Abstract
Introduction: The primary objectives were to compare the duration of sickness absence in employees with high levels of somatic symptom severity (HLSSS) with employees with lower levels of somatic symptom severity, and to establish the long-term outcomes concerning return to work (RTW), disability and discharge. Secondary objective was to evaluate determinants of the duration of sickness absence in employees with HLSSS. Methods: 489 sick-listed employees registered with five Occupational Health Physician (OHP) group practices were included in this study. We measured their baseline scores for somatic symptoms severity, depressive disorders, anxiety disorders, health anxiety, distress and functional impairment. The OHPs filled in a questionnaire on their diagnosis. A prospective 2-year follow-up was carried out to assess the long-term outcomes concerning sickness absence, and retrospective information was gathered with regard to sickness absence during the 12 months before the employees were sick-listed. Results: The median duration of sickness absence was 78 days longer for employees with HLSSS. They more often remained disabled and were discharged more often, especially due to problems in the relationship between the employer and the employee. HLSSS, health anxiety and older age contributed to a longer duration of sickness absence of employees. Conclusion: High levels of somatic symptom severity are a determinant of prolonged sickness absence, enduring disabilities and health-related job loss. Occupational health physicians should identify employees who are at risk and adhere to guidelines for medically unexplained somatic symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kroenke et al. [1] found that patients with high levels of somatic symptom severity (HLSSS) constituted 10 and 9% of samples in primary care and medical outpatient populations. These patients were severely bothered by multiple common somatic symptoms like fatigue, dizziness, and non-cardiac chest pain. The prevalence of HLSSS is in the same range as abridged somatization disorder, which is a clinical meaningful subthreshold somatoform disorder [2], whereby for this diagnosis it is needed that medical explanations are excluded and that the somatic symptoms resulted in medical help seeking behavior. HLSSS in patient samples are associated with reduced health-related functioning [3], disabilities and sickness absence, even after adjustment for psychiatric and medical co-morbidity [4, 5]. These associations with reduced functioning are linear with the level of somatic symptom severity [1]. Patients with long lasting medically unexplained somatic symptoms are more often disabled and unemployed [6]. Although single somatic symptoms are often self-limiting, patients with multiple somatic symptoms have a lower recovery rate [7]. About 15–30% of the patients with medically unexplained somatic symptoms or somatization do not recover or get worse [8].
In the working population the level of somatic symptom severity is much lower [9] than in the sick-listed population [10–12], where we found a prevalence of HLSSS of 15% [12]. There is limited information about the ‘transitions’ from healthy working employees, to employees with HLSSS and sickness absence, and subsequently to employees with chronic disability and to unemployment.
Higher levels of somatic symptom severity are in the working population associated with reduced health-related functioning [11], frequent sickness absence [13], a longer duration of sickness absence [11] and higher risk of a disability pension [10]. An employee’s expectation of a long sickness absence and an increase in pain predict barriers for return to work (RTW) [14]. These findings give rise to our hypothesis that high levels of somatic symptom severity will result in longer duration of sickness absence and may result in more lasting disabilities.
With regard to unemployment, Haahr et al. [15] found that health-related job loss (HRJL) was associated with body discomfort due to musculoskeletal pain, high pain levels, health worries and stress-related problems. Although it was not verified if the musculoskeletal pain was non-specific, this study gives an indication that HLSSS may result in more unemployment.
However, there is a lack of longitudinal studies of employees, measured with validated instruments to determine the course of medically unexplained somatic symptoms and related outcomes. We report here on a 2-year follow-up of a sample of long-term sick-listed employees with HLSSS and lower levels of somatic symptom severity, in order to test our hypothesis that employees with HLSSS are more at risk for lasting disabilities and discharge.
The research questions we addressed in this study were:
-
1.
What is the duration of sickness absence in sick-listed employees with HLSSS, compared to sick-listed employees with lower levels of somatic symptom severity and what was the duration and frequency of sickness absence 1 year before the sick-listed period?
-
2.
