Abstract
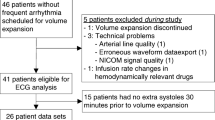
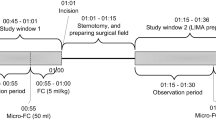
Fluid responsiveness prediction is an unsettled matter for most critical care patients and new methods relying only on the continuous basic monitoring are desired. It was hypothesized that the post-ectopic beat, which is associated with increased preload, could be analyzed in relation to preceding sinus beats and that the change in cardiac performance (e.g. systolic blood pressure) at the post-ectopic beat could predict fluid responsiveness. Cardiothoracic critical care patients scheduled for a 500 ml volume expansion were observed. In the 30 min prior to volume expansion, the ECG was analyzed for occurrence of extra systoles preceded by at least 10 sinus beats. Classification variables, were defined as the change in a variable (e.g. systolic blood pressure or pre-ejection period) from the median of 10 preceding sinus beats to extra systolic post-ectopic beat. A stroke volume increase >15 % following volume expansion defined fluid responsiveness. Thirty patients were included. The change in systolic blood pressure predicted fluid responsiveness in 24 patients correctly with 83 % specificity and 75 % sensitivity (optimal threshold: 5 % systolic blood pressure increase), receiver operating characteristic (ROC) area: 0.81 (CI [0.64;0.98]). The change in pre-ejection period predicted fluid responsiveness in 22 patients correctly with 67 % specificity and 83 % sensitivity (optimal threshold: 19 ms pre-ejection period decrease), ROC area: 0.81 (CI [0.66;0.96]). Pulse pressure variation had ROC area of 0.57 (CI [0.39;0.75]). Based on standard critical care monitoring, analysis of the extra systolic post-ectopic beat predicts fluid responsiveness in cardiothoracic critical care patients with good accuracy.



Similar content being viewed by others
References
Hoste EA, Maitland K, Brudney CS, Mehta R, Vincent JL, Yates D, Kellum JA, Mythen MG, Shaw AD. ADQI XII Investigators Group. Four phases of intravenous fluid therapy: a conceptual model. Br J Anaesth. 2014;113(5):740–7.
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41(7):1774–81.
Michard F. Changes in arterial pressure during mechanical ventilation. Anesthesiology. 2005;103(2):419–28.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37:2642–47.
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162(1):134–8.
Mahjoub Y, Lejeune V, Muller L, Perbet S, Zieleskiewicz L, Bart F, Veber B, Paugam-Burtz C, Jaber S, Ayham A, Zogheib E, Lasocki S, Vieillard-Baron A, Quintard H, Joannes-Boyau O, Plantefeve G, Montravers P, Duperret S, Lakhdari M, Ammenouche N, Lorne E, Slama M, Dupont H. Evaluation of pulse pressure variation validity criteria in critically ill patients: a prospective observational multicentre point-prevalence study. Br J Anaesth. 2014;112:681–5.
Hennings LI, Haase N, Pedersen UG, Perner A. Arterial waveform-analysis is of limited value in daily clinical practice in the intensive care unit. Danish Med J. 2015;62(9):A5136.
Schultz MJ, Haitsma JJ, Slutsky AS, Gajic O. What tidal volumes should be used in patients without acute lung injury? Anesthesiology. 2007;106(6):1226–31.
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL. Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med. 2005;31(4):517–23.
Lansdorp B, Lemson J, van Putten MJ, de Keijzer A, van der Hoeven JG, Pickkers P. Dynamic indices do not predict volume responsiveness in routine clinical practice. Br J Anaesth. 2012;108(3):395–401.
Strom T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet. 2010;375(9713):475–80.
Marik PE, Monnet X, Teboul JL. Hemodynamic parameters to guide fluid therapy. Ann Intensive Care. 2011;1(1):15820-1-1.
Cavallaro F, Sandroni C, Marano C, La Torre G, Mannocci A, De Waure C, Bello G, Maviglia R, Antonelli M. Diagnostic accuracy of passive leg raising for prediction of fluid responsiveness in adults: systematic review and meta-analysis of clinical studies. Intensive Care Med. 2010;36(9):1475–83.
Takada H, Takeuchi S, Ando K, Kaito A, Yoshida S. Experimental studies on myocardial contractility and hemodynamics in extrasystoles. Jpn Circ J. 1970;34(5):419–30.
Yellin EL, Kennish A, Yoran C, Laniado S, Buckley NM, Frater RW. The influence of left ventricular filling on postextrasystolic potentiation in the dog heart. Circ Res. 1979;44(5):712–22.
Vistisen ST, Andersen KK, Frederiksen CA, Kirkegaard H. Variations in the pre-ejection period induced by ventricular extra systoles may be feasible to predict fluid responsiveness. J Clin Monit Comput. 2014;28(4):341–9.
Vistisen ST, Koefoed-Nielsen J, Larsson A. Automated pre-ejection period variation predicts fluid responsiveness in low tidal volume ventilated pigs. Acta Anaesthesiol Scand. 2010;54(2):199–205.
Vistisen ST, Struijk JJ, Larsson A. Automated pre-ejection period variation indexed to tidal volume predicts fluid responsiveness after cardiac surgery. Acta Anaesthesiol Scand. 2009;53(4):534–42.
Feissel M, Badie J, Merlani PG, Faller JP, Bendjelid K. Pre-ejection period variations predict the fluid responsiveness of septic ventilated patients. Crit Care Med. 2005;33(11):2534–9.
De Backer D, Taccone FS, Holsten R, Ibrahimi F, Vincent JL. Influence of respiratory rate on stroke volume variation in mechanically ventilated patients. Anesthesiology. 2009;110(5):1092–7.
Vistisen ST, Koefoed-Nielsen J, Larsson A. Should dynamic parameters for prediction of fluid responsiveness be indexed to the tidal volume? Acta Anaesthesiol Scand. 2010;54(2):191–8.
Manolio TA, Furberg CD, Rautaharju PM, Siscovick D, Newman AB, Borhani NO, Gardin JM, Tabatznik B. Cardiac arrhythmias on 24-h ambulatory electrocardiography in older women and men: the cardiovascular health study. J Am Coll Cardiol. 1994;23(4):916–25.
Acknowledgments
This study has been financially supported by The Danish Independent Medical Research Council (DFF—4183-00540).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The extra systoles method has been protected by an international patent application by Aarhus University (PCT/DK2014/050094), but has not let to granting of a patent. Simon T Vistisen has ongoing research collaboration with Philips Healthcare including technical but not financial support from Philips Healthcare. Philips Healthcare has not had influence on the study design or the content of this paper.
Ethical standards
The study was approved by the relevant Danish authorities.
Additional information
Simon T Vistisen contributed entirely to the content of this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vistisen, S.T. Using extra systoles to predict fluid responsiveness in cardiothoracic critical care patients. J Clin Monit Comput 31, 693–699 (2017). https://doi.org/10.1007/s10877-016-9907-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9907-8