P. P., Mungovan, K., Ross, M. I., et al. (2015). Is surviving enough? Coping and impact on activities of daily living among melanoma patients with lymphoedema. European Journal of Cancer Care,24(5), 724–733.
Cutler, D. M., & Lleras-Muney, A. (2010). Understanding differences in health behaviors by education. Journal of Health Economics,29(1), 1–28.
Elgar, F. J., Arlett, C., & Groves, R. (2003). Stress, coping, and behavioural problems among rural and urban adolescents. Journal of Adolescence,26(5), 574–585.
Erskine, J., Kvavilashvili, L., Myers, L., Leggett, S., Davies, S., Hiskey, S., et al. (2016). A longitudinal investigation of repressive coping and ageing. Aging & Mental Health,20(10), 1010–1020.
Evon, D. M., Golin, C. E., Ruffin, R., & Fried, M. W. (2017). Development and pilot-testing of a cognitive behavioral coping skills group intervention for patients with chronic hepatitis C. Contemporary Clinical Trials Communications,6, 85–96.
Faraji, E., Sardashti, S., Firouzeh, M. M., Aminabad, F. J., Alinaghi, S. A. S., & Hajiabdolbaghi, M. (2015). Perceived social support affects disease coping among people living with HIV: A study in Tehran, Iran. Asian Pacific Journal of Tropical Disease,5(5), 412–417.
Folkman, S. (2008). The case for positive emotions in the stress process. Anxiety Stress and Coping,21(1), 3–14.
Folkman, S., & Moskowitz, J. T. (2004). Coping: Pitfalls and promise. Annual Review of Psychology,55, 745–774.
Gooding, H. C., Organista, K., Burack, J., & Biesecker, B. B. (2006). Genetic susceptibility testing from a stress and coping perspective. Social Science & Medicine,62(8), 1880–1890.
Goldzweig, G., Andritsch, E., Hubert, A., Walach, N., Perry, S., Brenner, B., et al. (2009). How relevant is marital status and gender variables in coping with colorectal cancer? A sample of middle-aged and older cancer survivors. Psycho-Oncology,18(8), 866–874.
Gray, D. E. (2003). Gender and coping: The parents of children with high functioning autism. Social Science and Medicine,56(3), 631–642. https://doi.org/10.1016/S0277-9536(02)00059-X.
Hamarat, Dennis Thompson, Zabrucky, Karen M., Steele, Don, Matheny, Kenneth B., & Ferda Aysan, E. (2001). Perceived stress and coping resource availability as predictors of life satisfaction in young, middle-aged, and older adults. Experimental Aging Research,27(2), 181–196.
Heckman, T. G., Heckman, B. D., Kochman, A., Sikkema, K. J., Suhr, J., & Goodkin, K. (2002). Psychological symptoms among persons 50 years of age and older living with HIV disease. Aging & Mental Health,6(2), 121–128.
Hopwood, M., & Treloar, C. (2008). Resilient coping: Applying adaptive responses to prior adversity during treatment for hepatitis C infection. Journal of Health Psychology,13(1), 17–27.
Jensen, M. P., Turner, J. A., Romano, J. M., & Strom, S. E. (1995). The chronic pain coping inventory: Development and preliminary validation. Pain,60, 203–216.
Keefe, F. J., & Williams, D. A. (1990). A comparison of coping strategies in chronic pain patients in different age groups. Journal of Gerontology,45(4), 161–165.
Kelly, M. M., Tyrka, A. R., Anderson, G. M., Price, L. H., & Carpenter, L. L. (2008). Sex differences in emotional and physiological responses to the Trier Social Stress Test. Journal of Behavior Therapy and Experimental Psychiatry,39(1), 87–98.
Kim, I. H., Noh, S., & Chun, H. (2016). Mediating and moderating effects in ageism and depression among the Korean elderly: The roles of emotional reactions and coping reponses. Osong Public Health and Research Perspectives,7(1), 3–11.
