Abstract
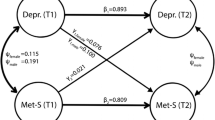
Arab Americans have high prevalences of metabolic syndrome (MetS) and depression. Depression and external locus of control (LOC) may worsen MetS. We examined the relationship between depression and MetS with a convenience sample of 136 Arab Americans living in the Washington, DC, metropolitan area. Participants were surveyed with the Multidimensional Health Locus of Control questionnaire and the Center of Epidemiological Studies-Depression scale. Laboratory measurements were collected based on the components of MetS. A structural equation model was used to explore the relationship between MetS and depression through analysis of LOC. MetS was significantly correlated with external LOC (powerful others and chance), and depression was correlated with a weak internal LOC. Future study of the effect of LOC on health outcomes in Arab Americans may be used to mitigate MetS and depression in this population.

Similar content being viewed by others
References
Shara N, Yassin SA, Abu-Bader S, et al. Overcoming recruitment challenges: a pilot study in Arab Americans. J Health Dispar Res Pract. 2016;9(4):30–40.
Aroian KJ, Katz A, Kulwicki A. Recruiting and retaining Arab Muslim mothers and children for research. J Nurs Scholarsh. 2006;38:255–61.
Jaber LA. Barriers and strategies for research in Arab Americans. Diabetes Care. 2003;26:514–5.
Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care. 2004;27:2444–9.
Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race, ethnicity, and body mass index: United States, 2003–2006. Hyattsville: National Health Statistics Reports; 2009.
Awad AI, Alsalah FM. 10-year risk estimation for type 2 diabetes mellitus and coronary heart disease in Kuwait: a cross-sectional population-based study. PloS ONE. doi:10.1371/journal.pone.0116742.
Sliem HA, Ahmed S, Nemr N, et al. Metabolic syndrome in the Middle East. Indian J Endocrinol Metab. 2012;16:67–71. doi:10.4103/2230-8210.91193.
Amer MM, Hovey JD. Socio-demographic differences in acculturation and mental health for a sample of 2nd generation/early immigrant Arab Americans. J Immigr Minor Health (London). 2007;9:335–47.
Jaber RM, Farroukh M, Ismael M, et al. Measuring depression and stigma towards depression and mental health treatment among adolescents in an Arab-American community. Int J Cult Ment Health. 2015;8:247–54.
Kira IA, Wrobel NH. Trauma: stress, coping, and emerging treatment models. In: Amer MM, Awad GH, editors. Handbook of Arab American psychology. New York, NY: Taylor & Francis; 2016
Abu-Bader SH, Tirmazi MT, Ross-Sheriff F. The impact of acculturation on depression among older Muslim immigrants in the United States. Gerontol Soc Work. 2001;54:425–48. doi:10.1080/01634372.2011.560928.
Ahmed SR, Kia-Keating M, Tsai KH. A structural model of racial discrimination, acculturative stress, and cultural resources among Arab American adolescents. Am J Community Psychol. 2011;48:181–92. doi:10.1007/s10464-011-9424-3.
Clay RA. Muslims in America, post 9/11. Am Psychol Assoc. 2011;428:72.
Zawawi JA, Hamaideh SH. Depressive symptoms and their correlates with locus of control and satisfaction with life among Jordanian college students. Eur J Psychol. 2009;4:71–103.
Afifi M. Health locus of control and depressive symptoms among adolescents in Alexandria, Egypt. East Mediterr Health J. 2007;13:1043–50.
Cohen M, Azaiza F. Health-promoting behaviors and health locus of control from a multicultural perspective. Ethn Dis. 2007;17:636–42.
Alexander CM, Landsman PB, Teutsch SM, et al. NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes. 2003;52:1210–4.
Hildrum B, Mykletun A, Hole T, et al. Age-specific prevalence of the metabolic syndrome defined by the International Diabetes Federation and the National Cholesterol Education Program: the Norwegian HUNT 2 Study. BMC Public Health. 2007;7:220. doi:10.1186/1471-2458-7-220.
Shin JA, Lee JH, Lim SY, et al. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. Diabetes Investig. 2013;4:334–43.
Wannamethee SG, Shaper AG, Lennon L, et al. Metabolic syndrome vs. Framingham risk score for prediction of coronary heart disease, stroke, and type 2 diabetes. Arch Intern Med. 2005;165:2644–50.
Boyko EJ, Doheny RA, McNeely MJ, et al. Latent class analysis of the metabolic syndrome. Diabetes Res Con Pract. 2010;89:88–93. doi:10.1016/j.diabres.2010.02.013.
Beltran-Sanchez H, Harhay MO, Harhay MM, et al. Prevalence and trends of metabolic syndrome in the adult U.S. population, 1999–2010. J Am Coll Cardiol. 2013;62:697–703.
Jaber LA, Brown MB, Adnan H, et al. The prevalence of the metabolic syndrome among Arab Americans. Diabetes Care. 2004;27:234–8.
Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi:10.1001/archpysc.62.6.593.
