Abstract
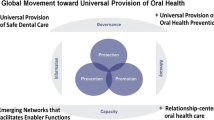
Oral health is a critical component to overall quality of life. Recommendations and guidelines for oral health continue to evolve while remaining underutilized worldwide. Still, oral healthcare parity and equity are achievable. This public health priority must be supported with stronger research, service delivery must be equitable and transparent, and the impact of oral healthcare must be fully understood. Data, surveillance, evidence and translation must be improved for oral health specialties as well as for greater global governance. Further, interdisciplinary coordination between orthodontic, dentistry, medical, biotechnology and research organizations must be prioritized. With dedication and consistent approach, oral healthcare can achieve the best outcomes for quality of life and cost effective public health.
Similar content being viewed by others
Abbreviations
- (CDC):
-
Centers for Disease Control and Prevention
- (FDI):
-
Fédération Dentaire Internationale
- (LMIC):
-
Low and Middle Income Countries
- (REALM):
-
Rapid Estimate of ADult Literacy in Medicine
- (TOFHLA):
-
Test of Functional Health Literacy in Adults
- (TOFHLiD):
-
The Test of Functional Literacy in Dentistry
- (WHO):
-
World Health Organization
References
World Health Organization, “Oral health.” [Online]. Available: http://www.who.int/oral_health/en/. [Accessed: 15-Apr-2018].
U.S. Department of Health and Human Services, “Oral Health,” 13-Apr-2018. [Online]. Available: https://www.healthypeople.gov/2020/topics-objectives/topic/oral-health/objectives. [Accessed: 15-Apr-2018].
Centers for Disease Control and Prevention, “Oral Health In America: Summary of the Surgeon General’s Report,” 19-Aug-2016. [Online]. Available: https://www.cdc.gov/oralhealth/publications/sgr2000_05.htm.
M. Glick, D. M. Williams, D. V. Kleinman, M. Vujicic, R. G. Watt, and R. J. Weyant, “A new definition for oral health developed by the FDI world dental federation opens the door to a universal definition of oral health,” J. Public Health Dent., vol. 77, no. 1, pp. 3–5, Dec. 2017.
J. A. Gil-Montoya, A. L. F. de Mello, R. Barrios, M. A. Gonzalez-Moles, and M. Bravo, “Oral health in the elderly patient and its impact on general well-being: A nonsystematic review,” Clin. Interv. Aging, vol. 10, pp. 461–467, Feb. 2015.
Lawrence, H. P., and Leake, J. L., The US surgeon General’s report on oral health in America: A Canadian perspective. J-Can Dent. Assoc 67(10):587–587, 2001.
S. S. Shueb, D. R. Nixdorf, M. T. John, B. F. Alonso, and J. Durham, “What is the impact of acute and chronic orofacial pain on quality of life?,” J. Dent., vol. 43, no. 10, pp. 1203–1210, Oct. 2015.
Hilgenberg-Sydney, P. B., Calles, B. M., and Conti, P. C. R., Quality of life in chronic trigeminal neuralgia patients. Rev. dor 16(3):195–197, 2015.
G. Almoznino et al., “Oral Health-Related Quality of Life in Patients with Temporomandibular Disorders,” J Oral Facial Pain Headache, vol. 29, no. 3, pp. 231–241, Summer 2015.
D. M. Saman, “A review of the epidemiology of oral and pharyngeal carcinoma: Update,” Head Neck Oncol., vol. 4, p. 1, Jan. 2012.
Global Oral cancer Form Group, “Understanding gaps in the oral cancer continuum and developing strategies to improve outcomes,” World Health Organization, 2016.
Scannapieco, F. A., and Harris, K. W., Oral Health and Pneumonia. In: Craig, R. G., Kamer, A. R. (Eds), A Clinician’s Guide to Systemic Effects of Periodontal Diseases. Berlin, Heidelberg: Springer Berlin Heidelberg, 2016, 81–92.
Klompas, M., Branson, R., Eichenwald, E. C., Greene, L. R., Howell, M. D., Lee, G., Magill, S. S., Maragakis, L. L., Priebe, G. P., Speck, K., Yokoe, D. S., Berenholtz, S. M., and Society for Healthcare Epidemiology of America (SHEA), Strategies to Prevent Ventilator-Associated Pneumonia in Acute Care Hospitals: 2014 Update. Infect. Control Hosp. Epidemiol. 35(8):915–936, 2014.
L. J. Jin, I. B. Lamster, J. S. Greenspan, N. B. Pitts, C. Scully, and S. Warnakulasuriya, “Global burden of oral diseases: Emerging concepts, management and interplay with systemic health,” Oral Dis., vol. 22, no. 7, pp. 609–619, Oct. 2016.
U. S. D. of Health, H. Services, and Others, “Integration of oral health and primary care practice,” Health Resources and Services Administration, 2014.