King, G., Cathers, T., Brown, E., Specht, J. A., Willoughby, C., Polgar, J. M., et al. (2003). Turning points and protective processes in the lives of people with chronic disabilities. Qualitative Health Research,13, 184–206.
Koenig, H. G., Larson, D. B., & Larson, S. S. (2001). Religion and coping with serious medical illness. Annals of Pharmacotherapy,35(3), 352–359.
Kraus, M. R., Schäfer, A., Csef, H., Scheurlen, M., & Faller, H. (2000). Emotional state, coping styles, and somatic variables in patients with chronic hepatitis C. Psychosomatics,41(5), 377–384.
Krause, N. (1998). Stressors in highly valued roles, religious coping, and mortality. Psychology and Aging,13(2), 242–255.
Kuo, B. C., Arnold, R., & Rodriguez-Rubio, B. (2014). Mediating effects of coping in the link between spirituality and psychological distress in a culturally diverse undergraduate sample. Mental Health, Religion & Culture,17(2), 173–184.
Lancaster, B. L., & Palframan, J. T. (2009). Coping with major life events: The role of spirituality and self-transformation. Mental Health, Religion & Culture,12(3), 257–276.
Lazarus, R. S., & Folkman, S. (1984). Coping and adaptation. In W. D. Gentry (Ed.), The handbook of behavioral medicine (pp. 282–325). New York: Guilford.
Lynggaard, V., Nielsen, C. V., Zwisler, A. D., Taylor, R. S., & May, O. (2017). The patient education—Learning and Coping Strategies—improves adherence in cardiac rehabilitation (LC–REHAB): A randomised controlled trial. International Journal of Cardiology,236, 65–70.
Mahmoudi, M., Dehdari, T., Shojaeezadeh, D., & Abbasian, L. (2015). Coping with stress strategies in HIV-infected Iranian patients. Journal of the Association of Nurses in AIDS Care,26(4), 464–471.
Maan Diong, S., Bishop, G. D., Enkelmann, H. C., Tong, E. M., Why, Y. P., Ang, J. C., & Khader, M. (2005). Anger, stress, coping, social support and health: Modelling the relationships. Psychology & Health,20(4), 467–495.
Michael, T., Zetsche, U., & Margraf, J. (2007). Epidemiology of anxiety disorders. Psychiatry,6(4), 136–142.
Mirza, I., & Jenkins, R. (2004). Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: Systematic review. BMJ,328(7443), 794–798.
Mitschke, D. B., & Kang, S. Y. (2012). Social support and coping in families facing prostate cancer. Journal of Social Service Research,38(3), 413–426.
Naghi, J. J., Philip, K. J., Phan, A., Cleenewerck, L., & Schwarz, E. R. (2012). The effects of spirituality and religion on outcomes in patients with chronic heart failure. Journal of Religion and Health,51(4), 1124–1136.
Namageyo-Funa, A., Muilenburg, J., & Wilson, M. (2015). The role of religion and spirituality in coping with type 2 diabetes: A qualitative study among black men. Journal of Religion and Health,54(1), 242–252.
Nicholls, A. R., Polman, R., Levy, A. R., Taylor, J., & Cobley, S. (2007). Stressors, coping, and coping effectiveness: Gender, type of sport, and skill differences. Journal of Sports Sciences,25(13), 1521–1530.
Olson, M. M., Trevino, D. B., Geske, J. A., & Vanderpool, H. (2012). Religious coping and mental health outcomes: An exploratory study of socioeconomically disadvantaged patients. Explore: The Journal of Science and Healing,8(3), 172–176.
Pampel, F. C., Krueger, P. M., & Denney, J. T. (2010). Socioeconomic disparities in health behaviors. Annual Review of Sociology,36, 349–370.
Panayiotou, G., Karekla, M., & Leonidou, C. (2017). Coping through avoidance may explain gender disparities in anxiety. Journal of Contextual Behavioral Science,6(2), 215–220.
