Abstract
β blockers reduce cerebral oxygenation after acute hemodilution and may contribute to the incidence of stroke when used perioperatively. The goal of the study was to investigate whether cerebral tissue oxygenation using near infrared spectroscopy can detect the β blocker-induced decrease in cerebral oxygenation depending on the severity of hemodilution and/or the dose of β blockers. Animals were anesthetized with 2 % isoflurane and randomly assigned to a landiolol or esmolol group. After baseline measurement, landiolol or esmolol was administered at 40 µg/kg/min for 20 min, increased to 200 µg/kg/min for 20 min, and then stopped. Hemodynamic and arterial variables and the tissue oxygenation index (TOI) were recorded at each β blocker dose. Two stages of hemodilution were sequentially induced by repeated hemorrhage of 600 ml (33 % of estimated blood volume) and infusion of the same volume of hydroxyethylstarch. During each stage, landiolol or esmolol was similarly administered and measurements were made. Landiolol and esmolol both dose-dependently decreased heart rate, mean arterial pressure and cardiac output, depending on the severity of hemodilution. Landiolol at 40 µg/kg/min was almost equivalent in potency to 200 µg/kg/min esmolol for decreasing HR before hemodilution. Based on the TOI, short-acting β blockers reduced cerebral oxygenation in a dose-dependent manner during hemodilution, and oxygenation returned to the baseline level after drug infusion was stopped. TOI may be useful for identification of a decrease in cerebral oxygenation for patients receiving β blockade during surgery associated with major bleeding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Perioperative β blockers prescribed for cardiac protection are associated with dose-dependent increases in adverse outcomes, including stroke and mortality [1–6]. Acute blood loss contributes to the incidence of these adverse events [5, 7]. Acute hemodilution causes a hemodynamic response in which adequate cerebral perfusion is maintained by an increase in cardiac output (CO) and preferential redistribution of blood flow to the brain [8–12]. β blockers reduce cerebral tissue oxygenation by restricting the cardiac response to acute hemodilution [13].
The volume of bleeding is a major factor in the increased mortality and incidence of multiple organ failure in patients treated with β blockers [7] and unexpected high blood loss associated with surgical bleeding may also occur during anesthesia. Hence, cerebral oxygenation monitoring using near infrared spectroscopy (NIRS), which permits non-invasive online monitoring of tissue oxygenation in a wide range of clinical scenarios [14], may be useful for patients receiving β blockade to prevent stroke during the perioperative period. Han et al. [15] used NIRS in major orthopedic surgery and found that esmolol-induced controlled hypotension caused a decrease in cerebral oxygen saturation during acute normovolemic hemodilution. However, it is unclear whether NIRS can detect the β blocker-induced decrease in cerebral oxygenation depending on the severity of hemodilution and/or the dose of β blocker.
The current animal study was conducted to determine whether the tissue oxygenation index (TOI) measured by NIRS could follow the effect of a β blocker on cerebral oxygenation under different hemodilution conditions and at different β blocker dosages. The short-acting β blockers, landiolol and esmolol, were used because these drugs allow individual titration of the drug effect due to their short half-lives of 4 and 9 min, respectively. Furthermore, comparison of the effects of these β blockers on TOI might allow examination of the influence of β1-selectivity on cerebral oxygenation. Landiolol is a highly β1-selective β blocker with a potency ratio (β1/β2) of 255, compared with 33 for esmolol [16], and several studies have shown that highly β1-selective agents are advantageous for preserving cerebral perfusion during hemodilution due to minimization of the effects of β2-mediated antagonism of cerebral vasodilation [17–19].
