Abstract
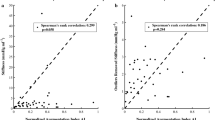
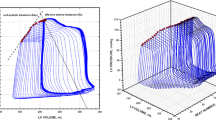
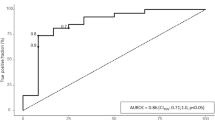
To compare the effective arterial elastance (Ea) obtained from the arterial pressure with Ea calculated from left-ventricular (LV) pressure–volume analysis. Experimental study. LV pressure–volume data was obtained with a conductance catheter and arterial pressures were measured via a fluid-filled catheter placed in the proximal aorta, femoral and radial arteries. Ea was calculated as LV end-systolic pressure (ESP)/stroke volume (SV). Experimental protocol consisted sequentially changing afterload (phenylephrine/nitroprusside), preload (bleeding/fluid), and contractility (esmolol/dobutamine). 90% of systolic pressure (Eaao_SYS, Eafem_SYS, Earad_SYS), mean arterial pressure (Eaao_MAP, Eafem_MAP, Earad_MAP), and dicrotic notch pressure (Eaao_DIC, Eafem_DIC, Earad_DIC) were used as surrogates for LV ESP. SV was calculated from the LV pressure–volume data. When Ea was compared with estimations based on 90% SAP, the relationship was r2 = 0.95, 0.94 and 0.92; and the bias and limits of agreement (LOA): − 0.01 ± 0.12, − 0.09 ± 0.12, − 0.05 ± 0.15 mmHg ml−1, for Eaao_SYS, Eafem_SYS and Earad_SYS, respectively. For estimates using dicrotic notch, the relationship was r2 = 0.94, 0.95 and 0.94 for Eaao_DIC, Eafem_DIC and Earad_DIC, respectively; with a bias and LOA: 0.05 ± 0.11, 0.06 ± 0.12, 0.10 ± 0.12 mmHg ml−1, respectively. When Ea was compared with estimates using MAP, the relationship was r2 = 0.95, 0.96 and 0.95 for Eaao_MAP, Eafem_MAP and Earad_MAP, respectively; with a bias and LOA: 0.05 ± 0.11, 0.06 ± 0.11, 0.06 ± 0.11 mmHg ml−1, respectively. LV ESP can be estimated from the arterial pressure. Provided that the SV measurement is reliable, the ratio MAP/SV provides a robust Ea surrogate over a wide range of hemodynamic conditions and is interchangeably in any peripheral artery, so it should be recommended as an arterial estimate of Ea in further research.






Similar content being viewed by others
References
Monge Garcia MI, Guijo Gonzalez P, Gracia Romero M, Gil Cano A, Oscier C, Rhodes A, Grounds RM, Cecconi M. Effects of fluid administration on arterial load in septic shock patients. Intensive Care Med. 2015;41(7):1247–55. https://doi.org/10.1007/s00134-015-3898-7.
Monge Garcia MI, Romero MG, Cano AG, Rhodes A, Grounds RM, Cecconi M. Impact of arterial load on the agreement between pulse pressure analysis and esophageal Doppler. Crit Care. 2013;17(3):R113. https://doi.org/10.1186/cc12785.
Monge Garcia MI, Saludes Orduna P, Cecconi M. Understanding arterial load. Intensive Care Med. 2016;42(10):1625–7. https://doi.org/10.1007/s00134-016-4212-z.
Guarracino F, Baldassarri R, Pinsky MR. Ventriculo-arterial decoupling in acutely altered hemodynamic states. Crit Care. 2013;17(2):213. https://doi.org/10.1186/cc12522.
Guarracino F, Ferro B, Morelli A, Bertini P, Baldassarri R, Pinsky MR. Ventriculoarterial decoupling in human septic shock. Crit Care. 2014;18(2):R80. https://doi.org/10.1186/cc13842.
Morelli A, Singer M, Ranieri VM, D’Egidio A, Mascia L, Orecchioni A, Piscioneri F, Guarracino F, Greco E, Peruzzi M, Biondi-Zoccai G, Frati G, Romano SM. Heart rate reduction with esmolol is associated with improved arterial elastance in patients with septic shock: a prospective observational study. Intensive Care Med. 2016;42(10):1528–34. https://doi.org/10.1007/s00134-016-4351-2.
Monge Garcia MI, Guijo Gonzalez P, Gracia Romero M, Gil Cano A, Rhodes A, Grounds RM, Cecconi M. Effects of arterial load variations on dynamic arterial elastance: an experimental study. Br J Anaesth. 2017;118(6):938–46. https://doi.org/10.1093/bja/aex070.
