Abstract
Introduction
Influenza virus is a potential cause of severe disease in the immunocompromised. X-linked agammaglobulinemia (XLA) is a primary immunodeficiency characterized by the lack of immunoglobulin, B cells, and plasma cells, secondary to mutation in Bruton’s tyrosine kinase (Btk) gene. Btk is expressed in both B and dendritic cells (DC). However, little is known about the immune response of DC and T cells to influenza virus in XLA patients.
Methods
The in vitro maturation and antigen presenting function of monocyte-derived immature DC (imDC) from 12 XLA patients and 23 age-matched normal controls in response to influenza virus were examined. Influenza virus-specific CD4 and CD8 T cell responses in the patients and controls were further determined after administration of inactivated trivalent influenza vaccine.
Results
imDC from XLA patients had normal maturation based on major histocompatibility complex (MHC)-I, MHC-II, CD83 and CD86 expression, and interferon (IFN)-α and interleukin-12 production upon influenza virus stimulation. They also had a normal capacity to induce allogeneic T cell proliferation in response to influenza virus. TIV was well tolerated in XLA patients. Influenza virus-specific CD4+IFN-γ+ and CD8+ IFN-γ+ T cells and HLA-A2/M158–66-tetramer+ CTLs could be induced by TIV in XLA patients, and the levels and duration of maintaining these virus-specific cells in XLA patients are comparable to that in normal controls.
Conclusion
We demonstrated for the first time that XLA patients have fully competent DC and T cell immune responses to influenza virus. TIV is safe and could be an option for providing T cell-mediated protection against influenza virus infection in XLA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Influenza virus is a cause of substantial morbidity and mortality worldwide. Seasonal and pandemic influenza has posed many challenges for our community [1]. Children and the immunocompromised have high risks for influenza virus infection. X-linked agammaglobulinemia (XLA) is an X-chromosome linked recessive primary immunodeficiency characterized by the lack of immunoglobulin, B cells, and plasma cells, secondary to mutation in the Bruton’s tyrosine kinase (Btk) gene [2, 3]. Due to the deficiency of humoral immunity, cellular immune response becomes critical for these patients to control infections, including influenza.
T cell-mediated cellular immunity against virus depends on the activation of T cells by professional antigen presenting cells (APC), such as dendritic cells (DC). Btk is a member of the Tec family of protein tyrosine kinases, constitutively expressed in all hematopoietic cells including DC and monocytes, except T and natural killer cells [4, 5]. Multiple defects in the development and function of DC in XLA patients and Btk-deficient mice have been reported [6–11]. However, it is still not clear whether DC from XLA patients have defect in their maturation and cytokine production during influenza virus infection.
Very few but contradictory data on the T cell function in XLA patients and Btk-deficient mice were reported. One earlier study described an impaired delayed cutaneous hypersensitivity reaction in XLA patients [12]. However, another study of 5 XLA patients indicated that their T cell activity and cytokine production are normal in terms of T cell proliferation, interleukin (IL)-2, interferon (IFN)-γ, and IL-4 production in response to either various mitogens or tetanus toxoid [13]. In contrast, it has been demonstrated that there is predominant Th1 response in a cohort of 6 XLA patients [14]. Whether XLA patients have impaired T cell function, secondary to the deficiency of B cells or the defect of DC to influenza virus, remains unknown.
Recently, we summarized the clinical characteristics and genotype–phenotype correlation in 62 XLA patients diagnosed by our laboratory with confirmation of the mutations in Btk gene over the past 20 years [15, 16]. In the present study, using immature monocyte-derived DC (imDC) from XLA patients, we determined DC maturation and antigen presenting ability in response to influenza virus as defined by phenotype, cytokine production, and mixed lymphocyte reaction in vitro. The influenza virus-specific CD4+ and CD8+ T cell responses were further determined in XLA patients after administration of inactivated influenza vaccine.