2 Materials and methods
2.1 Animal preparation
This study was approved by the Institutional Ethics Committee (Committee on Animal Research, Hamamatsu University School of Medicine, Hamamatsu, Japan). Twenty-four swine (body weight range: 24.5–26.9 kg, mean ± SD = 25.3 ± 0.6 kg) were used in the study. General anesthesia was achieved by isoflurane inhalation (5 %) in oxygen at 6 L/min, using a standard animal mask. After tracheostomy with regional anesthesia, anesthesia was maintained with a 2 % inhalational concentration of isoflurane and an oxygen-air mixture (oxygen : air = 1 : 1 L/min) via mechanical ventilation to keep a constant anesthetic depth throughout the study [20]. Exhalation gases were analyzed using a Capnomac Ultima (ULT-V-31-04, Datex-Ohmeda, Helsinki, Finland). A ventilator was set to keep end-tidal carbon dioxide between 35 and 45 mmHg during the animal preparation period and this setting was maintained throughout the study. Lead II of an electrocardiogram was monitored with three cutaneous electrodes. A pulmonary artery catheter (5 F, 4 lumen, Nihon Kohden, Tokyo, Japan) and a central venous catheter (16 gauge) were inserted via the right jugular vein and a catheter (16 gauge) was placed in the right femoral artery. All catheters were placed under local anesthetic. The blood temperature of the swine was maintained at 37.5–38.5 °C with heating lamps throughout the study. After these preparation steps, NIRS monitoring (NIRO-200, Hamamatsu Photonics, Hamamatsu, Japan) was started bilaterally by preparing the skin over the fronto-occipital regions and positioning electrodes. The TOI and normalized tissue hemoglobin index (nTHI) were collected electronically at intervals of 10 s using spatially resolved spectroscopy, which is not influenced by the scalp or surface area [21].
2.2 Experimental protocol
The experimental protocol is shown in
Fig. 1. After completion of animal preparation, baseline measurements were taken after a 20 min stabilization period. Animals were randomly assigned to the landiolol group (body weight range: 24.5–26.1 kg, mean ± SD = 25.2 ± 0.5 kg) and esmolol group (body weight range: 24.6–26.9 kg, mean ± SD = 25.4 ± 0.6 kg). Landiolol or esmolol was administered with an infusion pump via a central venous catheter at a rate of 40 µg/kg/min for 20 min, increased to a rate of 200 µg/kg/min for 20 min, and then stopped. The landiolol doses were determined based on our previous swine studies [22, 23] and the same doses were used for esmolol. Hemodynamic variables [heart rate (HR), mean arterial pressure (MAP), and CO], arterial blood analysis (pH, PCO2, PO2, hematocrit and O2 content), and NIRS values (TOI and nTHI) were recorded just before the start of β blocker infusion, after 20 min of 40 µg/kg/min infusion, after 20 min of 200 µg/kg/min infusion, and 20 min after stopping infusion. Hemodynamic variables except CO were also recorded at intervals of 1 min throughout the study. CO was determined with a thermodilution computer (Cardiac Output Computer, MTC6210, Nihon Kohden, Tokyo, Japan) using 5 ml of cold 5 % glucose injected into the right atrium. CO measurements were performed four times at each time point and the mean of the last three values was recorded. After these measurements, 600 ml of blood (approximately 33 % of estimated total blood volume; estimated total blood volume (ml) = 70 × 25 kg = 1,750 ml) was removed for 20 min via the arterial catheter and then the same volume of hydroxyethylstarch was infused for 20 min via the central venous catheter (33 % hemodilution). After a further 20 min stabilization period, each β blocker was administered and measurements were obtained as described above. Finally, a further 600 ml of blood was removed for 20 min via the arterial catheter and the same volume of hydroxyethylstarch was infused for 20 min via the central venous catheter (66 % hemodilution). After another 20 min stabilization period, each β blocker was administered and measurements were performed for a third time, again as described above.
2.3 Cerebral oxygenation measurements
TOI and nTHI were continuously measured by spatially resolved spectroscopy using a standard procedure with the NIRO-200 system (Hamamatsu Photonics). This form of spectroscopy uses continuous wave light emission coupled with light detectors at multiple distances. The NIRO-200 system transmits light at three wavelengths in the near infrared range (775, 810 and 850 nm), delivered via a fiber optic bundle terminating in an emission probe. A detection probe positioned 4 cm from the emission probe incorporates two aligned photographic detectors, which are separated by 4 mm. The emission and detection probes were fixed in a black rubber holder as a NIRO-200 probe and placed over the fronto-occipital regions bilaterally and covered with opaque dressing. Bilateral NIRO-200 probes were combined with measuring units connected to the NIRO-200 display unit. Spatially resolved spectroscopy measurements were made using slopes of the near infrared light attenuation versus the distances of the two detectors from the emission probe. By fitting these data to a modified diffusion equation describing light transport in tissue, the ratio of concentrations of oxyhemoglobin to total hemoglobin and the percentage change in the amount of initial hemoglobin (reflecting the change in regional blood volume), and hence the absolute average TOI and nTHI, were computed continuously [24, 25].
