Abstract
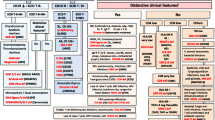
The number of genetically defined Primary Immunodeficiency Diseases (PID) has increased exponentially, especially in the past decade. The biennial classification published by the IUIS PID expert committee is therefore quickly expanding, providing valuable information regarding the disease-causing genotypes, the immunological anomalies, and the associated clinical features of PIDs. These are grouped in eight, somewhat overlapping, categories of immune dysfunction. However, based on this immunological classification, the diagnosis of a specific PID from the clinician’s observation of an individual clinical and/or immunological phenotype remains difficult, especially for non-PID specialists. The purpose of this work is to suggest a phenotypic classification that forms the basis for diagnostic trees, leading the physician to particular groups of PIDs, starting from clinical features and combining routine immunological investigations along the way. We present 8 colored diagnostic figures that correspond to the 8 PID groups in the IUIS Classification, including all the PIDs cited in the 2011 update of the IUIS classification and most of those reported since.








Similar content being viewed by others
Abbreviations
- αFP:
-
Alpha- fetoprotein
- Ab:
-
Antibody
- AD:
-
Autosomal dominant inheritance
- ADA:
-
Adenosine deaminase
- Adp:
-
Adenopathy
- AIHA:
-
Auto-immune hemolytic anemia
- AML:
-
Acute myeloid leukemia
- Anti PSS:
-
Anti- pneumococcus polysaccharide antibodies
- AR:
-
Autosomal recessive inheritance
- BL:
-
B lymphocyte
- CAPS:
-
Cryopyrin-associated periodic syndromes
- CBC:
-
Complete blood count
- CD:
-
Cluster of differentiation
- CGD:
-
Chronic granulomatous disease
- CID:
-
Combined immunodeficiency
- CINCA:
-
Chronic infantile neurologic cutaneous and articular syndrome
- FCM*:
-
Flow cytometry available
- CMML:
-
Chronic myelo-monocytic leukemia
- CNS:
-
Central nervous system
- CVID:
-
Common variable immunodeficiency disorders
- CT:
-
Computed tomography
- CTL:
-
Cytotoxic T-lymphocyte
- DA:
-
Duration of attacks
- Def:
-
Deficiency
- DHR:
-
DiHydroRhodamine
- Dip:
-
Diphtheria
- EBV:
-
Epstein-barr virus
- EDA:
-
Anhidrotic ectodermal dysplasia
- EDA-ID:
-
Anhidrotic ectodermal dysplasia with immunodeficiency
- EO:
-
Eosinophils
- FA:
-
Frequency of attacks
- FCAS:
-
Familial cold autoinflammatory syndrome
- FISH:
-
Fluorescence in situ hybridization
- GI:
-
Gastrointestinal
- Hib:
-
Haemophilus influenzae serotype b
- HIDS:
-
Hyper IgD syndrome
- HIES:
-
Hyper IgE syndrome
- HIGM:
-
Hyper Ig M syndrome
- HLA:
-
Human leukocyte antigen
- HSM:
-
Hepatosplenomegaly
- Hx:
-
Medical history
- Ig:
-
Immunoglobulin
- IL:
-
Interleukin
- LAD:
-
Leukocyte adhesion deficiency
- MKD:
-
Mevalonate kinase deficiency
- MSMD:
-
Mendelian susceptibility to mycobacteria disease
- MWS:
-
Muckle-Wells syndrome
- N:
-
Normal, not low
- NK:
-
Natural killer
- NKT:
-
Natural killer T cell
- NN:
-
Neonate
- NOMID:
-
Neonatal onset multisystem inflammatory disease
- NP:
-
Neutropenia
- PAPA:
-
Pyogenic sterile arthritis pyoderma gangrenosum, Acne syndrome
- PMN:
-
Neutrophils
- PT:
-
Platelet
- SCID:
-
Severe combined immune deficiencies
- Sd:
-
Syndrome
- SLE:
-
Systemic lupus erythematosus
- SPM:
-
Splenomegaly
- Subcl:
-
IgG subclass
- TCR:
-
T-cell receptor
- Tet:
-
Tetanus
- TL:
-
T lymphocyte
- TNF:
-
Tumor necrosis factor
- TRAPS:
-
TNF receptor-associated periodic syndrome
- WBC:
-
White blood cells
- XL:
-
X-linked
References
Al-Herz W, Bousfiha A, Casanova JL, Chapel H, Conley ME, Cunningham-Rundles C, et al. Primary immunodeficiency diseases: an update on the classification from the International Union of Immunological Societies Expert Committee for Primary Immunodeficiency. Front Immunol. 2011;2:54.
