Abstract
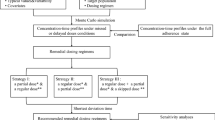
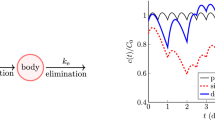
Missed doses, late doses, and other dosing irregularities are major barriers to effective pharmacotherapy, especially for the treatment of chronic conditions. What should a patient do if they did not take their last dose at the prescribed time? Should they take it late or skip it? In this paper, we investigate the pharmacokinetic effects of taking a late dose. We consider a single compartment model with linear absorption and elimination for a patient instructed to take doses at regular time intervals. We suppose that the patient forgets to take a dose and then realizes some time later and must decide what remedial steps to take. Using mathematical analysis, we derive several metrics which quantify the effects of taking the dose late. The metrics involve the difference between the drug concentration time courses for the case that the dose is taken late and the case that the dose is taken on time. In particular, the metrics are the integral of the absolute difference over all time, the maximum of the difference, and the maximum of the integral of the difference over any single dosing interval. We apply these general mathematical formulas to levothyroxine, atorvastatin, and immediate release and extended release formulations of lamotrigine. We further show how population variability can be immediately incorporated into these results. Finally, we use this analysis to propose general principles and strategies for dealing with dosing irregularities.







Similar content being viewed by others
References
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353(5):487–497
Coleman CI, Limone B, Sobieraj DM, Lee S, Roberts MS, Kaur R, Alam T (2012) Dosing frequency and medication adherence in chronic disease. J Manag Care Pharm 18(7):527–539
Burnier M (2019) Is there a threshold for medication adherence? lessons learnt from electronic monitoring of drug adherence. Front Pharmacol 9:1540
Thier SL, Yu-Isenberg KS, Leas BF, Cantrell CR, DeBussey S, Goldfarb NI, Nash DB (2008) In chronic disease, nationwide data show poor adherence by patients to medication and by physicians to guidelines. Manag Care 17(2):48–52
Paschal AM, Rush SE, Sadler T (2014) Factors associated with medication adherence in patients with epilepsy and recommendations for improvement. Epilepsy Behav 31:346–350
Cramer JA, Glassman M, Vincent R (2002) The relationship between poor medication compliance and seizures. Epilepsy Behav 3(4):338–342
Howard J, Wildman K, Blain J, Wills S, Brown D (1999) The importance of drug information from a patient perspective. J Soc Admin Pharm 16(3–4):115–126
Gilbert A, Roughead L, Sansom L et al (2002) I’ve missed a dose; what should I do? Austral Prescrib 25(1):16–17
Abdullah A, Hughes DA (2020) What should patients do if they miss a dose? A systematic review of patient information leaflets and summaries of product characteristics. Eur J Clin Pharmacol 1:1–10
Sankar AP, Nevedal DC, Neufeld Stewart, Luborsky MR (2007) What is a missed dose? implications for construct validity and patient adherence. AIDS Care 19(6):775–780
Millum J, Grady C (2013) The ethics of placebo-controlled trials: methodological justifications. Contemp Clin Trials 36(2):510–514
Brittain ST, Wheless JW (2015) Pharmacokinetic simulations of topiramate plasma concentrations following dosing irregularities with extended-release vs. immediate-release formulations. Epilepsy Behav 52:31–36
Gu J, Guo Y, Jiao Z, Ding J, Li G (2020) How to handle delayed or missed doses: a population pharmacokinetic perspective. Eur J Drug Metab Pharmacokinet 45(2):163–172
Gibaldi M, Perrier D (1982) Pharmacokinetics. Marcelly Dekker, 2nd edn. Wiley, New York
Bauer LA (2015) Clinical pharmacokinetic equations and calculations. McGraw-Hill Medical, New York
Lexicomp. Levothyroxine. http://online.lexi.com. Accessed 12 Jan 2022
Colucci P, Seng YC, Murray D, Salvatore B (2013) A review of the pharmacokinetics of levothyroxine for the treatment of hypothyroidism. Eur Endocrinol 9(1):40