2.4 Statistical analysis
Data are expressed as mean values ± SD. Statistical analysis was performed using StatView 5.0 for Windows (Abacus Concepts, Berkeley, CA). Hemodynamic and arterial blood analysis variables and TOI and nTHI for each β blocker dose in all hemodilution stages and for each hemodilution stage at all β blocker doses were analyzed by repeated-measures one-way analysis of variance (ANOVA). If the ANOVA was significant, a Scheffe F-test for multiple comparisons was performed. Percentage changes in HR, MAP, CO and bilateral vertex TOI from the respective values before β blocker infusion were calculated. Values obtained with landiolol and esmolol at the same β blocker dose and same hemodilution state were compared by unpaired t test. P values <0.05 were considered to be significant.
3 Results
Averaged hemodynamic variables in the landiolol and esmolol groups are shown in Tables 1 and 2, respectively. Before hemodilution, esmolol decreased HR, MAP and CO, whereas landiolol did not decrease MAP. Stopping infusion for 20 min reversed these changes. At 33 and 66 % hemodilution, both drugs decreased HR, MAP and CO in a dose-dependent manner. These changes tended to recover after stopping infusion, but the values did not return to those before administration. Hemodilution produced compensatory increases in HR and CO, and both drugs attenuated these hemodynamic responses and decreased MAP in a dose-dependent manner.
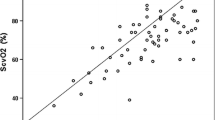
Averaged arterial blood analysis variables and TOI and nTHI values with landiolol and esmolol are shown in Tables 3 and 4, respectively, and individual changes in TOI are shown in Figs. 2 and 3, respectively. Hemodilution decreased hematocrit and O2 content by almost two-thirds at 33 % hemodilution and by another one-third at 66 % hemodilution. Bilateral TOI changed similarly in both groups, with TOI values in the left vertex tending to be smaller than those in the right vertex. Before hemodilution, β blockers did not change TOI, but TOI increased after infusion was stopped. After hemodilution, β blockers decreased TOI and dose dependency was observed at 66 % hemodilution in the landiolol group, and at 33 and 66 % hemodilution in the esmolol group. Stopping landiolol returned each TOI value to that before infusion. However, TOI did not return to the value before infusion after stopping esmolol at 66 % hemodilution. Hemodilution decreased nTHI and the extent of the change depended on the severity of hemodilution, but β blockers did not change nTHI.
Percentage changes in hemodynamic variables from each value before β blocker infusion are shown in Fig. 4. Hemodynamic changes induced by landiolol and esmolol after hemodilution were greater than those before hemodilution: 200 µg/kg/min landiolol decreased HR, MAP and CO by 18, −1 and 15 % compared to the respective pre-administration values before hemodilution; by 28, 23 and 34 % at 33 % hemodilution; and by 33, 33 and 35 % at 66 % hemodilution; and 200 µg/kg/min esmolol decreased these values by 14, 2 and 11 % before hemodilution; by 24, 16 and 32 % at 33 % hemodilution; and by 25, 25 and 31 % at 66 % hemodilution. Landiolol induced greater changes in HR than esmolol, with 40 µg/kg/min landiolol (13 ± 8 % decrease) having almost equivalent potency to 200 µg/kg/min esmolol (14 ± 8 % decrease) before hemodilution.
Percentage changes in HR, MAP, CO, and bilateral vertex tissue oxygenation index (TOI) from each value before infusion of landiolol or esmolol. HR heart rate, MAP mean arterial pressure, CO cardiac output, TOI Right or Left TOI of the right or left vertex. Asterisk Significant difference between % changes at same dose of β blockers before hemodilution. Dagger Significant difference between % changes at same dose of β blockers at 33 % hemodilution. Double dagger Significant difference between % changes at same dose of β blockers at 66 % hemodilution
Percentage changes in bilateral TOI from each value before β blocker infusion are also shown in Fig. 4. Decreases in TOI induced by landiolol and esmolol after hemodilution depended on the severity of hemodilution: 200 µg/kg/min landiolol decreased TOI in the right and left vertex by 7 and 5 % at 33 % hemodilution, and by 10 and 11 % at 66 % hemodilution; and 200 µg/kg/min esmolol decreased TOI in the right and left vertex by 6 and 5 % at 33 % hemodilution, and by 12 and 10 % at 66 % hemodilution. There were no significant differences in the % changes in bilateral TOI induced by the two drugs.