What are the long-term outcomes in terms of complete RTW, disability and discharge for sick-listed employees with HLSSS compared to sick-listed employees with lower levels of somatic symptom severity?
-
3.
What are the determinants of the duration of sickness absence in sick-listed employees with HLSSS?
Methods
Introduction
The law in the Netherlands states that employees who report sick must be seen before the sixth week of sick-leave (first consultation) by an occupational health physician (OHP), who will establish the diagnosis, the disabilities, and the prognosis for RTW. The maximum period of sickness certification is 2 years, after which an employee who is still disabled can apply for a state disability pension. However, an employer can choose to pay the employee for a longer period of sickness absence with a maximum of 3 years. This happens mainly in local and central government. Most of the visits made by the employees to OHPs in the Netherlands concern consultations for sickness certification.
Design
We carried out an observational study with a prospective follow-up of 2 years and a 1-year period of retrospective data collection.
Patients
Sick-listed employees were included in the study from April 2006 until December 2007. Their characteristics are described in Table 1.
OHPs
A total of 43 OHPs from five group practices in two large occupational health services in the Netherlands participated in this study. The group practices, located in four different geographical regions of the Netherlands, provide services for organisations of different sizes and branches located in urban and rural areas (Table 2).
Data-Collection
In the inclusion period the employee questionnaires and the OHP questionnaires were gathered during a period of 6 weeks in each of the five group practices. Follow-up ended March 2009 with gathering the data for 2 years follow-up of employees from the first four group practices and for 1 year follow-up of employees from the fifth group. Data on sickness absence were gathered from the information systems of the two occupational health services.
Measurements
Patient Questionnaires
The employees were asked to answer questions about socio-demographic variables and to fill in the following questionnaires, to measure:
-
(a)
Somatic symptom severity, with the somatization module of the PHQ, the PHQ-15 [3, 16]. The PHQ-15 assesses how much the patient has been bothered during the past month (score 0–2; ranging from not bothered at all to bothered a lot) by 15 common physical complaints. These complaints are moderately related to a history of medically unexplained symptoms [17] and are associated with significant impairment in health-related functioning [1]. Cut-off levels are 0, 5, 10 and 15 for minimal, low, medium and high levels of somatic symptom severity. The cut-off point of 15 for high levels of somatic symptoms severity (PHQ-15 ≥ 15) is comparable with clinically representative samples of somatoform disorders with a lower threshold than somatisation disorder [17]. The internal consistency of the PHQ-15 is good (Cronbach’s α = 0.80) [3, 18]. Its sensitivity and specificity have been established in a primary care population as 78% and 71%, respectively, at a cut-off level of 3 symptoms or more, with a low positive predictive value and a high negative predictive value [18]. Its test–retest reliability is moderate with a score of 0.60. Although limited research has focused on this questionnaire it seems to be reliable for the identification of patients who are at risk for somatoform disorders [18].
-
(b)
Depression, with the depression module of the Patient Health Questionnaire (PHQ-9) [16, 19]. The PHQ-9 rates how much the patient has been bothered during the past 2 weeks (score 0–3) by 9 symptoms of depression. Total scores for the 9 symptoms range from 0 to 27, with a cut-off point of 15 (PHQ-9 ≥ 15) for severe levels of depression. Two questions (about feeling tired and sleeping problems), in the PHQ-9 are also included in the PHQ-15. Although this makes the PHQ-9 score less independent of the PHQ-15 score, it has been reported to have high construct validity and strong associations with clinical variables in the general population [19]. Algorithms, based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria, are applied to help the physician to discern a major depressive disorder from any depressive disorder (excluding the other diagnosis).
-
(c)
Anxiety disorders, with the anxiety module of the Patient Health Questionnaire (PHQ) [16, 20]. This subscale of the PHQ contains 15 yes/no questions about anxiety and panic symptoms, and is used with algorithms for panic disorder and other anxiety disorders. The algorithm for panic disorder is the most valid, with a sensitivity of 75% and a specificity of 96% [20].