Guinot PG, Longrois D, Kamel S, Lorne E, Dupont H. Ventriculo-arterial coupling analysis predicts the hemodynamic response to norepinephrine in hypotensive postoperative patients: a prospective observational study. Crit Care Med. 2018;46(1):e17–25. https://doi.org/10.1097/CCM.0000000000002772.
Suga H. Theoretical analysis of a left-ventricular pumping model based on the systolic time-varying pressure–volume ratio. IEEE Trans Biomed Eng. 1971;18(1):47–55.
Sunagawa K, Maughan WL, Burkhoff D, Sagawa K. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol. 1983;245(5 Pt 1):H773–80.
Frank O. Die Grundform des Arteriellen Pulses. Z Biol. 1899;37:483–526.
Westerhof N, Elzinga G, Sipkema P. An artificial arterial system for pumping hearts. J Appl Physiol. 1971;31(5):776–81. https://doi.org/10.1152/jappl.1971.31.5.776.
Stergiopulos N, Westerhof BE, Westerhof N. Total arterial inertance as the fourth element of the windkessel model. Am J Physiol. 1999;276(1 Pt 2):H81–8.
Murgo JP, Westerhof N, Giolma JP, Altobelli SA. Aortic input impedance in normal man: relationship to pressure wave forms. Circulation. 1980;62(1):105–16.
Grossman W, Braunwald E, Mann T, McLaurin LP, Green LH. Contractile state of the left ventricle in man as evaluated from end-systolic pressure–volume relations. Circulation. 1977;56(5):845–52.
Colin P, Slama M, Vahanian A, Lecarpentier Y, Motte G, Chemla D. Hemodynamic correlates of effective arterial elastance in mitral stenosis before and after balloon valvotomy. J Appl Physiol (1985). 1997;83(4):1083–9. https://doi.org/10.1152/jappl.1997.83.4.1083.
Kelly RP, Ting CT, Yang TM, Liu CP, Maughan WL, Chang MS, Kass DA. Effective arterial elastance as index of arterial vascular load in humans. Circulation. 1992;86(2):513–21.
Chemla D, Antony I, Lecarpentier Y, Nitenberg A. Contribution of systemic vascular resistance and total arterial compliance to effective arterial elastance in humans. Am J Physiol Heart Circ Physiol. 2003;285(2):H614–20. https://doi.org/10.1152/ajpheart.00823.2002.
Nichols WW, O’Rourke M. McDonald’s blood flow in arteries: theoretical, experimental and clinical principles. McDonald’s blood flow in arteries: theoretical, experimental and clinical principles. 5th ed. London: Oxford University Press; 2005.
Morelli A, Sanfilippo F, Romano SM. Esmolol in septic shock: old pathophysiological concepts, an old drug, perhaps a new hemodynamic strategy in the right patient. J Thorac Dis. 2016;8(11):3059–62. https://doi.org/10.21037/jtd.2016.11.111.
McLean AS, Taccone FS, Vieillard-Baron A. Beta-blockers in septic shock to optimize hemodynamics? No. Intensive Care Med. 2016;42(10):1610–2. https://doi.org/10.1007/s00134-016-4407-3.
Kass DA, Yamazaki T, Burkhoff D, Maughan WL, Sagawa K. Determination of left ventricular end-systolic pressure–volume relationships by the conductance (volume) catheter technique. Circulation. 1986;73(3):586–95.
Baan J, van der Velde ET, de Bruin HG, Smeenk GJ, Koops J, van Dijk AD, Temmerman D, Senden J, Buis B. Continuous measurement of left ventricular volume in animals and humans by conductance catheter. Circulation. 1984;70(5):812–23.
Kono A, Maughan WL, Sunagawa K, Hamilton K, Sagawa K, Weisfeldt ML. The use of left ventricular end-ejection pressure and peak pressure in the estimation of the end-systolic pressure–volume relationship. Circulation. 1984;70(6):1057–65.
Hatib F, Roteliuk L. (2014) Detection of parameters in cardiac output related waveforms. United States Patent US12699540, 2010-02-03.
Segers P, Stergiopulos N, Westerhof N. Relation of effective arterial elastance to arterial system properties. Am J Physiol Heart Circ Physiol. 2002;282(3):H1041–6. https://doi.org/10.1152/ajpheart.00764.2001.
Sunagawa K, Maughan WL, Sagawa K. Optimal arterial resistance for the maximal stroke work studied in isolated canine left ventricle. Circ Res. 1985;56(4):586–95.