Demiana WF, Urien S, Carreau V, Chauvenet M, Jean SH, Giral P, Bruckert E, Lechat P (2006) Use of an indirect effect model to describe the ldl cholesterol-lowering effect by statins in hypercholesterolaemic patients. Fund Clin Pharmacol 20(3):321–330
Chen C, Wright J, Gidal B, Messenheimer J (2013) Assessing impact of real-world dosing irregularities with lamotrigine extended-release and immediate-release formulations by pharmacokinetic simulation. Therapeut Drug Monit 35(2):188–193
Assawasuwannakit P, Braund R, Duffull SB (2015) Quantification of the forgiveness of drugs to imperfect adherence. CPT 4(3):204–211
Assawasuwannakit P, Braund R, Duffull SB (2016) A framework for quantifying the influence of adherence and dose individualization. Clin Pharmacol Therapeut 99(4):452–459
Pellock JM, Brittain ST (2016) Use of computer simulations to test the concept of dose forgiveness in the era of extended-release (XR) drugs. Epilepsy Behav 55:21–23
Morrison A, Stauffer ME, Kaufman AS (2017) Relationship between adherence rate threshold and drug ‘forgiveness’. Clin Pharmacokinet 56(12):1435–1440
Véronique D (2011) Drug forgiveness and interpatient pharmacokinetic variability in tuberculosis. J Infect Dis 204:1
Lowy A, Munk VC, Ong SH, Burnier M, Vrijens B, Tousset EP, Urquhart J (2011) Effects on blood pressure and cardiovascular risk of variations in patients? Adherence to prescribed antihypertensive drugs: role of duration of drug action. Int J Clin Pract 65(1):41–53
Nony P, Boissel J-P (2002) Use of sensitivity functions to characterise and compare the forgiveness of drugs. Clin Pharmacokinet 41(5):371–380
McAllister NP, Lawley SD (2022) A pharmacokinetic and pharmacodynamic analysis of drug forgiveness. Submitted
Brent GA, Koenig RJ (2017) Thyroid and antithyroid drugs. McGraw-Hill Education, New York
Clinic Mayo (2022) Levothyroxine. https://www.mayoclinic.org/drugs-supplements/levothyroxine-oral-route/proper-use/drg-20072133. Accessed 12 Jan 2022
RxList. Synthroid. https://www.rxlist.com/synthroid-drug/patient-images-side-effects.htm. Accessed 12 Jan 2022
Drugs.com. Levothyroxine. https://www.drugs.com/levothyroxine.html. Accessed 12 Jan 2022
National Health Service (UK). Levothyroxine. https://www.nhs.uk/medicines/levothyroxine/. Accessed 12 Jan 2022
Jacqueline J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, Cooper DS, Kim BW, Peeters RP, Rosenthal MS et al (2014) Guidelines for the treatment of hypothyroidism: prepared by the American thyroid association task force on thyroid hormone replacement. Thyroid 24(12):1670–1751
Lennernäs H (2003) Clinical pharmacokinetics of atorvastatin. Clin Pharmacokinet 42(13):1141–1160
April V, Cynthia S, Judith D (2017) Davis’s drug guide for nurses, 15th edn. New York, F.A, Davis Company
Healthline. Dosage for lipitor: what you need to know. https://www.healthline.com/health/drugs/lipitor-dosage. Accessed 12 Jan 2022
Mould DR, Upton RN (2013) Basic concepts in population modeling, simulation, and model-based drug development part 2: introduction to pharmacokinetic modeling methods. CPT 2(4):1–14
Qiu Y, Zhou D (2011) Understanding design and development of modified release solid oral dosage forms. J Valid Technol 17(2):23
Logan JD (2013) Applied mathematics. Wiley, New York
Garnett WR, McLean AM, Yuxin Z, Susan C, Tulloch SJ (2033) Simulation of the effect of patient nonadherence on plasma concentrations of carbamazepine from twice-daily extended-release capsules. Curr Med Res Opin 19(6):519–525
Reed RC, Dutta S (2004) Predicted serum valproic acid concentrations in patients missing and replacing a dose of extended-release divalproex sodium. Am J Health Syst Pharm 61(21):2284–2289
Dutta S, Reed RC (2006) Effect of delayed and/or missed enteric-coated divalproex doses on valproic acid concentrations: simulation and dose replacement recommendations for the clinician 1. J Clin Pharm Therapeut 31(4):321–329
Ding J, Zhang Y, Jiao Z, Wang Y (2012) The effect of poor compliance on the pharmacokinetics of carbamazepine and its epoxide metabolite using monte carlo simulation. Acta Pharmacol Sin 33(11):1431–1440
Gidal BE, Majid O, Ferry J, Hussein Z, Yang H, Zhu J, Fain R, Laurenza A (2014) The practical impact of altered dosing on perampanel plasma concentrations: pharmacokinetic modeling from clinical studies. Epilepsy Behav 35:6–12