-
(d)
Health anxiety, with the Whitely Index (WI). This 14-item yes/no self-report questionnaire, which was designed to assess hypochondriasis [21], can be used to measure levels of health anxiety. Higher levels of health anxiety are related to less symptom recovery after 1 year [22].
-
(e)
Distress, with the distress module of the 4-Dimensional Symptom Questionnaire (4DSQ) [9, 23]. This Dutch questionnaire is internally consistent, with a Cronbach’s alpha of 0.90 for distress. Total distress scores for the sixteen distress items range from 0 to 32, with a cut-off point of 20 for severe distress.
-
(f)
Functional impairment, with a Dutch translation of the Short Form Health Survey (SF-36) [24]. The SF-36 is well validated [25] and measures eight aspects of health-related quality of life.
OHP Questionnaire—Employee and Consultation Characteristics
This OHP questionnaire contained questions about the presence of physical symptoms, the causes to which the employees attributed their physical complaints (physical, mental or physiologic), and the diagnosis made by the OHP (categorized as musculoskeletal, mental and other disorders).
Information About Sickness Absence
Information about duration and frequency of sickness absence was gathered from the registration systems of the occupational health services. The following data were retrieved:
-
Duration in days of sickness absence during the period in which the employee was included, this will be further referred to as ‘baseline sickness absence’, with retrospective gathering of the starting date on this sickness-absence period and a maximum follow-up period of 2 years after inclusion. Partial RTW was not measured, only duration until complete RTW (as duration of sickness absence).
-
Sickness absence periods (duration in days and number of periods) in the 12 months prior to the baseline sickness absence.
The long-term outcome of the sickness absence from inclusion was retrieved from the registration systems of the occupational health services and classified as:
-
1.
Ending sickness absence due to:
-
complete return to own work (RTW) and no new period of sickness absence within 4 weeks after complete RTW;
-
complete RTW to different work (although no continued disability and with the same salary);
-
pregnancy leave;
-
discharge.
-
-
2.
Continued disability:
-
disabled for own work, doing no work at all, doing partially own work, doing partially or completely different work due to the disability, no disability pension but less salary, applying for disability pension, or receiving a disability pension;
-
disabled and discharge due to total and permanent occupational disability;
-
disabled and discharge due to problems in the employer–employee relationship.
-
-
3.
Unknown:
-
employer changed to another occupational health service;
-
outcome not registered.
-
The information about the employees included by one of the occupational health services was retrieved by the main author from the central information system. The information about the employees included by the other occupational health service was provided by the participating OHPs, because they had no central registration system.
Data-Analysis
A missing value analysis was performed for baseline data on age, gender, level of education, ethnicity, and missing PHQ score at follow-up.
In the analysis on duration of sickness absence, employees were dichotomized into employees with HLSSS, categorised as the PHQ ≥ 15 group (the PHQ 15+ group), and the employees with moderate, mild or minimal somatic symptom severity, categorised as the PHQ < 15 group (the PHQ 15− group). Independent Student t-tests were performed for continuous variables, and Mann–Whitney U tests were performed for non-parametric distributions. Chi-square tests were performed for categorical variables. Chi-square trend tests were performed to investigate trends for ordinal variables.
We censored all data on the duration of sickness absence to 2 years, because this is the maximum period of sickness absence if there is no complete RTW. All cases in which the sickness absence continued after the end of the data-collection (September 2008) were also censored. This concerned a minority of the cases, all belonging to one group practice.
Partial RTW and the percentage of RTW were not included in any of the analyses because the relevant information obtained from the employers on this subject was not consistent.
To identify the determinants for the duration of the sickness absence, we constructed a Cox regression model. First, we assessed the univariate associations. We chose the following independent variables based on literature: gender, age, ethnicity, group practice, attribution of the employee, HLSSS, depressive symptoms, health anxiety symptoms, distress symptoms, panic disorder and anxiety disorder. The significant univariate determinants were included in a first Cox regression model for multivariate associations. Finally we removed the non-significant determinants from this model to construct a second Cox regression model.