4 Discussion
This study shows that short-acting β blockers reduce cerebral oxygenation during hemodilution, as found previously for long-acting β blockers. This effect occurs because short-acting β blockers reduce compensatory increases of HR and CO in response to acute hemodilution and decrease MAP in a dose-dependent manner. Decreases in TOI induced by β blockers after hemodilution depended on the severity of hemodilution and the dose of β blockers, indicating that measurement of TOI using NIRS could be useful for monitoring of patients receiving β blockade to detect a decrease in cerebral oxygenation during surgery associated with major bleeding.
Han et al. [15] showed that controlled hypotension (target MAP: 55–65 mmHg) using esmolol decreased cerebral oxygen saturation at approximately 30 % acute normovolemic hemodilution in major orthopedic surgery, and that this decrease recovered after stopping controlled hypotension. These findings are consistent with our results and suggest that β blocker-induced hypotension during hemodilution is a potential neurological risk due to the decrease in cerebral oxygenation.
A NIRO monitor was used to measure nTHI and TOI using spatially resolved spectroscopy. Despite aggressive hemodilution, TOI did not decrease before β blocker infusion [26]. This finding suggests that oxygenation was maintained by fluid resuscitation using the same volume of hydroxyethylstarch, which effectively expanded the intravascular volume and induced an approximately 50 % increase in CO compared to CO before hemodilution. nTHI reflects the total hemoglobin concentration and is expressed relative to an initial value of 1. nTHI before landiolol administration had values of 1, 0.9 and 0.7 before hemodilution and at 33 and 66 % hemodilution, respectively (Tables 3, 4). Assuming no change in hemoglobin level with hemodilution, the regional blood volume decreased by 10 % from baseline at 33 % hemodilution and by 30 % at 66 % hemodilution. However, with landiolol, hemoglobin actually decreased from 9.8 g/dL before hemodilution to 5.7 g/dL at 33 % hemodilution and 3.6 g/dL at 66 % hemodilution, which indicates that the mean regional blood volume increased by 55 % at 33 % hemodilution and 91 % at 66 % hemodilution, compared to the volume before hemodilution. We speculate that the regional blood volume showed a compensatory increase in response to hemodilution to maintain oxygen delivery. Both doses of β blockers did not change nTHI, but decreased TOI. These findings indicate that landiolol and esmolol restrict blood inflow and outflow to the brain (assuming only inflow or outflow restriction, nTHI decreased or increased, indicating ischemia or congestion) and decrease the ratio of the concentration of oxyhemoglobin to that of total hemoglobin.
In this study, it was unclear if the decrease in TOI would reach a critical level for inducing cerebral injury. In a swine study of cardiopulmonary bypass (hematocrit 20 %), Hagino et al. [27] showed that animals with an average TOI < 55 % had cerebral injury, as evaluated using a neurologic deficit scale and histologic assessment, whereas animals with average TOI > 55 % showed minimal or no evidence of injury. Our results showed that this threshold was reached in one animal with landiolol and three with esmolol at 33 % hemodilution (hematocrit 21 %), and five animals with landiolol group and seven with esmolol group at 66 % hemodilution (hematocrit 12 %), all at doses of 200 µg/kg/min. We did not perform a histological examination after the experiments, but these animals might have been exposed to a critical state inducing cerebral injury.
Both drugs decreased TOI dose-dependently and to a similar extent during hemodilution, but careful interpretation of these results are required. The continuous infusion dose of landiolol is 10–40 µg/kg/min and that of esmolol is 150–300 µg/kg/min in humans, and the inhibitory potency of landiolol for reversal of an isoproterenol-induced increase in HR is six to eight times greater than that of esmolol in beagle dogs [28]. In the present study, 40 µg/kg/min landiolol had almost equivalent potency to 200 µg/kg/min esmolol for decreasing HR before hemodilution, whereas 200 µg/kg/min esmolol decreased TOI in the right vertex to a significantly greater extent than 40 µg/kg/min landiolol at 66 % hemodilution (p = 0.0083). Several studies of long-acting β blockers have shown that highly β1-selective agents are advantageous for preserving cerebral perfusion during hemodilution and reducing the risk of stroke due to minimization of the effects of β2-mediated antagonism of cerebral vasodilation [17–19]. Landiolol is a highly β1-selective β blocker with a potency ratio (β1/β2) of 255, compared with 33 for esmolol and 0.68 for propranolol [16]. Hence, landiolol might have less effect on cerebral oxygenation than esmolol and further studies are required to examine this issue.