Sunkaraneni S, Blum D, Ludwig E, Chudasama V, Fiedler-Kelly J, Marvanova M, Bainbridge J, Phillips L (2018) Population pharmacokinetic evaluation and missed-dose simulations for eslicarbazepine acetate monotherapy in patients with partial-onset seizures. Clin Pharmacol Drug Dev 7(3):287–297
Hard ML, Wehr AY, Sadler BM, Mills RJ, von Moltke L (2018) Population pharmacokinetic analysis and model-based simulations of aripiprazole for a 1-day initiation regimen for the long-acting antipsychotic aripiprazole lauroxil. Eur J Drug Metab Pharmacokinet 43(4):461–469
Elkomy MH (2020) Changing the drug delivery system: does it add to non-compliance ramifications control? A simulation study on the pharmacokinetics and pharmacodynamics of atypical antipsychotic drug. Pharmaceutics 12(4):297
Counterman ED, Lawley SD (2021) What should patients do if they miss a dose of medication? A theoretical approach. J Pharmacokinet Pharmacodyn 48:873
Counterman ED, Lawley SD (2022) Designing drug regimens that mitigate nonadherence. Bull Math Biol 84(1):1–36
Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M (2008) Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. Bmj 336(7653):1114–1117
Sun J, Nagaraj HN, Reynolds NR (2007) Discrete stochastic models for compliance analysis based on an AIDS clinical trial group (ACTG) study. Biometr J 49(5):731–741
McAllister NP, Lawley SD (2022) A pharmacokinetic and pharmacodynamic analysis of drug forgiveness. J Pharmacokinet Pharmacodyn 1:1–17
Felmlee MA, Morris ME, Mager DE (2012) Mechanism-based pharmacodynamic modeling. Computational toxicology. Springer, Cham, pp 583–600
Funding
SDL was supported by the National Science Foundation (Grant Nos. CAREER DMS-1944574 and DMS-1814832)
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
In this Appendix, we collect details of the mathematical analysis. We also present a fourth metric in Sect. 5.3 for studying the effects of a late dose.
Derivation of mathematical formulas
To calculate \(\rho ^{\text {skip}}\) in (15), we note that
where \(c_{0}(t)\) is defined in (5). Integrating (45) yields (16).
To calculate \(\rho _{-}\) and \(\rho _{+}\) defined in (13)-(14), we first use that (10) and (8) imply that \(\rho _{-}\) and \(\rho _{+}\) can be written in terms of \(\delta (t,d)\) in (8) as
where \({{s_{0}}}>d>0\) is such that \(\delta (t,d)<0\) for all \(t\in (0,{{s_{0}}})\) and \(\delta (t,d)>0\) for all \(t>{{s_{0}}}\). Solving for \({{s_{0}}}\) yields
Integrating (46) using (8) and (47) yields (17), which then yields (19) by (12).
To calculate \(\nu\) defined in (24), we first use (10) to obtain that \(\nu\) can be written in terms of \(\delta\) as
A simple calculus exercise yields that \(\delta (t,d)\) is maximized at \(t={{s_{1}}}\), where
Plugging (49) into (48) yields the formula for \(\nu\) in (26).
To calculate \(\gamma\) in (25), we first use (10) to obtain that \(\gamma\) can be written in terms of \(\delta\) as
Integrating (50) and performing a simple calculus exercise yields that the maximum in (50) occurs at \(t={{s_{2}}}\), where
Plugging (51) into (50) yields the formula for \(\gamma\) in (27).
Monotonicity
We now prove (32) and (33). Applying the chain rule to (19) yields
where \(f_{x}\) and \(f_{y}\) denote the partial derivatives of f in (18) with respect to x and y, respectively. Specifically,
and the formula for \(f_{y}(x,y)\) is obtained from (53) upon swapping x and y. Though (53) is a complicated expression, it is easy to plot as a function of \(x>0\) and \(y>0\) to obtain that
Hence, (54) and the expressions in (52) yield (32).
The sign of the partial derivatives of \(\gamma\) in (33) follow immediately from (27), the chain rule, and (54).
To obtain the sign of the partial derivatives of \(\nu\) in (33), we first note that the partial derivative of g in (28) with respect to x is
and the formula for \(g_{y}(x,y)\) is obtained from (55) upon swapping x and y. Though (55) is a complicated expression, it is easy to plot as a function of \(x>0\) and \(y>0\) to obtain that
Hence, the sign of the partial derivatives of \(\nu\) in (33) follow immediately from using (26), the chain rule, and (54) and (56).