Results
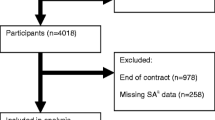
The eligible study population consisted of 812 sick-listed employees, of whom 489 participated in this study (response 60.2%) as described elsewhere [13]. We retrieved follow-up data from 401 employees (follow-up rate: 83.6%). For 80 sick-listed employees no follow-up data could be retrieved because of missing data in the local computer registration system of one of the two participating occupational health services. For eight sick-listed employees follow-data were incomplete.
Participants with no follow-up were comparable to those who completed the follow-up with regard to gender, age, level of education and PHQ-15 score, but in the non-response group more employees belonged to ethnic minority groups (20% vs. 12%, P = 0.017).
The baseline characteristics of the PHQ15+ and PHQ15− group are presented in Table 1. The total number of days and frequency of sickness absence during 1 year before baseline sickness absence were comparable.
The median duration of sickness absence was 78 days longer (P = 0.039) for employees with high levels of somatic symptom severity than for employees with moderate, mild and minimal levels of symptoms severity. The median duration of sickness absence in the total study population was 273 days.
The long-term outcomes of the sickness absence are shown in Table 3. In the PHQ15+ group more employees were still disabled after 2 years, and more employees were discharged because of problems in the employer-employee relationship.
In univariate analyses the duration of sickness absence was associated with HLSSS, depression symptom score, anxiety disorder, health anxiety score, distress, age and group practice 2 (See Table 4).
The Cox regression analysis (see Table 5, Model 1) with the univariate significant determinants showed that older age and health anxiety contributed to a longer duration of sickness absence. Group practices 2, 4 and 5 contributed to a shorter duration of sickness absence. After removing the multivariate non-significant determinants other than having HLSSS (Table 5, Model 2), having HLSSS showed also to be also a significant determinant as health anxiety score, age and group practices 2, 4 and 5. Posthoc analysis showed that health anxiety was a confounder of the relationship between anxiety disorder and distress on the one hand and duration of sickness absence on the other hand.
In group practice 1 with an over-representation of middle sized non-profit organizations like educational, local government and health care organisations and in group practice 3, with many small sized organizations in a rural area, there was also a longer duration of sickness absence. Group practice 2 with large government organisations (non-profit), with each OHP being responsible for ~2,500 employees of the same organisation, and group practices 4 and 5 with a mix of middle sized organizations contributed also to shorter duration of sickness absence.
Discussion
We found a longer duration of sickness absence among sick-listed employees with HLSSS (340 days) than among employees with lower levels of somatic symptom severity (262 days) in this sample of long-term sick-listed employees. These findings are in line with earlier findings that longer lasting higher levels of somatic symptom severity result in more disabilities [3], a longer sickness absence [10, 11] and more lasting disabilities [10].
In contradiction to the findings mentioned above, the total amount of sickness absence (days and frequency) before baseline sickness absence was not higher among employees with HLSSS. It is unclear whether or not this would have been the same in a longer-term retrospective study. The role of selection by lasting disabilities and discharge of sick-listed employees with HLSSS must also be taken into account. Another factor could be that employees with HLSSS manage to continue working in spite of their symptoms for a certain period of time, during which fear for health-related job loss (HRJL) could be an important factor, after which they have a longer period of sickness absence.
We found an indication that HLSSS more often contributed to discharge during sickness absence, because of problems in the employer-employee relationship. From a longitudinal observational study it is not possible to draw conclusions about causal relationships, but our results show that sick-listed employees with HLSSS, and an associated decrease in health related functioning, are at risk for HRJL and a longer period of sickness absence. This suggests that HLSSS contribute to the transition from a working employee to an unemployed and disabled patient.
The Cox regression analysis showed that HLSSS and health anxiety, but not psychiatric co-morbidity (depressive, anxiety and panic disorder) contribute to a longer duration of sickness absence. This is in line with the studies of Barsky et al. [4] and Harris et al. [5], who found in a primary care population that HLSSS showed stronger associations with functional limitations and medical consumption than with psychiatric co-morbidity. Another explanation might be that psychiatric co-morbidity is managed well by OHPs and treating physicians according the guidelines for common mental disorders (CMDs).