“Oral Health Services,” World Health Organization , 2018. [Online]. Available: http://www.who.int/oral_health/action/services/en/. [Accessed: 19-Apr-2018].
“Improving access to oral health care for vulnerable : HRSA,” National Academy of Sciences, 2011.
World Health Organization, “Density of dentistry personnel (total number per 1000 population, latest available year),” 2018. [Online]. Available: http://www.who.int/gho/health_workforce/dentistry_density_text/en/. [Accessed: 18-Apr-2018].
M. Masood, A. Sheiham, and E. Bernabé, “Household expenditure for dental care in low and middle income countries,” PLoS One, vol. 10, no. 4, p. e0123075, Apr. 2015.
E. Bernabé, M. Masood, and M. Vujicic, “The impact of out-of-pocket payments for dental care on household finances in low and middle income countries,” BMC Public Health, vol. 17, no. 1, p. 109, Jan. 2017.
S. Listl, J. Galloway, P. A. Mossey, and W. Marcenes, “Global economic impact of dental diseases,” J. Dent. Res., vol. 94, no. 10, pp. 1355–1361, Aug. 2015.
“Extent of Flouridation,” British Flouridation Society, 2012. [Online]. Available: https://docs.wixstatic.com/ugd/014a47_0776b576cf1c49308666cef7caae934e.pdf. [Accessed: 18-Apr-2018].
Petersen, P. E., and Ogawa, H., Prevention of dental caries through the use of fluoride – the WHO approach. Community Dental Health 35(1), 2016.
A. A. C. Heggie, “Oral and maxillofacial surgery: What are our credentials?,” Ann. Maxillofac. Surg., vol. 4, no. 1, p. 1, Jan. 2014.
Centers for Disease Prevention and Control, “Disparities in oral health,” 2018. [Online]. Available: https://www.cdc.gov/oralhealth/oral_health_disparities/index.htm. [Accessed: 19-Apr-2018].
M. Reza et al., “Oral health status of immigrant and refugee children in north america: a scoping review,” J. Can. Dent. Assoc., vol. 82, p. g3, Feb. 2016.
M. T. Keboa, N. Hiles, and M. E. Macdonald, “The oral health of refugees and asylum seekers: a scoping review,” Global. Health, vol. 12, no. 1, p. 59, Oct. 2016.
J. A. Shariff and B. L. Edelstein, “Medicaid meets its equal access requirement for dental care, but Oral health disparities remain,” Health Aff. , vol. 35, no. 12, pp. 2259–2267, Dec. 2016.
J. Steele et al., “The Interplay between socioeconomic inequalities and clinical oral health,” J. Dent. Res., vol. 94, no. 1, pp. 19–26, Jan. 2015.
N. Gupta et al., “Changing Trends in oral cancer - a global scenario,” Nepal J Epidemiol, vol. 6, no. 4, pp. 613–619, Dec. 2016.
K. D. Shield et al., “The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012: Lip, Oral Cavity, and Pharyngeal Cancers,” CA Cancer J. Clin., vol. 67, no. 1, pp. 51–64, Jan. 2017.
A. Taniguchi-Tabata et al., “Associations between dental knowledge, source of dental knowledge and oral health behavior in Japanese university students: A cross-sectional study,” PLoS One , vol. 12, no. 6, p. e0179298, Jun. 2017.
C.-C. Chen et al., “Immigrant-native differences in caries-related knowledge, attitude, and oral health behaviors: a cross-sectional study in Taiwan,” BMC Oral Health, vol. 14, no. 1, p. 3, Jan. 2014.
A. R. Wilson et al., “Validation and Impact of Caregivers’ Oral Health Knowledge and Behavior on Children's Oral Health Status,” Pediatr. Dent., vol. 38, no. 1, pp. 47–54, Jan. 2016.
V. Dickson-Swift, A. Kenny, J. Farmer, M. Gussy, and S. Larkins, “Measuring oral health literacy: A scoping review of existing tools,” BMC Oral Health, vol. 14, p. 148, Dec. 2014.
L. Stein, K. S. Pettersen, M. Bergdahl, and J. Bergdahl, “Development and validation of an instrument to assess oral health literacy in Norwegian adult dental patients,” Acta Odontol. Scand., vol. 73, no. 7, pp. 530–538, Feb. 2015.
I. S. Simpelaere, G. Van Nuffelen, J. Vanderwegen, K. Wouters, and M. De Bodt, “Oral health screening: Feasibility and reliability of the oral health assessment tool as used by speech pathologists,” Int. Dent. J., vol. 66, no. 3, pp. 178–189, Jun. 2016.
J. Rylands, D. Lowe, and S. N. Rogers, “Outcomes by area of residence deprivation in a cohort of oral cancer patients: Survival, health-related quality of life, and place of death,” Oral Oncol., vol. 52, pp. 30–36, Jan. 2016.
