Abstract
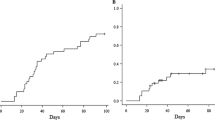
Allogeneic hematopoietic stem cell transplantation (HSCT) is curative for many patients with primary immune deficiency (PID). Haploidentical donors have historically been associated with higher rates of graft-versus-host disease (GvHD) and graft failure. Use of T cell receptor (TCR) α+β+/CD19+–depleted grafts has resulted in improved haploidentical HSCT outcomes. We sought to evaluate outcomes of TCR α+β+/CD19+–depleted haploidentical HSCT in pediatric patients with PID at a single center in Australia. Specifically, we evaluated immune reconstitution, looking at time to T cell and B cell reconstitution, and B cell function post-HSCT. Eleven patients with a mean age of 7.92 years (range 0.33–17.17 years) were included. The median time to B cell recovery was 93 days (range 41–205 days), and the median time to cessation of immunoglobulin replacement was 281.5 days (range 41–205 days). All patients who had ceased immunoglobulin replacement had an adequate response to pneumococcal conjugate (Prevenar 13) vaccine. The median time to CD4+ recovery was 132 days (range 30–296 days), and naive T cells were present in all surviving patients by 4 months post-HSCT. Eight of 11 patients are surviving, with six patients having whole blood chimerism greater than 95%, one patient with whole blood chimerism of 82.8%, and another with 76.0%. All of these patients clinically had no evidence of underlying immunodeficiency. Likelihood of overall survival at 2 years post-HSCT was 81.8%. Cumulative incidence of acute GvHD was 27.3%. Cumulative incidence of CMV viremia was 63.6%. All patients previously exposed to CMV had reactivation post-HSCT, but were controlled with pre-emptive CMV treatment. Assuming most children with PID have a haploidentical donor available, use of this technique is likely to result in good outcomes for patients who do not have a suitable matched sibling or matched unrelated donor.


Similar content being viewed by others
Abbreviations
- HSCT:
-
Hematopoietic stem cell transplant
- PID:
-
Primary immune deficiency
- GvHD:
-
Graft-versus-host disease
- TCR:
-
T cell receptor
- CMV:
-
Cytomegalovirus
- MUD:
-
Matched unrelated donor
- HLA:
-
Human leukocyte antigen
- SCID:
-
Severe combined immune deficiency
- MMF:
-
Mycophenolate mofetil
- CsA:
-
Cyclosporin A
- HHV-6:
-
Human herpes virus-6
- VODI:
-
Veno-occlusive disease with immunodeficiency
- ECP:
-
Extra-corporeal photopheresis
- MRI:
-
Magnetic resonance imaging
References
Smith AR, Gross TG, Baker KS. Transplant outcomes for primary immunodeficiency disease. Semin Hematol. 2010;47(1):79–85.
Szabolcs P, Cavazzana-Calvo M, Fischer A, Veys P. Bone marrow transplantation for primary immunodeficiency diseases. Pediatr Clin N Am. 2010;57:207–37.
Gennery AR, Slatter MA, Grandin L, Taupin P, Cant AJ, Veys P, et al. Transplantation of hematopoietic stem cells and long-term survival for primary immunodeficiencies in Europe: entering a new century, do we do better? J Allergy Clin Immunol. 2010;126(3):602–10.
Fernandes JF, Rocha V, Labopin M, Neven B, Moshous D, Gennery AR, et al. Transplantation in patients with SCID: mismatched related stem cells or unrelated cord blood? Blood. 2012;119:2949–55.
Rousso SZ, Shamriz O, Zilkha A, Braun J, Averbuch D, Or R, et al. Hematopoietic stem cell transplantations for primary immune deficiencies: 3 decades of experience from a tertiary medical center. J Pediatr Hematol Oncol. 2015;37:295–300.
Kongtim P, Cao K, Ciurea SO. Donor specific anti-HLA antibody and risk of graft failure in Haploidentical stem cell transplantation. Adv Hematol. 2016;2016:1–10.
Bertaina A, Merli P, Rutella S, Pagliara D, Bernardo ME, Masetti R, et al. HLA-haploidentical stem cell transplantation after removal of alpha beta+ T and B cells in children with nonmalignant disorders. Blood. 2014;124(5):822–6.
Balashov D, Shcherbina A, Maschan M, Trakhtman P, Skvortsova Y, Shelikhova L, et al. Single-center experience of unrelated and haploidentical stem cell transplantation with TCRab and CD19 depletion in children with primary immunodeficiency syndromes. Biol Blood Marrow Transplant. 2015;21:1955–62.
Laberko A, Bogoyavlenskaya A, Shelikhova L, Shekhovtsova Z, Balashov D, Voronin K, et al. Risk factors for and the clinical impact of cytomegalovirus and Epstein-Barr virus infections in pediatric recipients of TCR alpha/beta- and CD19-depleted grafts. Biol Blood Bone Marrow Transplant. 2017;23:483–90.
Shah RM, Elfeky R, Nademi Z, Qasim W, Amrolia P, Chiesa R. T-cell receptor alpha-beta+ and CD19+ cell-depleted haploidentical and mismatched hematopoietic stem cell transplantation in primary immune deficiency. J Allergy Clin Immunol. 2018;141(4):1417–26.
Przepiorka. Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Bryant KA, Block SL, Baker SA, Gruber WC, Scott DA, PCV13 Infant Study Group. Safety and immunogenicity of a 13-valent pneumococcal conjugate vaccine. Pediatrics. 2010;125(5):866–75.
Brodsky RA, Luznik L, Bolaños-Meade J, Leffell MS, Jones RJ, Fuchs EJ. Reduced intensity HLA-haploidentical BMT with post transplantation cyclophosphamide in nonmalignant hematologic diseases. Bone Marrow Transplant. 2008;42:523–7.
Abd Hamid IJ, Slatter MA, McKendrick F, Pearce MS, Gennery AR. Long-term health outcome and quality of life post-HSCT for IL7Ra-, Artemis-, RAG1- and RAG2-deficient severe combined immunodeficiency: a single center report. J Clin Immunol. 2018;38:727–32.
Hartz B, Marsh R, Rao K, Henter JI, Jordan M, Filipovich L. The minimum required level of donor chimerism in hereditary hemophagocytic lymphohistiocytosis. Blood. 2016;127(25):3281–90.
Author information
Authors and Affiliations
Contributions
Tim Brettig 50%, Theresa Cole 20%, Trisha Soosay Raj 15%, Richard Mitchell 10%, Joanne Smart, Sharon Choo, Francoise Mechinaud (5% combined).
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brettig, T., Smart, J., Choo, S. et al. Use of TCR α+β+/CD19+–Depleted Haploidentical Hematopoietic Stem Cell Transplant Is a Viable Option in Patients With Primary Immune Deficiency Without Matched Sibling Donor. J Clin Immunol 39, 505–511 (2019). https://doi.org/10.1007/s10875-019-00648-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-019-00648-x