Health anxiety showed to be a determinant. So for OHPs it is besides the recognition of HLSSS important to recognize the health anxiety in order to give adequate reassurance. In employees with temporary and moderate levels of health anxiety this may be enough to continue the process of RTW. In employees with persistent and high levels of health anxiety which result in hampering process of RTW a referral for cognitive behavioral therapy (CBT) is according literature the best intervention [26, 27].
Determinants that are not directly symptom related that hamper RTW are age and certain factors of organization and occupational health care. We know from older employees that they have a graduate decline in physical abilities and that with increasing age the amount of somatic co-morbidity grows. It can be imagined that this attributes to fatigue, as the Maastricht Cohort Study [28, 29] shows and to sickness absence [30]. A study of Roelen et al. [31] showed that worse working conditions and age are associated with more self-reported symptoms. Furthermore, although older employees report less mental disorders, higher age is related to less recovery of depression [32]. A review [8] reported only an inconsistent weak association between older age and worse prognosis, but according to our data the combination of older age and specific work conditions is a risk factor when an employee gets sick-listed, so it is important to give these employees extra guidance.
The influence of group practices on duration of sickness absence might indicate that employees in middle sized non-profit organisations and also their employers, have major difficulties in mastering the process of RTW. From the results of earlier studies [33, 34] we know that certain non-profit branches such as education and local government have a longer duration of sickness absence, and more fatigue and chronic ill employees, than employees in profit-orientated branches. As group practice 2 with large governmental organizations attributed to a shorter duration of sickness absence there must be other factors as these organizations are also non-profit organizations. Possible is that larger non-profit organizations, especially when central government, have higher quality of internal processes. Their occupational health service is more centralized and can therefore be more specialised. Specific conclusions are not possible from our data.
Strengths and Limitations
A strength of our study is that, to our knowledge, this is the first large-scale study of sickness absence in sick-listed employees with a follow-up of 2 years, after baseline measurements with validated questionnaires, assessing somatic symptom severity, psychiatric morbidity, OHP diagnosis and the attribution of the employee. The duration of sickness absence was measured with computer-registered data, which are more accurate than measurements based on self-report.
The participation of five different group practices located in urban and rural areas, and the participation of employees from different branches of small and large companies, enhances the generalisability of the results.
From the results of our longitudinal observational study, no conclusions can be drawn with regard to the underlying causes of somatic symptom severity. This is especially important with regard to the associations between somatic symptom severity on the one hand, and psychiatric co-morbidity, distress and health anxiety on the other hand.
An important limitation is that self-report questionnaires were used for our main outcomes, and no medical examination was performed to find somatic explanations for the multiple physical symptoms. Such an examination is necessary to confirm that a physical symptom can not be explained by a somatic disease. However, it should be noted that the OHPs in their consultations usually ask and check for somatic causes, and perform physical examinations on indication. The median duration of sickness absence of 6 months at inclusion, is that long that many somatic causes will have manifested themselves. Furthermore, the questionnaires we used were well validated, and in the literature there is enough evidence that the PHQ is moderate reliable, but better than other comparable questionnaires, in indicating medically unexplained somatic symptoms [3, 17, 18].
Our sample consisted of sick-listed employees, who were included after a mean sickness absence of 6 months. In the total study population there was a median sickness absence of 273 days, illustrating that our findings relate to a population of employees with long-term sickness absence. On the one hand, we can draw no conclusion about short-term sickness absence in relation to somatic symptom severity, but on the other hand our findings indicate that HLSSS are associated with lasting disabilities, resulting in more disability pensions.
The small number of employees with HLSSS in our study resulted in broad confidence intervals in the results of the Cox regression analysis.
Implications for Practice
Since high HLSSS appears to be a predictor for long-term sickness absence [10] and HRJL [15], OHPs’ recognition of these symptoms should be improved.