Several limitations of the study should be addressed. There was no time-control group for measurements of TOI in the absence of β blocker infusion to determine the effect of hemodilution alone. In pilot studies, we found that TOI did not change for at least 60 min after completion of 33 and 66 % hemodilution alone, but it is possible that the effect of the β blocker on TOI might include the effect of hemodilution. In addition, because we did not measure the concentrations of β blockers, it was unclear whether the β blockers reached steady-state concentrations and/or underwent significant elimination after maintaining each dose for 20 min. Similarly, the half-lives of landiolol and esmolol are 4 and 9 min, respectively, in humans and the period without β blocker infusion was 80 min between each hemodilution stage; hence, the residual β blocker concentration before each stage was negligible. However, the impact of blocking the adrenergic input to the cardiovascular system might have sustained effects on intracellular signaling pathways. We also note that cerebral oxygenation was assessed in the bilateral vertex, but not in other brain regions, and thus the interpretation of the results may be limited because of the heterogeneity in metabolic demands in different brain regions [29].
In summary, NIRS could detect the β blocker-induced decrease in cerebral oxygenation depending on the severity of hemodilution and/or the dose of β blocker. The clinical implications are that β blocker-induced decreases in MAP and CO during hemodilution should be carefully monitored to prevent cerebral ischemia and that monitoring of cerebral tissue oxygenation is important for patients receiving β blockade in surgery in which major bleeding is anticipated.
References
Bangalore S, Gluud C, Wetterslev J, Messerli FH. Perioperative beta blockade. Lancet. 2008;372:1147–8.
Redelmeier D, Scales D, Kopp A. Beta blockers for elective surgery in elderly patients: population based, retrospective cohort study. BMJ. 2005;331:932.
Wallace AW, Au S, Cason BA. Perioperative β-blockade: atenolol is associated with reduced mortality when compared to metoprolol. Anesthesiology. 2011;114:824–36.
Yang H, Raymer K, Butler R, Parlow J, Roberts R. The effects of perioperative beta-blockade: results of the metoprolol after vascular surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006;152:983–90.
Beattie WS, Wijeysundera DN, Karkouti K, McCluskey S, Tait G, Mitsakakis N, Hare GM. Acute surgical anemia influences the cardioprotective effects of beta-blockade: a single center, propensity-matched cohort study. Anesthesiology. 2010;112:25–33.
Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, Xavier D, Chrolavicius S, Greenspan L, Pogue J, Pais P, Liu L, Xu S, Malaga G, Avezum A, Chan M, Montori VM, Jacka M, Choi P. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371:1839–47.
Le Manach Y, Collins GS, Ibanez C, Goarin JP, Coriat P, Gaudric J, Riou B, Landais P. Impact of perioperative bleeding on the protective effect of β-blockers during infrarenal aortic reconstruction. Anesthesiology. 2012;117:1203–11.
Ickx BE, Rigolet M, Van Der Linden PJ. Cardiovascular and metabolic response to acute normovolemic anemia. Eff Anesth Anesthesiol. 2000;93:1011–6.
van Bommel J, Trouwborst A, Schwarte L, Siegemund M, Ince C, Henny C. Intestinal and cerebral oxygenation during severe isovolemic hemodilution and subsequent hyperoxic ventilation in a pig model. Anesthesiology. 2002;97:660–70.
Weiskopf RB, Viele MK, Feiner J, Kelley S, Lieberman J, Noorani M, Leung JM, Fisher DM, Murray WR, Toy P, Moore MA. Human cardiovascular and metabolic response to acute, severe isovolemic anemia. JAMA. 1998;279:217–21.
Brown MM, Wade JP, Marshall J. Fundamental importance of arterial oxygen content in the regulation of cerebral blood flow in man. Brain. 1985;108:81–93.
Hare GM, Mazer CD, Mak W, Gorczynski RM, Hum KM, Kim SY, Wyard L, Barr A, Qu R, Baker AJ. Hemodilutional anemia is associated with increased cerebral neuronal nitric oxide synthase gene expression. J Appl Physiol. 2003;94:2058–67.
Ragoonanan TE, Beattie WS, Mazer CD, Tsui AK, Leong-Poi H, Wilson DF, Tait G, Yu J, Liu E, Noronha M, Dattani ND, Mitsakakis N, Hare GM. Metoprolol reduces cerebral tissue oxygen tension after acute hemodilution in rats. Anesthesiology. 2009;111:988–1000.
Scheeren TW, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26:279–87.