Panzini, R. G., & Bandeira, D. R. (2005). Spiritual/religious coping scale (SRCOPE Scale): Elaboration and construct validation. Psicologia em Estudo,10(3), 507–516.
Pargament, K. I. (1997). The psychology of religion and coping: Theory, research, practice. New York: Guilford.
Pargament, K. I. (2011). Religion and coping: The current state of knowledge. In S. Folkman (Ed.), Oxford handbook of stress health and coping. New York: Oxford University Press.
Pargament, K. I., Koenig, H. G., & Perez, L. M. (2000). The many methods of religious coping: Development and initial validation of the RCOPE. Journal of Clinical Psychology,56(4), 519–543.
Pargament, K. I., & Raiya, H. A. (2007). A decade of research on the psychology of religion and coping: Things we assumed and lessons we learned. Psyke & Logos,28(2), 25.
Paukert, A. L., LeMaire, A., & Cully, J. A. (2009). Predictors of depressive symptoms in older veterans with heart failure. Aging & Mental Health,13(4), 601–610.
Pepperell, T. A., Paynter, J., & Gilmore, L. (2016). Social support and coping strategies of parents raising a child with autism spectrum disorder. Early Child Development and Care,188, 1–13.
Rana, M., Gellrich, N. C., Czens, F., Kanatas, A., & Rana, M. (2014). Coping with oral cancer: The impact of health and disease-related personality traits. Supportive Care in Cancer,22(11), 2981–2986.
Richards, H., & Barry, R. (1998). US life tables for 1990 by sex, race, and education. Journal of Forensic Economics,11(1), 9–26.
Roohafza, H., Sadeghi, M., Shirani, S., Bahonar, A., Mackie, M., & Sarafzadegan, N. (2009). Association of socioeconomic status and life-style factors with coping strategies in Isfahan Healthy Heart Program, Iran. Croatian Medical Journal,50(4), 380–386.
Santavirta, N., Björvell, H., Solovieva, S., Alaranta, H., Hurskainen, K., & Konttinen, Y. T. (2001). Coping strategies, pain, and disability in patients with hemophilia and related disorders. Arthritis Care & Research,45(1), 48–55.
Scambler, G. (Ed.). (2005). Medical sociology: Coping with illness (Vol. 3). Milton Park: Taylor & Francis.
Schoenmakers, E. C., van Tilburg, T. G., & Fokkema, T. (2015). Problem-focused and emotion-focused coping options and loneliness: How are they related? European Journal of Ageing,12(2), 153–161.
Siegel, S., Milian, M., Kleist, B., Psaras, T., Tsiogka, M., Führer, D., Koltowska-Häggström, M., Honegger, J., Müller, O., Sure, U., Menzel, C., Buchfelder, M., Kreitschmann-Andermahr, I. (2016). Coping strategies have a strong impact on quality of life, depression, and embitterment in patients with Cushing’s disease. Pituitary,19(6), 590–600.
Smrtnik Vitulić, H., & Prosen, S. (2016). Coping and emotion regulation strategies in adulthood: Specificities regarding age, gender and level of education. Društvena istraživanja: časopis za opća društvena pitanja,25(1), 43–62.
Sohail, M. M. (2018). Belief in God’s Help during Hepatitis C: A Qualitative Study on Muslim Patients in Pakistan. Journal of Religion and Health. https://doi.org/10.1007/s10943-018-0700-5.
Sohail, M. M., Yasin, M. G., & Ahmad, S. (2017). A phenomenological account of social sources, coping effects and relational role of social support in nursing among chronic patients with hepatitis. Journal of Research in Nursing,23(1), 23–39.
Somerfield, M. R., & McCrae, R. R. (2000). Stress and coping research: Methodological challenges, theoretical advances, and clinical applications. American psychologist,55(6), 620.