The results of our earlier study [12] showed that OHPs tend to label HLSSS as signs of mental disorders, without diagnosing somatization as such. Even accepting this, due to difficulties in the categorisation of HLSSS [35, 36], the sick-listed employees should be screened by the OHP for HLSSS and this can be done reliably with the PHQ-15.
Adhering to the guidelines for the management and treatment of employees with medically unexplained somatic symptoms is important. There do exist guidelines for the treatment of patients with functional syndromes, [37] which also can be seen as clusters of medically unexplained somatic symptoms, and a multidisciplinary guideline for ‘somatic insufficient explained physical symptoms’ is being authorized in the Netherlands [38].
Morbidity and co-morbidity, and the adequacy of treatment, should be explored, as well as contributing factors at work and at home and coping styles. The employee should be asked to formulate a prognosis for RTW, because this is an important prognostic factor [14, 39].
When the process of RTW is hampered, early intervention should be considered. Reviews [40, 41] show that patients with functional syndromes and somatoform disorders with hampered recovery can benefit from cognitive behavioral therapy and multidisciplinary treatment. An interesting possibility is collaborative care [42],in which the employee has a consultation with the psychiatrist and the OHP together. This has been found to be effective in general practice [39].
Especially after recognising HLSSS in older employees, the OHP should check whether these employees have problems with the balance between their abilities and their workload.
Since it is known that education and local government branches have a longer duration of sickness absence, and more fatigue and chronic ill employees, than employees in profit-orientated branches [33, 34]. In these branches employers and OHPs should pay extra attention to employees with HLSSS in order to prevent and limit sickness absence.
Implications for Research
Kant et al. [43] indicated that in certain cases early consultation with the OHP before actual sickness absence is effective in reducing sickness absence in office workers who are at high risk for long-term sickness absence. We recommend an intervention study to assess the effectiveness of early consultation and management according to guidelines for employees with medically unexplained somatic symptoms.
There is also a need for more information on the course of medically unexplained somatic symptoms in sick-listed employees. A follow-up study based on validated questionnaires at different measurement moments (e.g. 6, 12, 24 months), will be useful, to establish the prognostic determinants more precisely.
Our findings about the influence of group practice are exploratory and further research is needed about which factors in organizations and occupational health care determine duration of sickness absence in sick-listed employees with medically unexplained somatic symptoms.
Final Conclusions
In conclusion, we found that HLSSS contribute to longer sickness absence, long-term disability and discharge. This indicates that HLSSS contribute to the ‘transition’ of working employees to a disabled and/or unemployed status. Especially at risk are employees with HLSSS accompanied with health anxiety, older employees and employees in certain organizations possibly in combination with lower level of occupational health care. We recommend that OHPs use the PHQ-15 to assess somatic symptom severity and to investigate and eliminate barriers for RTW.
References
Kroenke K, Spitzer RL, Williams JB. The PHQ-15: Validity of a new measure for evaluation of the severity of somatic symptoms. Psychosom Med. 2002;64:258–66.
Escobar JI, Burnam A, Karno M, Forsythe A, Goldinig JM. Somatisation in the community. Arch Gen Psych. 1987;44:713–8.
Jackson J, Fiddler M, Kapur N, Wells A, Tomenson B, Creed F. Number of bodily symptoms predicts outcome more accurately than health anxiety in patients attending neurology, cardiology and gastroenterology clinics. J Psychosom Res. 2006;60:357–63.
Barsky AJ, Orav J, Bates DW. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psych. 2005;62:903–10.
Harris AM, Orav EJ, Bates DW, Barsky AJ. Somatization increases disability independent of comorbidity. J Gen Intern Med. 2009;24:155–61.
Escobar JI, Golding JM, Hough RL, Karno M, Burnam MA, Wells KB. Somatization in the community: relationship to disability and use of services. Am J Public Health. 1987;77:837–40.
Jackson JL, Passamonti M. The outcomes among patients presenting in primary care with a physical symptom at 5 years. J Gen Intern Med. 2005;20:1031–7.