Methods
Subjects
Twelve XLA patients aged 14–31 years old and 23 age-matched healthy volunteers were recruited before the 2008 influenza season and vaccinated with one dose of 2008–2009 seasonal trivalent influenza vaccine comprised of A/Brisbane/59/2007 (H1N1)-like, A/Brisbane/10/2007 (H3N2)-like, and B/Florida/4/2006-like strains manufactured by GlaxoSmithKline Biologicals. For patients, the exclusion criteria include known allergy to egg or component of the influenza vaccine, receipt of any other vaccine within 1 month. For healthy volunteers, the exclusion criteria include any serious infection at time of vaccination; known or suspected impairment of immunologic function including, but not limited to, clinically significant liver disease, diabetes mellitus, moderate to severe kidney impairment, and autoimmune disease; use of immunosuppressive medication; known allergy to egg or component of the influenza vaccine; and receipt of any other vaccine within 1 month. All patients were receiving regular intravenous immunoglobulin (IVIG) replacement therapy at 4-week intervals. The first blood draw was taken prior to the infusion of IVIG, and the subsequent blood draw was taken at indicated time after vaccination. The research protocol was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
Generation of imDC In Vitro
Monocytes and CD3+ T cells were isolated from PBMCs by using anti-CD14 and anti-CD3 microbeads respectively (Miltenyi Biotec, Germany) [17, 18]. The purity of isolated CD14+ cells and CD3+ T cells was consistently ranging from 93% to 97%, as determined by flow cytometry. Monocytes were cultured in RPMI supplemented with 10% human AB serum, 10 ng/ml IL-4, and 50 ng/ml GM-CSF (Peprotech, Rocky Hill, NJ, USA) for 7 days to generate imDC as we described before [19, 20].
Phenotypic Analysis and Cytokine Measurement
Influenza A virus H1N1 (A/HK/54/98) was heat-inactivated at 56°C for 30 min. imDC were incubated with H1N1 at multiplicity of infection (MOI) of 1 in the absence of human AB serum. After 1 h of viral adsorption, the culture was supplemented with 10% human AB serum. After 24 h of culture with virus, imDC were collected and analyzed by immunofluorescent staining using mAbs PE/Cy5 anti-major histocompatibility complex (MHC)-I, APC anti-CD83, and PE anti-CD86 (Biolegend, San Diego, CA, USA), fluorescein isothiocyanate (FITC) anti-MHC-II (BD Pharmingen, San Jose, CA, USA) to determine phenotypic maturation with flow cytometer. Supernatants were collected and the concentrations of IL-12 and IFN-α were determined by Human IL-12 DuoSet (R&D system, Minneapolis, MN, USA) and Verikine™ Human IFN-α ELISA Kit (PBL InterferonSource, Piscataway, NJ, USA), respectively.
Mixed Lymphocyte Reaction
Allogeneic peripheral CD3+ T cells were cultured in triplicate in a 96-well, flat-bottomed microplate with different numbers of irradiated (30 Gy) virus-treated imDC (DC/T cells ratio of 1:1,000, 1:100, or 1:10). [3H]-Thymidine was added to the wells 18 h before the end of 6 days culture, and its incorporation was measured to determine cell proliferation as described previously [21] with incorporation expressed as the mean ± SEM counts per minute of three wells.
Influenza Virus-Specific T Cell Immunity
The memory/effector influenza virus-specific CD4 and CD8 T cells were measured by whole blood intracellular cytokine staining assay as we established before [22–24]. Fresh, heparinized whole blood was incubated with 2008–2009 trivalent seasonal influenza vaccine at a final concentration of 4.0 μg/ml. The negative control was phosphate-buffered saline (PBS). Co-stimulation was done with anti-CD28 and anti-CD49d mAbs (3 μg/ml; BD Biosciences, San Jose, CA, USA). After 2 h of incubation, brefeldin A was added at a final concentration of 10 μg/ml, and the blood samples were incubated for an additional 4 h. Following 6 h of incubation, red blood cells were lysed and fixed by FACS lysing solution (BD Biosciences). The fixed cells were washed; stained with mAb mixture consisting of anti-CD3-PE, anti-CD4-PE-Cy5, and anti-CD8-APC (BD Biosciences, San Jose, CA, USA) for surface markers; and then cells were permeabilized and stained with IFN-γ-FITC intracellularly. Isotype-matched control mAbs of irrelevant specificity were included in all experiments [25, 26]. For tetramer analysis, PBMCs were incubated with anti-CD3, anti-CD8, and HLA-A2/M158–66 tetramer (Beckman Coulter) for 30 min [23]. HLA-A*0201 phenotype screening was done with primary MAbs MA2.1 (HLA-A2 and B17) or BB7.2 (HLA-A2 and Aw69) (ATCC) and secondary FITC goat-anti-mouse IgG. Samples were collected 2–5 × 105 events for each sample with FACSAria flow cytometer (BD Biosciences). Data were prepared for statistical analysis using FLOW JO software (Tree Star, San Carlos, CA, USA).