Han SH, Bahk JH, Kim JH, Lim YJ, Park CD, Do SH, Park YS. The effect of esmolol-induced controlled hypotension in combination with acute normovolemic hemodilution on cerebral oxygenation. Acta Anaesthesiol Scand. 2006;50:863–8.
Iguchi S, Iwamura H, Nishizaki M, Hayashi A, Senokuchi K, Kobayashi K, Sakaki K, Hachiya K, Ichioka Y, Kawamura M. Development of a highly cardioselective ultra short-acting β-blocker, ONO-1101. Chem Pharm Bull. 1992;40:1462–9.
Webb AJ, Fischer U, Rothwell PM. Effects of β-blocker selectivity on blood pressure variability and stroke. Neurology. 2011;77:731–7.
Hu T, Beattie WS, Mazer CD, Leong-Poi H, Fujii H, Wilson DF, Tsui AK, Liu E, Muhammad M, Baker AJ, Hare GM. Treatment with a highly selective β1 antagonist causes dose-dependent impairment of cerebral perfusion after hemodilution in rats. Anesth Analg. 2013;116:649–62.
Hare GM, Worrall JM, Baker AJ, Liu E, Sikich N, Mazer CD. Beta2 adrenergic antagonist inhibits cerebral cortical oxygen delivery after severe haemodilution in rats. Br J Anaesth. 2006;97:617–23.
Kurita T, Morita K, Fukuda K, Uraoka M, Takata K, Sanjo Y, Sato S. Influence of hemorrhagic shock and subsequent fluid resuscitation on the electroencephalographic effect of isoflurane in a swine model. Anesthesiology. 2005;103:1189–94.
Yoshitani K, Kawaguchi M, Miura N, Okuno T, Kanoda T, Ohnishi Y, Kuro M. Effects of hemoglobin concentration, skull thickness, and the area of the cerebrospinal fluid layer on near-infrared spectroscopy measurements. Anesthesiology. 2007;106:458–62.
Kurita T, Morita K, Fukuda K, Takata K, Uraoka M, Sanjo Y, Sato S. Landiolol, an ultra-short-acting beta 1-adrenoceptor antagonist, does not alter the electroencephalographic effect of isoflurane in swine model. Br J Anaesth. 2006;96:602–7.
Kurita T, Takata K, Uraoka M, Morita K, Sato S. Landiolol, an ultra-short-acting β1-adrenoceptor antagonist, does not alter the minimum alveolar anesthetic concentration of isoflurane in a swine model. Anesth Analg. 2007;105:656–60.
Matcher SJ, Kirkpatrick P, Nahid K, Cope M, Delpy D. Absolute quantification methods in tissue near infrared spectroscopy. Proc SPIE. 1995;2389:486–95.
Suzuki S, Takasaki S, Ozaki T, Kobayashi Y. Tissue oxygenation monitor using NIR spatially resolved spectroscopy. Proc SPIE. 1999;3597:582–92.
Tobias JD. Assessment of cerebral oxygenation using near infrared spectroscopy during isovolemic hemodilution in pediatric patients. J Clin Monit Comput. 2011;25:171–4.
Hagino I, Anttila V, Zurakowski D, Duebener LF, Lidov HG, Jonas RA. Tissue oxygenation index is a useful monitor of histologic and neurologic outcome after cardiopulmonary bypass in piglets. J Thorac Cardiovasc Surg. 2005;130:384–92.
Sugiyama A, Takahara A, Hashimoto K. Electrophysiologic, cardiohemodynamic and beta-blocking actions of a new ultra-short-acting beta-blocker, ONO-1101, assessed by the in vivo canine model in comparison with esmolol. J Cardiovasc Pharmacol. 1999;34:70–7.
Sakandzić S, Roussakis E, Yaseen MA, Mandeville ET, Srinivasan VJ, Arai K, Ruvinskaya S, Devor A, Lo EH, Vinogradov SA, Boas DA. Two-photon high-resolution measurement of partial pressure of oxygen in cerebral vasculature and tissue. Nat Methods. 2010;7:755–9.
Acknowledgments
Support was provided solely from institutional and/or departmental sources.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurita, T., Morita, K. & Sato, S. Evaluation of near infrared spectroscopy for detecting the β blocker-induced decrease in cerebral oxygenation during hemodilution in a swine model. J Clin Monit Comput 29, 779–788 (2015). https://doi.org/10.1007/s10877-015-9667-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9667-x