Olde Hartman TC, Borghuis MS, Lucassen PL, Van der Laar FA, Speckens AE, Van Weel C. Medically unexplained symptoms, somatisation disorder and hypochondriasis: course and prognosis. A systematic review. J Psychosom Res. 2009;66:363–77.
Terluin B, Van Rhenen W, Schaufeli WB, De Haan M. The Four-Dimensional Symptom Questionnaire (4DSQ): measuring distress and other mental health problems in a working population. Work Stress. 2004;18:187–207.
Eriksen HR, Svendsrod R, Ursin G, Ursin H. Prevalence of subjective health complaints in the Nordic European countries in 1993. Eur J Public Health. 1998;8:294–8.
Hansen A, Edlund C, Bränholm I-B. Significant resources needed for return to work after sick leave. Work. 2005;25:231–40.
Hoedeman R, Krol B, Blankenstein AH, Koopmans PC, Groothoff JW. Severe MUPS in a sick-listed population: a cross-sectional study on prevalence, recognition, psychiatric co-morbidity and impairment. BMC Public Health. 2009;9:440.
Norrmén G, Svärdsudd K, Andersson DKG. How primary health care physicians make sick listing decisions: The impact of medical factors and functioning. BMC Fam Pract. 2008;9:3.
Heijbel B, Josephson M, Jensen I, Stark S, Vingärd E. Return to work expectation predicts work in chronic musculoskeletal and behavioral health disorders: prospective study with clinical implications. J Occup Rehabil. 2006;16:173–84.
Haahr JPL, Frost P, Andersen JH. Predictors of health related job loss: a two-year follow-up study in a general working population. J Occup Rehabil. 2007;17:581–92.
Spitzler RL, Kroenke K, Williams JB, Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282:1737–44.
Interian A, Allen LA, Gara MA, Escobar JI, Diaz-Martinez AM. Somatic complaints in primary care: further examining the validity of the Patient Health Questionnaire (PHQ-15). Psychosom. 2006;47:392–8.
Van Ravestijn H, Wittkampf K, Lucassen P, Van de Lisdonk E, Van den Hoogen H, Van Weert H, et al. Detecting somatoform disorders in primary care with the PHQ-15. Ann Fam Med. 2009;7:232–8.
Löwe B, Spitzer RL, Gräfe K, Kroenke K, Quenter A, Zipfel S, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians diagnoses. J Affect Disord. 2004;78:131–40.
Löwe B, Gräfe K, Zipfel S, Spitzer RL, Herrmann-Lingen C, Witte S, et al. Detecting panic disorder in medical and psychosomatic outpatients: comparative validation of the Hospital Anxiety and Depression Scale, the Patient Health Questionnaire, a screening question, and physicians diagnosis. J Psychosom Res. 2003;55:515–9.
Pilowsky I. Dimensions of hypochondriasis. Br J Psych. 1967;113:39–43.
Speckens AEM, Spinhoven P, Sloekers PPA, Bolk JH, Van Hemert AM. A validation study of the Whitely Index, the Illness Attitude Scales, and the Somatosensory Amplification Scale in general medical and general practice patients. J Psychosom Res. 1996;40:95–104.
Terluin B, Van Marwijk HWJ, Ader HJ, De Vet HCW, Penninx BWJH, Hermens MLM, et al. The four-dimensional symptom questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry. 2006;6:34.
Van der Zee KI, Sanderman R. Het meten van de algemene gezondheidstoestand met de RAND-36. Een handleiding. [Manual for measuring health-related functioning with the RAND-36]. Groningen. Noordelijk Centrum voor Gezondheidsvraagstukken. 1993.
Ware JE, Sherbourne CD. The MOS 36-item short form health survey (SF-36). Conceptual framework and item selection. Med Care. 1992;30:473–83.
Barsky A. The patient with hypochondriasis. N Engl J Med. 2001;345:1395–9.