Maximum concentration
In the main text of the paper, the metric \(\nu\) measures the maximum amount that \(c^{d}(t)\) can rise above c(t). To obtain the value for the maximum of \(c^{d}(t)\) rather than how the \(c^{d}(t)\) rises above c(t), we must make assumptions about the patient’s adherence before and after the late dose. For simplicity, we assume that the patient has perfect adherence for a long time before and after the late dose. Letting \(\{c^{\text {perf},d}(t)\}_{t\in {\mathbb {R}}}\) denote this concentration time course, we prove below that
where \(\delta\) is defined in (8) and
In (58), we use the floor function notation, in which \({\lfloor {x}\rfloor }\) denotes the largest integer less than or equal to x.
While the complicated formulas in (57)-(59) do not offer much intuition, they can be easily plotted to investigate how the maximum concentration depends on the various parameters. In Fig. 8, we plot
which is a dimensionless measure of how far \(c^{\text {perf},d}(t)\) rises above \({\langle }c^{\text {perf}}{\rangle }\), relative to \({\langle }c^{\text {perf}}{\rangle }\). The top left panel in Fig. 8 is for no delay (\(d=0\)) to show how the concentration time courses rises above the average \({\langle }c^{\text {perf}}{\rangle }\) for perfect adherence. In this case of no delay, \(\theta\) has a simpler formula which we denote by \(\theta ^{\text {perf}}\),
The bottom right panel shows that even in the extreme case of a double dose (\(d=\tau\)), the drug concentration rises only slightly above the average if the absorption and/or elimination rate is sufficiently slow compared to \(1/\tau\). Conversely, this plot shows that the drug concentration can rise far above the average if both the absorption and elimination rate is sufficiently fast compared to \(1/\tau\). Analogous to Figs. 2 and 4, the letter markers in Fig. 8 are for the drugs in Table 1.
To obtain the formula for \(\max _{t\in {\mathbb {R}}}c^{\text {perf},d}(t)\) in (57), we first note that
where \(c^{\text {perf}}(t)\) is defined in (6). Now, \(\delta (t,d)\) is strictly increasing for \(t\in ({{s_{0}}},{{s_{1}}})\) and strictly decreasing for \(t\in ({{s_{1}}},\infty )\). It therefore follows that \({{s_{2}}}\in ({{s_{0}}},{{s_{1}}})\) is such that \(\delta ({{t_{1}}},d)>\delta (t_{0},d)\) if \({{t_{1}}}\in ({{s_{2}}},{{s_{2}}}+\tau )\) and \(t_{0}\notin ({{s_{2}}},{{s_{2}}}+\tau )\). Since \(c^{\text {perf}}(t)\) is periodic with period \(\tau\), it follows from (62) that the maximum of \(c^{\text {perf},d}(t)\) must occur at some \(t\in [{{s_{2}}},{{s_{2}}}+\tau ]\). Now, since \(j^{*}\) in (58) satisfies \(j^{*}={\lfloor {{{s_{2}}}/\tau }\rfloor }\), it follows that the maximum of \(c^{\text {perf},d}(t)\) must occur at some \(t\in [j^{*}\tau ,(j^{*}+2)\tau ]\) since \([{{s_{2}}},{{s_{2}}}+\tau ]\subset [j^{*}\tau ,(j^{*}+2)\tau ]\). If \(t=j\tau +s\) for some fixed integer \(j\in {\mathbb {Z}}\) and some time \(s\in [0,\tau ]\), then it follows immediately from (6) that
Hence, (62) implies \(c^{\text {perf},d}(j\tau +s)=C_{j}^{d}(s)\) where \(C_{j}^{d}(s)\) is defined to be
Differentiating (64) with respect to s shows that \(\frac{\text {d}}{\text {d}s}C_{j}^{d}(s)=0\) if \(s=t_{j}\) where \(t_{j}\) is defined in (59). Hence, we have obtained (57).
To obtain \(\max _{t\in {\mathbb {R}}}c^{\text {perf}}(t)\), we merely differentiate (63) with respect to s to find the maximum. Plugging the resulting expression into the definition of \(\theta\) in (60) yields the formula for \(\theta ^{\text {perf}}\) in (61).
Rights and permissions
About this article
Cite this article
Clark, E.D., Lawley, S.D. Should patients skip late doses of medication? A pharmacokinetic perspective. J Pharmacokinet Pharmacodyn 49, 429–444 (2022). https://doi.org/10.1007/s10928-022-09812-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-022-09812-0