Parvaneh N, Casanova JL, Notarangelo LD, Conley ME. Primary immunodeficiencies: a rapidly evolving story. J Allergy Clin Immunol. 2013;131(2):314–23.
Ochs HD, Smith CIE, Puck JM. Primary immunodeficiency diseases: a molecular & cellular approach. 2nd ed. New York: Oxford University Press; 2007.
Casanova JL, Abel L. Primary immunodeficiencies: a field in its infancy. Science. 2007;317:617–9.
Notarangelo LD, Casanova JL. Primary immunodeficiencies: increasing market share. Curr Opin Immunol. 2009;21:461–5.
Conley ME, Notarangelo LD, Casanova JL. Definition of primary immunodeficiency in 2011: a “trialogue” among friends. N Y Acad Sci. 2011;1238:1–6.
Bousfiha AA, Jeddane L, Ailal F, Benhsaien I, Mahlaoui N, Casanova JL, et al. Primary immunodeficiency diseases worldwide: more common than generally thought. J Clin Immunol. 2012. doi:10.1007/s10875-012-9751-7.
de Vries E, European Society for Immunodeficiencies (ESID) members. Patient-centred screening for primary immunodeficiency, a multi-stage diagnostic protocol designed for non-immunologists: 2011 update. Clin Exp Immunol. 2012;167(1):108–19.
Oliveira JB, Fleisher TA. Laboratory evaluation of primary immunodeficiencies. J Allergy Clin Immunol. 2010;125:S297–305.
Admou B, Haouach K, Ailal F, Benhsaien I, Barbouch MR, Bejaoui M, et al. Primary immunodeficiencies: diagnosis approach in emergent countries (African Society for Primary Immunodeficiencies). Immunol Biol Spec. 2010;25(5–6):257–65.
Samarghitean C, Ortutay C, Vihinen M. Systematic classification of primary immunodeficiencies based on clinical, pathological, and laboratory parameters. J Immunol. 2009;183(11):7569–75.
Perreault S, Bernard G, Lortie A, Le Deist F, Decaluwe H. Ataxia-telangiectasia presenting with a novel immunodeficiency. Pediatr Neurol. 2012;46(5):322–4.
Rohr J, Beutel K, Maul-Pavicic A, Vraetz T, Thiel J, Warnatz K, et al. Atypical familial hemophagocytic lymphohistiocytosis due to mutations in UNC13D and STXBP2 overlaps with primary immunodeficiency diseases. Haematologica. 2010;95(12):2080–7.
Pessach I, Walter J, Notarangelo LD. Recent advances in primary immunodeficiencies: identification of novel genetic defects and unanticipated phenotypes. Pediatr Res. 2009;65(5 Pt 2):3R–12.
Villa A, Sobacchi C, Notarangelo LD, Bozzi F, Abinun M, Abrahamsen TG, et al. V(D)J recombination defects in lymphocytes due to RAG mutations: severe immunodeficiency with a spectrum of clinical presentations. Blood. 2001;97(1):81–8.
Acknowledgments
We thank Dr Capucine Picard and Dr Claire Fieschi for their contribution to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bousfiha, A.A., Jeddane, L., Ailal, F. et al. A Phenotypic Approach for IUIS PID Classification and Diagnosis: Guidelines for Clinicians at the Bedside. J Clin Immunol 33, 1078–1087 (2013). https://doi.org/10.1007/s10875-013-9901-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-013-9901-6