Thomson A, Page L. Psychotherapies for hypochondriasis. Cochrane Database Syst Rev. 2007;4. CD006520.
Van Amelsvoort LPGM, Kant I, Beurskens AJHM, Shroer CA. Swaen GMl. Fatigue as a predictor of work disability. Occup Environ Med. 2002;59:712–3.
Janssen N, Kant I, Swaen GMH, Janssen PP, Schroer CA. Fatigue as a predictor of sickness absence: results from the Maastricht cohort study on fatigue at work. Occup Environ Med. 2003;60(Suppl 1):171–6.
Duijts SF, Kant I, Swaen GM, Van den Brandt PA, Zeegers MP. A meta-analysis of observational studies identifies predictors of sickness absence. J Clin Epidemiol. 2007;60:1105–15.
Roelen CAM, Van der Pol TR, Koopmans PC, Groothoff JW. Identifying workers at risk of sickness absence by questionnaire. Occup Med. 2006;56:442–6.
Nieuwenhuijsen K, Verbeek JHAM, De Boer AGEM, Blonk RW, Van Dijk FJ. Predicting the duration of sickness absence for patients with common mental disorders in occupational health care. Scand J Work Env Health. 2006;32:67–74.
Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. J Epidemiol Community Health. 2000;54:502–9.
Schroër CAP, Janssen M, Van Amelsfoort LGPM, Bosma H, Swaen GMH, Nijhuis FJN, et al. Organizational characteristics as predictor of work disability: a prospective study among sick employees of for-profit and not-for-profit organizations. J Occup Rehabil. 2005;15:435–45.
Fink P, Sorensen L, Engberg M, Holm M, Munk-Jorgensen P. Somatization in primary care. Prevalence, health care utilization, and general practitioner recognition. Psychosom. 1999;40:330–8.
O’Neill E, McNamee R, Agius R, Gittins M, Hussey L, Turner S. The validity and reliability of diagnoses of work-related mental ill-health. Occup Environ Med. 2008;50:451–8.
National Institute for Health and Clinical Excellence. Guideline 53: Chronic fatigue syndrome/myalgic encephalomyalitis (or encephalopathy). NICE, London. 2007.
Multidisciplinaire richtlijn. Somatisch onvoldoende verklaarde lichamelijke klachten en somatoforme stoornissen. [Multidisciplinary guideline. Somatically insufficiëntly explained physical symptoms and somatoform disorders]. Trimbos Institute. 2009.
Marhold C, Linton SJ, Melin L. Identification of obstacles for chronic pain patients to return to work: evaluation of a questionnaire. J Occup Rehabil. 2002;12:65–75.
Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes. Lancet. 2007;369:946–55.
Sumathipala A. What is the evidence for the efficacy of treatments for somatoform disorders? A critical review of previous intervention studies. Psychosom Med. 2007;69:889–900.
Van der Feltz-Cornelis CM, Van Oppen P, Ader HJ, Van Dyck R. Randomised controlled trial of a collaborative care model with psychiatric consultation for persistent medically unexplained symptoms in general practice. Psychother Psychosom. 2006;75:282–99.
Kant I, Jansen NW, Van Amelsvoort LG, Van Leusden R, Berkouwer A. Structured early consultation with the occupational health physician reduces sickness absence among office workers at high risk for long-term sickness absence: a randomized controlled trial. J Occup Rehabil. 2008;18:79–86.
Acknowledgments
This study was supported by a grant from the Aladdin Fund (project no. 1.9). We wish to thank Professor Jan Bolk, internist, for his helpful reading and advising on this manuscript. We thank also Eric van der Beek and Inge Speller for coordinating the study activities at the Achmea-Vitale sites and Jan-Willem van der Werff for his statistical support.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Hoedeman, R., Blankenstein, A.H., Krol, B. et al. The Contribution of High Levels of Somatic Symptom Severity to Sickness Absence Duration, Disability and Discharge. J Occup Rehabil 20, 264–273 (2010). https://doi.org/10.1007/s10926-010-9239-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-010-9239-3