P. Speight, J. Epstein, O. Kujan, M. W. Lingen, T. Nagao, K. Ranganathan, P. Vargas “Screening for oral cancer – Who, what, why and where?,” World Health Organization, 2016.
D. R. Reissmann, A. Erler, C. Hirsch, I. Sierwald, C. Machuca, and O. Schierz, “Bias in retrospective assessment of perceived dental treatment effects when using the Oral health impact profile,” Qual. Life Res., vol. 27, no. 3, pp. 775–782, Mar. 2018.
D. J. Fischer, J. B. Epstein, Y. Yao, and D. J. Wilkie, “Oral health conditions affect functional and social activities of terminally ill cancer patients,” Support. Care Cancer, vol. 22, no. 3, pp. 803–810, Mar. 2014.
M. C. Carra, A. Schmitt, F. Thomas, N. Danchin, B. Pannier, and P. Bouchard, “Sleep disorders and oral health: A cross-sectional study,” Clin. Oral Investig., vol. 21, no. 4, pp. 975–983, May 2017.
Silvola, A.-S., Tolvanen, M., Rusanen, J., Sipilä, K., Lahti, S., and Pirttiniemi, P., Do changes in oral health-related quality-of-life, facial pain and temporomandibular disorders correlate after treatment of severe malocclusion? Acta Odontol. Scand. 74(1):44–50, 2016.
Y. Wang, D.-Y. Cao, B. Remeniuk, S. Krimmel, D. A. Seminowicz, and M. Zhang, “Altered brain structure and function associated with sensory and affective components of classic trigeminal neuralgia,” Pain, vol. 158, no. 8, pp. 1561–1570, Aug. 2017.
H. Shigeishi, M. Z. Rahman, K. Ohta, S. Ono, M. Sugiyama, and M. Takechi, “Professional oral health care reduces the duration of hospital stay in patients undergoing orthognathic surgery,” Biomed Rep, vol. 4, no. 1, pp. 55–58, Jan. 2016.
R. Sarkis-Onofre et al., “Use of guidelines to improve the quality and transparency of reporting oral health research,” J. Dent., vol. 43, no. 4, pp. 397–404, Apr. 2015.
M. C. Carra, F. Thomas, A. Schmitt, B. Pannier, N. Danchin, and P. Bouchard, “Oral health in patients treated by positive airway pressure for obstructive sleep apnea: A population-based case–control study,” Sleep and Breathing, vol. 20, no. 1, pp. 405–411, Mar. 2016.
Ajwani, S. et al., Integrated oral health care for stroke patients--a scoping review. J. Clin. Nurs. 26(7–8):891–901, 2017.
R. E. Long, M. Wilson-Genderson, B. H. Grayson, R. Flores, and H. L. Broder, “Oral health-related quality of life and self-rated speech in children with existing fistulas in mid-childhood and adolescence,” Cleft Palate Craniofac. J., 2015.
de Queiroz Herkrath, A. P. C., Herkrath, F. J., Rebelo, M. A. B., and Vettore, M. V., Measurement of health-related and oral health-related quality of life among individuals with nonsyndromic orofacial clefts: A systematic review and meta-analysis. Cleft Palate Craniofac. J. 52(2):157–172, 2015.
Smallridge, J. et al., Functional outcomes in the Cleft Care UK study--Part 3: oral health and audiology. Orthod. Craniofac. Res. 18(S2):25–35, 2015.
A. Maiya, Y. R. Shetty, K. Rai, V. Padmanabhan, and A. M. Hegde, “Use of different oral hygiene strategies in children with cerebral palsy: A comparative study,” J Int Soc Prev Community Dent, vol. 5, no. 5, pp. 389–393, Sep. 2015.
N. Sinha, B. Singh, K. G. Chhabra, and S. Patil, “Comparison of oral health status between children with cerebral palsy and normal children in India: A case-control study,” J. Indian Soc. Periodontol., vol. 19, no. 1, pp. 78–82, Jan. 2015.
Rodríguez, J. P. L. et al., Dental Decay and Oral Findings in Children and Adolescents Affected by Different Types of Cerebral Palsy: A Comparative Study. J. Clin. Pediatr. Dent. 42(1):62–66, 2018.
Availability of Data and Material
There is no original data to aggregate or report.
Funding
There are no funding contributions to declare.
Author information
Authors and Affiliations
Contributions
The author is the sole author of this manuscript.
Ethics declarations
Conflict of Interest
This author declares she has no conflict of interest This article does not contain any studies with human participants or animals performed by any of the authors There are no competing interests to declare Not applicable The author consents to publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Systems-Level Quality Improvement
Rights and permissions
About this article
Cite this article
Babyar, J. Inclusive Oral Healthcare for a better Future Together. J Med Syst 44, 89 (2020). https://doi.org/10.1007/s10916-020-01560-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-020-01560-3