Abstract
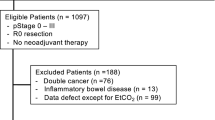
The relationship between muscular tissue oxygen saturation (SmtO2) during surgery and postoperative nausea and vomiting (PONV) remains to be determined. Patients undergoing robotic hysterectomy participated in this prospective cohort study. SmtO2 of the brachioradialis muscle in the forearm was continuously monitored during surgery. Thresholds based on relative changes or absolute values were systematically assigned. The relationship between thresholds and PONV was investigated based on threshold analysis (i.e., exceeding or not exceeding a threshold), area under the curve analysis (i.e., the size of the area enclosed by the SmtO2 trace and threshold), and multivariable analysis by accounting for recognized PONV risk factors. PONV occurred in 35 of 106 patients (33%). Based on the multivariable analysis, the SmtO2 threshold of 20% above baseline correlated with less PONV (OR 0.39; 95% CI 0.16–0.93; p = 0.034), and the following values correlated with more PONV: 5% below baseline (OR 2.37; 95% CI 1.26–4.45; p = 0.007), 20% below baseline (OR 16.08; 95% CI 3.05–84.73; p = 0.001), < 70% (OR 2.86; 95% CI 1.17–6.99; p = 0.021) and < 60% (OR 6.55; 95% CI 1.11–38.53; p = 0.038). Our study suggests that a potential therapeutic goal for PONV prophylaxis may be to maintain SmtO2 at > 70% and above baseline.




Similar content being viewed by others
References
Kovac AL. Prevention and treatment of postoperative nausea and vomiting. Drugs. 2000;59:213–43.
Wang J, Ho S, Liu H, Ho C. Prophylactic antiemetic effect of dexamethasone in women undergoing ambulatory laparoscopic surgery. Br J Anaesth. 2000;84:459–62.
Geng ZY, Liu YF, Wang SS, Wang DX. Intra-operative dexmedetomidine reduces early postoperative nausea but not vomiting in adult patients after gynaecological laparoscopic surgery: a randomised controlled trial. Eur J Anaesthesiol. 2016;33:761–6.
Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA, Watcha M, Chung F, Angus S, Apfel CC, Bergese SD, Candiotti KA, Chan MT, Davis PJ, Hooper VD, Lagoo-Deenadayalan S, Myles P, Nezat G, Philip BK, Tramer MR. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118:85–113.
Gan T, Mythen M. Does peroperative gut-mucosa hypoperfusion cause postoperative nausea and vomiting? The Lancet. 1995;345:1123–4.
Meng L, Cannesson M, Alexander BS, Yu Z, Kain ZN, Cerussi AE, Tromberg BJ, Mantulin WW. Effect of phenylephrine and ephedrine bolus treatment on cerebral oxygenation in anaesthetized patients. Br J Anaesth. 2011;107:209–17.
Meng L, Gelb AW, Alexander BS, Cerussi AE, Tromberg BJ, Yu Z, Mantulin WW. Impact of phenylephrine administration on cerebral tissue oxygen saturation and blood volume is modulated by carbon dioxide in anaesthetized patients. Br J Anaesth. 2012;108:815–22.
Benni PB, MacLeod D, Ikeda K, Lin H-M. A validation method for near-infrared spectroscopy based tissue oximeters for cerebral and somatic tissue oxygen saturation measurements. J Clin Monit Comput. 2018;32:269–84.
Meng L, Xiao J, Gudelunas K, Yu Z, Zhong Z, Hu X. Association of intraoperative cerebral and muscular tissue oxygen saturation with postoperative complications and length of hospital stay after major spine surgery: an observational study. Br J Anaesth. 2017;118:551–62.
Simpson KM, Advincula AP. The essential elements of a robotic-assisted laparoscopic hysterectomy. Obstet Gynecol Clin N Am. 2016;43:479–93.
Magner JJ, McCaul C, Carton E, Gardiner J, Buggy D. Effect of intraoperative intravenous crystalloid infusion on postoperative nausea and vomiting after gynaecological laparoscopy: comparison of 30 and 10 ml kg(-1). Br J Anaesth. 2004;93:381–5.
Pusch F, Berger A, Wildling E, Tiefenthaler W, Krafft P. The effects of systolic arterial blood pressure variations on postoperative nausea and vomiting. Anesth Analg. 2002;94:1652–5.
Mythen MG, Webb AR. Perioperative plasma volume expansion reduces the incidence of gut mucosal hypoperfusion during cardiac surgery. Arch Surg. 1995;130:423–9.