Kahl KG, Schwiger U, Correll C, et al. Depression, anxiety disorders, and metabolic syndrome in a population at risk for type 2 diabetes mellitus. Brain Behavior. 2015. doi:10.1002/brb3.306.
El-Sayid AM, Galea S. The health of Arab-Americans living the United States: a systematic review of the literature. BMC Public Health 2009;9:272.
Amer M, Awad GH, Hovey JD. Evaluation of the CES-D Scale factor structure in a sample of second-generation Arab-Americans. Int J Culture Mental Health. 2012;7:46–58.
Moise N, Khodneva Y, Richman J, et al. Elucidating the association between depressive symptoms, coronary heart disease, and stroke in black and white adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. J Am Heart Assoc. 2016. doi:10.1161/JAHA.116.003767.
Block A, Schipf S, Van der Auwera S, et al. Sex- and age-specific associations between major depressive disorder and metabolic syndrome in two general population samples in Germany. Nord J Psychiatry. 2016;14:1–10.
Heiskanen T, Niskanen LK, Hintikka JJ, et al. Metabolic syndrome and depression: a cross-sectional analysis. J Clin Psychiatry. 2006;67:1422–7.
Dunbar JA, Reddy P, Davis-Lameloise N, et al. Depression: an important comorbidity with metabolic syndrome in a general population. Diabetes Care. 2008;31:2368–73.
Pan A, Keum N, Okereke OI, et al. Bidirectional association between depression and metabolic syndrome. Diabetes Care. 2012;35:1171–80.
Foley DL, Morley KI, Madden PAF, et al. Major depression and the metabolic syndrome. Twin Res Hum Genet. 2010;1:347–58. doi:10.1375/twin.13.4.347.
Kinder LS, Carnethon MR, Palaniappan LP, et al. Depression and the metabolic syndrome in young adults: findings from the Third National Health and Nutrition Examination Survey. Psychosom Med. 2004;66:316–22.
Wallston KA, Wallston BS, DeVellis R. Development of the multidimensional health locus of control (MHCL) scales. Health Educ Monogr. 1978;6:160–70.
Eaton WW, Muntaner C, Smith C, et al. Center for epidemiological studies depression scale: review and revision (CESD and CESD-R). In: Mariush ME, editor. The use of psychological testing for treatment planning and outcomes assessment, 3rd ed. Mahwah NJ: Lawrence Eribaum; 2004. pp. 363–77.
Ghubash R, Daradkeh T, Al Naseri K, Bin al Bloushi N, Al Daheri A. The performance of the center of epidemiologic study depression scale (CES-D) in an Arab female community. Int J Soc Psychiatry. 2000;46:241–9.
Parikh RM, Mohan V. Changing definitions of metabolic syndrome. Indian J Endocrinol Metab. 2012;16:7–12. doi:10.4103/2230-8210.91175.
Borsboom D. Latent variable theory. Meas Interdiscip Res Perspect. 2008;6:25–53.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016. https://www.R-project.org/.
Fox J, Nie Z, Byrnes J. Sem: structural equation models. R package version 3.1–9. https://CRAN.R-project.org/package=sem (2017)
Galanos AN, Strauss RP, Pieper CF. Sociodemographic correlates of health beliefs among Black and White community dwelling elderly individuals. Int J Aging Hum Dev. 1994;38:339–50.
Grotz m, Kapke U, Lampert T, Baumeister H. Health locus of control and health behavior: results from a nationally representative survey. Psychol Health Med. 2011;16:129–40. doi:10.1080/13548506.2010.521570.
Janowski K, Kurpas D, Kusz J, Mroczek B, Jedynak T. Health-related behavior, profile of health locus of control and acceptance of illness in patients suffering from chronic somatic diseases. PLoS ONE 2013;8:e63920. doi:10.1371/journal.pone.0063920.
Lundren S, Eurenius E, Olausson A, et al. The Swedish version of the multidimensional health locus of control scales, form C. Aspects of reliability and validity in patients with rheumatoid arthritis. Adv Physiotherapy. 2007;9:16–22.
Egan JT, Leonardson G, Best LG, et al. Multidimensional health locus of control in American Indians: the Strong Heart Study. Ethn Dis. 2009;19:338–44.
Keedy NH. Health locus of control, self-efficancy, and multidisciplinary intervention for chronic back pain (doctoral dissertation). Retrieved from Iowa research online: The University of Iowa’s Institutional Repository; 2009.
Norman P, Bennet P, Smith C, et al. Health locus of control and health behaviours. J Health Psychol. 1998;3:171–80.
Acknowledgements
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR001409. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Rachel Schaperow, MedStar Health Research Institute, for editing the manuscript.
Funding
This research was funded by the National Center for Advancing Translational Sciences of the National Institutes of Health (Award Number UL1TR001409).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shara, N.M., Zeymo, A., Abudiab, Z. et al. Depression, Metabolic Syndrome, and Locus of Control in Arab Americans Living in the DC Metropolitan Area: A Structural Equation Model. J Immigrant Minority Health 20, 902–908 (2018). https://doi.org/10.1007/s10903-017-0626-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-017-0626-0