Statistical Analysis
Data were expressed as mean ± SEM. Statistical analysis was performed by Student’s paired t test or one-way ANOVA with a multiple comparison test using Prism 5 (GraphPad Software). P < 0.05 was considered significant.
Results
The Differentiation and Maturation of imDC in XLA Patients Upon Influenza Virus Stimulation
imDC were generated in vitro from purified blood monocytes from 12 XLA patients and 23 age-matched healthy donors in the presence of IL-4 and GM-CSF. As shown in Fig. 1, the monocytes from XLA patients and normal controls differentiated into imDC after 7 days of culture. The imDC derived from monocytes of patients expressed similar level of MHC-I, MHC-II, and CD83 but lower CD86 level compared to that of normal controls (Fig. 1a, b). After 24 h stimulation with influenza virus, significant upregulation of CD83 and CD86 expressions was observed in imDC from patients (Fig. 1b). In contrast, MHC-I, MHC-II, CD83, and CD86 molecules in imDC from normal controls were all upregulated by stimulation with influenza virus (Fig. 1b). Importantly, the expression level of these four molecules in imDCs from patients after stimulation with influenza virus was comparable to that from normal controls (Fig. 1b). These data indicated that imDC from XLA patients have normal differentiation and maturation upon influenza virus stimulation in terms of the phenotype.
The differentiation and maturation of imDC in XLA patients upon influenza virus stimulation. Monocyte-derived imDC from XLA patients (n = 12) and normal controls (n = 23) were treated with heat killed H1N1 (MOI = 1) for 24 h. Surface expressions of MHC-I, MHC-II, CD83, and CD86 were examined by flow cytometry. a Histogram showed the representative data of the increase in phenotype expressions after virus stimulation; b bar chart showed the mean fluorescent intensity of the phenotype expression. Data represented as mean ± SEM. *p < 0.05; **p < 0.01
Cytokine Production of DC in XLA Patients Upon Influenza Virus Stimulation
To further confirm whether the mature phenotype of imDC from XLA patients was associated with normal function of DC in terms of cytokine production, the production of IFN-α and IL-12 in imDC upon influenza virus stimulation was examined. As shown in Fig. 2, influenza virus significantly enhanced the production of IFN-α in imDC from either patients or normal controls as compared to mock-treated imDC. However, influenza virus did not induce IL-12 production in imDC from patients or normal controls. The levels of IFN-α and IL-12 produced by imDC from patients were similar to that from normal controls before or after influenza virus stimulation. These data indicated that imDC from XLA patients has normal function in response to influenza virus.
Cytokine production in DC in XLA patients upon influenza virus stimulation. Monocyte-derived imDC from XLA patients (n = 12) and normal controls (n = 23) were treated with heat killed H1N1 (MOI = 1) for 24 h. The concentrations of IFN-α and IL-12 in culture supernatant was determined by ELISA. Data represented as mean ± SEM. NS no significant difference; *p < 0.05; **p < 0.01; ***p < 0.001
T Cell Stimulatory Ability of Influenza Virus-Treated DC in XLA Patients
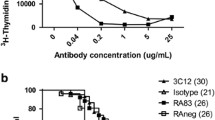
To determine the T cell stimulatory capacity of influenza virus-treated imDC from XLA patients, allogeneic naïve CD3+ T cells were stimulated with influenza virus- or mock-treated imDC from XLA patients and normal controls. As shown in Fig. 3, influenza virus-treated imDC from patients or normal controls induced allogeneic naïve CD3+ T cell proliferation in a dose-dependent manner. There was no significant difference between imDC from patients and normal controls in their capacities to induce allogeneic T cell proliferation. These data suggest that imDC from XLA patients have a normal capacity to induce T cell responses to influenza viruses.
T cell stimulatory ability of influenza virus-treated DC in XLA patients. Monocyte-derived imDC from XLA patients (n = 12) and normal controls (n = 23) were treated with heat killed H1N1 (MOI = 1) or mock for 24 h. Cells were then irradiated and co-cultured with allogeneic purified CD3+ T at different DC/T ratio for 6 days. The proliferative responses of CD3+ T cells were measured by [3H]-thymidine incorporation assay. Data represented as mean ± SEM. ***p < 0.001
Safety of TIV in XLA Patients
Twelve XLA patients and 23 age-matched normal controls were administrated with one dose of TIV intramuscularly. TIV was well tolerated in both groups. No obvious adverse events, including induration, redness, ecchymosis, and shivering, were reported during the first month after vaccination in both patients and normal controls.