Pauca AL, Wallenhaupt SL, Kon ND, Tucker WY. Does radial artery pressure accurately reflect aortic pressure? Chest. 1992;102(4):1193–8.
Chen CH, Nakayama M, Talbot M, Nevo E, Fetics B, Gerstenblith G, Becker LC, Kass DA. Verapamil acutely reduces ventricular-vascular stiffening and improves aerobic exercise performance in elderly individuals. J Am Coll Cardiol. 1999;33(6):1602–9.
Dahlgren G, Veintemilla F, Settergren G, Liska J. Left ventricular end-systolic pressure estimated from measurements in a peripheral artery. J Cardiothorac Vasc Anesth. 1991;5(6):551–3.
Hatib F, Jansen JR, Pinsky MR. Peripheral vascular decoupling in porcine endotoxic shock. J Appl Physiol. 2011;111(3):853–60. https://doi.org/10.1152/japplphysiol.00066.2011.
Monge Garcia MI, Santos A, Diez Del Corral B, Guijo Gonzalez P, Gracia Romero M, Gil Cano A, Cecconi M. Noradrenaline modifies arterial reflection phenomena and left ventricular efficiency in septic shock patients: A prospective observational study. J Crit Care. 2018;47:280–6. https://doi.org/10.1016/j.jcrc.2018.07.027.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2016. Intensive Care Med. 2017;43(3):304–77. https://doi.org/10.1007/s00134-017-4683-6.
Nirmalan M, Dark PM. Broader applications of arterial pressure wave form analysis. Contin Educ Anaesth Crit Care Pain. 2014;14(6):285–90. https://doi.org/10.1093/bjaceaccp/mkt078.
Asanoi H, Sasayama S, Kameyama T. Ventriculoarterial coupling in normal and failing heart in humans. Circ Res. 1989;65(2):483–93.
Hoeksel SA, Jansen JR, Blom JA, Schreuder JJ. Detection of dicrotic notch in arterial pressure signals. J Clin Monit. 1997;13(5):309–16.
Chantler PD, Lakatta EG. Arterial-ventricular coupling with aging and disease. Front Physiol. 2012;3:90. https://doi.org/10.3389/fphys.2012.00090.
Kelly R, Fitchett D. Noninvasive determination of aortic input impedance and external left ventricular power output: a validation and repeatability study of a new technique. J Am Coll Cardiol. 1992;20(4):952–63.
Acknowledgements
We are grateful to all laboratory staff of the Edwards Research Center for their help in this work.
Funding
Edwards Lifesciences provided the software, hardware, and animals for the study.
Author information
Authors and Affiliations
Contributions
Study conception: MIMG, MRP and MC. Study design: MIMG, ZJ, MRP. Performed experimental research: MIMG, ZJ, FH. Analyzed and interpreted the data: MIMG, ZJ, MRP, FH. Drafted the manuscript: MIMG, ZJ, JJS and FH. All authors reviewed it, contributed significantly to its critical review, and approved the final version of the manuscript. All authors ensure the accuracy or integrity of the results of this study and will be accountable for any question related with this work.
Corresponding author
Ethics declarations
Conflict of interest
MIMG is a consultant to Edwards Lifesciences and received honoraria and/or travel expenses from Deltex Medical. MRP is a consultant to Edwards LifeSciences, LiDCO Ltd., and Cheetah. MC has received honoraria and/or travel expenses from Edwards Lifesciences, LiDCO, Cheetah, Bmeye, Masimo and Deltex Medical. ZJ, JJS, and FH are Edwards Lifesciences employees.
Ethical approval
The study was approved for the use of Yorkshire crossbred pigs by the Institutional Animal Care and Use Committee (IACUC) at the Edwards Research Center, and all experimentation was performed in accordance with the USDA Animal Welfare Act regulations (AWArs), and the Guide for the Care and Use of Laboratory Animals (ILAR, NAP, Washington, DC, 2010, 8th edition). The Test Facility is accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care, International (AAALACi) and registered with the United States Department of Agriculture to conduct research with laboratory animals. The ARRIVE guidelines were used for the elaboration of this manuscript.
Rights and permissions
About this article
Cite this article
Monge Garcia, M.I., Jian, Z., Settels, J.J. et al. Reliability of effective arterial elastance using peripheral arterial pressure as surrogate for left ventricular end-systolic pressure. J Clin Monit Comput 33, 803–813 (2019). https://doi.org/10.1007/s10877-018-0236-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0236-y