Stegniga, S., Occhipinti, S., Dunn, J., Gardiner, R., Heathcote, P., & Yaxley, J. (2001). The supportive care needs of men with prostate cancer. Psycho-Oncology,10, 66–75.
Stewart, B. J., Mikocka-Walus, A. A., Harley, H., & Andrews, J. M. (2012). Help-seeking and coping with the psychosocial burden of chronic hepatitis C: A qualitative study of patient, hepatologist, and counsellor perspectives. International Journal of Nursing Studies,49(5), 560–569.
Stuart, M., & McGrew, J. H. (2009). Caregiver burden after receiving a diagnosis of an autism spectrum disorder. Research in Autism Spectrum Disorders,3, 86–97.
Suarez, A. E. (2017). Is disclosure a privilege? Race and disclosure patterns of hepatitis C. Journal of Health Psychology. https://doi.org/10.1177/1359105317694485.
Tamres, L. K., Janicki, D., & Helgeson, V. S. (2002). Sex differences in coping behavior: A meta-analytic review and an examination of relative coping. Personality and Social Psychology Review,6(1), 2–30.
Tewari, P., & Suryawanshi, S. K. (2015). Emotional need fulfillment in adolescents of joint family and nuclear family: A comparative study. Online Journal of Multidisciplinary Research (OJMR),1(1), 18–22.
Thoits, P. A. (1995). Stress, coping and social support processes: Where are we now? What next? Journal of Health and Social Behavior,35(Extra Issue), 53–79.
Turkington, C., Dempster, M., & Maguire, J. (2018). Adjustment to hand injury: Cross-sectional survey exploring adjustment in relation to illness perceptions and coping strategies. Journal of Hand Therapy,31(4), 502–510.
Vandsburger, E., & Biggerstaff, M. A. (2004). Evaluation of the stress adjustment and adaptation model among families reporting economic pressure. Journal of Family Social Work,8(2), 65–84.
Vitorino, L. M., Marins, L. S., Lucchetti, A. L. G., Santos, A. E. O., Cruz, J. P., Cortez, P. J. O., et al. (2018). Spiritual/religious coping and depressive symptoms in informal caregivers of hospitalized older adults. Geriatric Nursing,39(1), 48–53.
Výrost, J., Lova, L., Baumgartner, F., Bolfíková, E., Frankovský, M., & Hadu Ovská, S. (1995). Possibilities of empiric classifications of demanding life situations. Studia Psychologica,37(2), 93–106.
Walsh, T. M., Stewart, S. H., McLaughlin, E., & Comeau, N. (2004). Gender differences in childhood anxiety sensitivity index (CASI) dimensions. Journal of Anxiety Disorders,18(5), 695–706.
Whitty, M. T. (2003). Coping and defending: Age differences in maturity of defence mechanisms and coping strategies. Aging & Mental Health,7(2), 123–132.
Wingo, A. P., Baldessarini, R. J., & Windle, M. (2015). Coping styles: Longitudinal development from ages 17 to 33 and associations with psychiatric disorders. Psychiatry Research,225(3), 299–304.
Zabalegui, A., Cabrera, E., Navarro, M., & Cebria, M. I. (2013). Perceived social support and coping strategies in advanced cancer patients. Journal of Research in Nursing,18(5), 409–420.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical Approval
Researchers also ensured the quality and integrity of the research. All the participants participated in the study voluntarily. Confidentiality and anonymity of the respondents were also ensured. The research topic and study protocol were approved by the board of studies, advanced studies research board and the departmental research ethical committee (Advanced Studies Research Board (ASRB), University of Sargodha, Punjab, Pakistan).
Informed Consent
Research participants were recruited after proper informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sohail, M.M., Ahmad, S. & Maqsood, F. The Role of Socio-demographics in Adoption of Religious–Spiritual and Other Coping Strategies Among Muslim Chronic Patients with Hepatitis C in Pakistan. J Relig Health 59, 234–256 (2020). https://doi.org/10.1007/s10943-019-00761-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-019-00761-6