Induction of Influenza Virus-Specific T Cells by TIV in XLA Patients
To determine influenza virus-specific T cell immunity in XLA patients in vivo, the frequencies of peripheral blood influenza-specific CD4+ and CD8+ T cells were assessed in these XLA patients and normal controls before and after 1 week, 1 month, 3 months, and 6 months of TIV vaccination using vaccine as an antigenic stimulus in vitro. As shown in representative studies from a single normal adult donor (Fig. 4a), a discrete subset of CD4+ or CD8+ T cells expressing IFN-γ were generated after incubation with influenza vaccine antigen. Only cells with IFN-γ expression were considered as true positive influenza-specific CD4+ or CD8+ T cells, as previously described [23, 24]. Frequencies of IFN-γ+CD4+ or IFN-γ+CD8+ T cells detected after addition of PBS buffer were very low indicating the antigen-specificity of this response.
Induction of influenza virus-specific T cells by TIV in XLA patients. a Representative results of influenza-specific expression in CD4+IFN-γ+ and CD8+ IFN-γ+ T cells from a normal individual after 3 month of TIV vaccination were shown. b The frequency of CD4+IFN-γ+ and CD8+ IFN-γ+ T cells in the peripheral blood from XLA patients (n = 12) and normal controls (n = 23) before and after TIV vaccination. c The fold increase of influenza-specific CD4+IFN-γ+ and CD8+ IFN-γ+ T cells from the basal level in XLA patients (n = 12) and normal controls (n = 23). NS no significant difference
In both XLA patients and normal controls, the frequency of influenza-specific CD4+ T cells gradually increased from 1 week to 6 months post-vaccination and reached peak levels at months 3 and 6 post-vaccination (Fig. 4b). To compare the induction of influenza-specific CD4+ T cells between patients and normal controls after immunization, we evaluated the fold increase of influenza-specific CD4+ T cells from the basal level at the time of pre-vaccination. As shown in Fig. 4c, the fold increase of influenza-specific CD4+ T cells in both patients and normal controls is comparable at each time point post-vaccination, indicating XLA patients had normal CD4+ T cell responses to influenza vaccine.
Similarly, influenza-specific CD8+ T cells were also induced by vaccine in XLA patients. The frequency of influenza-specific CD8+ T cells gradually increased from 1 week to 6 months post-vaccination and reached a peak level at month 6 post-vaccination in both patients and normal controls (Fig. 4b). For the fold increase of influenza-specific CD8+ T cells from the basal level, there was no significant difference between patients and normal controls at each time point post-vaccination (Fig. 4c). This result suggests that XLA patients had normal CD8+ T cell responses to TIV.
Induction of Influenza Virus M158–66 Epitope-Specific Memory CTLs by TIV in XLA Patients
To further evaluate influenza virus-specific CD8+ cell immunity in XLA patients in vivo, the frequencies of peripheral blood influenza virus M158–66 epitope-specific memory CTLs were assessed in HLA-A2-positive XLA patients and normal controls. HLA-A2/M158–66-tetramer+ CD8+ T cells from PBMCs isolated from seven HLA-A2-positive XLA patients and 14 HLA-A2-positive normal controls before and after TIV vaccination were analyzed. Among them, one out of seven patients and two out of 14 normal individuals had detectable HLA-A2/M158–66-tetramer+ CTLs before immunization (Fig. 5). After influenza vaccination, the frequency of HLA-A2/M158–66-tetramer+ CTLs was increased from week 1 to month 3 post vaccination and dropped to the basal level after 6 months of vaccination in patient and one normal control, whereas the frequency of HLA-A2/M158–66-tetramer+ CTLs maintained up to 6 months post-vaccination in another normal control. These results indicated that TIV can induce CTL response in both XLA patient and normal control although the duration for maintain CLTs may varied among different cases (Fig. 5).