Goll V, Akça O, Greif R, Freitag H, Arkiliç CF, Scheck T, Zoeggeler A, Kurz A, Krieger G, Lenhardt R. Ondansetron is no more effective than supplemental intraoperative oxygen for prevention of postoperative nausea and vomiting. Anesth Analg. 2001;92:112–7.
Greif R, Laciny S, Rapf B, Hickle RS, Sessler DI. Supplemental oxygen reduces the incidence of postoperative nausea and vomiting. Anesthesiology. 1999;91:1246–52.
Orhan-Sungur M, Kranke P, Sessler D, Apfel CC. Does supplemental oxygen reduce postoperative nausea and vomiting? A meta-analysis of randomized controlled trials. Anesth Analg. 2008;106:1733–8.
Aiello LC, Wheeler P. The expensive-tissue hypothesis: the brain and the digestive system in human and primate evolution. Curr Anthropol. 1995;36:199–221.
Johnson PC. Autoregulation of intestinal blood flow. Am J Physiol–Legacy Content. 1960;199:311–8.
Kiel J, Riedel G, Shepherd A. Autoregulation of canine gastric mucosal blood flow. Gastroenterology. 1987;93:12–20.
Kvietys PR, Miller T, Granger DN. Intrinsic control of colonic blood flow and oxygenation. Am J Physiol Gastrointest Liver Physiol. 1980;238:G478-G84.
Beuk RJ, Heineman E, Tangelder G-J, Kurvers HA, Bonke H-J, oude Egbrink MG. Effects of different durations of total warm ischemia of the gut on rat mesenteric microcirculation. J Surg Res. 1997;73:14–23.
Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg. 1993;76:1067–71.
Fukuyama K, Iwakiri R, Noda T, Kojima M, Utsumi H, Tsunada S, Sakata H, Ootani A, Fujimoto K. Apoptosis induced by ischemia–reperfusion and fasting in gastric mucosa compared to small intestinal mucosa in rats. Dig Dis Sci. 2001;46:545–9.
Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. Acute mesenteric ischemia: a clinical review. Arch Intern Med. 2004;164:1054–62.
Türler A, Moore BA, Pezzone MA, Overhaus M, Kalff JC, Bauer AJ. Colonic postoperative inflammatory ileus in the rat. Ann Surg. 2002;236:56–66.
Murkin J, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103:i3–13.
Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surgery Forum. 2003: E376–81.
Colak Z, Borojevic M, Bogovic A, Ivancan V, Biocina B, Majeric-Kogler V. Influence of intraoperative cerebral oximetry monitoring on neurocognitive function after coronary artery bypass surgery: a randomized, prospective study. Eur J Cardiothorac Surg. 2015;47:447–54.
Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM, Rodriguez AL, Magovern CJ, Zaubler T, Freundlich K. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thoracic Surg. 2009;87:36–45.
Meng L, Gruenbaum SE, Dai F, Wang T. Physiology, intervention, and outcome: three critical questions about cerebral tissue oxygen saturation monitoring. Minerva Anestesiol 2018;84:599–614.
Hyttel-Sorensen S, Hessel TW, Greisen G. Peripheral tissue oximetry: comparing three commercial near-infrared spectroscopy oximeters on the forearm. J Clin Monit Comput. 2014;28:149–55.
Sørensen H, Thomsen J, Meyer A, Terzic D, Hilsted L, Kjærgaard J, Goetze J, Barbosa T, Secher N. Phenylephrine increases near-infrared spectroscopy determined muscle oxygenation in men. J Clin Monit Comput. 2016:1–8.
Scheeren TWL, Saugel B. Journal of clinical monitoring and computing 2016 end of year summary: monitoring cerebral oxygenation and autoregulation. J Clin Monit Comput. 2017;31:241–6.
Acknowledgements
We thank CAS Medical Systems, Inc., Branford, CT, USA, for providing the FORE-SIGHT ELITE Tissue Oximeter at no cost.
Funding
Support provided from institutional and/or departmental sources at Yale University and Peking University.
Author information
Authors and Affiliations
Contributions
GL contributed to the study design and the interpretation and acquisition of the data. LL contributed to the study design and acquisition of the data. FD contributed to analysis and interpretation of the data. XG contributed to the interpretation of the data. LM contributed to the study design and the acquisition and interpretation of the data. All authors were involved in the writing and revising of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
LM is a consultant to CAS Medical Systems, Inc. The other authors declare no conflicts of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, G., Lin, L., Dai, F. et al. Muscular tissue oxygen saturation during robotic hysterectomy and postoperative nausea and vomiting: exploring the potential therapeutic thresholds. J Clin Monit Comput 33, 597–604 (2019). https://doi.org/10.1007/s10877-018-0193-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0193-5