Induction of influenza virus M158–66 epitope-specific memory CTLs by TIV in XLA patient. PBMCs from HLA-A2-seropositive XLA patients and normal controls were isolated before and after influenza vaccination at indicated time. HLA-A2/M158–66 tetramer staining was performed and analyzed by flow cytometry. The numbers showed here indicated the frequency of HLA-A2/M158–66 tetramer+ cells within the population of CD3+CD8+ T cells. The data from one XLA patient and two normal controls with detectable HLA-A2/M158–66 tetramer+ cells were shown
Discussion
In this study, using imDC from XLA patients, we first showed that these imDC had normal maturation and antigen presenting function in response to influenza virus in vitro. By administration of TIV, we further demonstrated that XLA patient had normal influenza virus-specific CD4+ and CD8+ T cell responses in vivo. This, to the best of our knowledge, is the first time to report that XLA patient had a fully competent DC and T cell immune response to influenza virus.
As Btk gene is constitutively expressed in DC and monocytes, it is believed that the deficiency of Btk may affect the maturation and function of DC. Indeed, Btk has been demonstrated to be involved in toll-like receptor (TLR) signaling [7, 9, 10]. However, the data from different cohorts of XLA patients were not consistent. One study in a cohort of eight XLA patients indicated that imDC from XLA patients had less phenotypic maturation based on CD83 expression and TNF-a production than controls, whereas the productions of IL-6 and IL-12 in patients were comparable to that in controls [27]. Other two studies, one in a cohort of five XLA patients and another one in a cohort of six XLA patients, showed that DC from XLA patients had normal phenotypic maturation and antigen presenting function and no defect in the production of IL-10 and IL-12 in response to stimulation of TLR1/2, 2/6, 3, 4, and 5 but display impaired TLR8-mediated IL-6 and TNF-α production and TLR2- and TLR4-mediated TNF-α and IL-1β production [6, 10]. Here, we demonstrated that, although the CD86 expression in imDC of XLA patients was also lower than that in normal controls, imDC from XLA patients have normal maturation based on phenotype (MHC-I, MHC-II, CD83, and CD86) expressions. In addition, imDC in XLA patients have normal ability to produce the major anti-viral cytokine IFN-α upon influenza virus stimulation. Importantly, influenza virus-treated DC have also showed a normal capacity to induce allogeneic T cell proliferation.
The reason for the difference of DC maturation remains unknown. Bayry et al. reported that the maturation of DC from XLA patients in the presence of their autologous plasma was severely impaired [28]. When reconstitution of patients’ plasma with IVIG corresponding to the concentration reached in patients’ plasma immediately following infusion or with natural anti-CD40 IgG from IVIG, it could restore some of the defects of DC maturation [28]. This suggests that the impaired maturation of DC in XLA patients may be related with the deficiency of circulating natural antibodies, especially natural IgG to CD40. Since the blood samples from XLA patients were taken prior to the infusion of IVIG, their autologous plasma may only have very low levels of the natural antibodies. Therefore, Batry’s study found a severe impairment of DC maturation. In contrast, our current study and others used normal human AB serum or fetal bovine sera for the culture of DC, thus found a normal maturation of DC in XLA patients.
Whether B cells can regulate T cell-mediated immune responses is still controversial. Some studies showed that B cells were dispensable for the generation and maintenance of antigen-specific T cell responses [29, 30], whereas other studies have demonstrated that B cells can actively participate in T-cell mediated immune responses by directing the magnitude and quality of the T cell response to foreign and self-antigens [31, 32]. Here, using XLA patients as a unique human model in absence of B cells, we, for the first time, administrated TIV to XLA patients and evaluated the induction of virus-specific CD4 and CD8 T cells by vaccine. We found that both influenza virus-specific CD4+ and CD8+ T cells can be induced by TIV in XLA patients, and the levels and the duration of maintaining these virus-specific cells in XLA patients are comparable to that in normal controls. Our data indicated that the absence of B cells does not affect the generation and maintenance of influenza virus-specific memory T cells. Indeed, a previous study also showed a normal hepatitis B envelope Ag-specific CD4+ T cell memory response in a cohort of nine XLA patients after HBV vaccination [33]. Of note, as all these XLA patients received regular IVIG replacement therapy, we cannot exclude the possibility that natural antibodies are involved in the generation and maintenance of virus-specific memory T cells.
Here, we further showed that TIV induced HLA-A2/M158–66-tetramer+ CTLs in 14% of HLA-A2-positive XLA patients and normal individuals respectively, and these induced epitope-specific memory CTLs can maintain up to 3 or 6 months after vaccination in XLA patients or normal controls. Consistent with our data, previous studies also showed that TIV could induce HLA-A2/M158–66-tetramer+ CTLs in 12% to 25% of HLA-A2-positive normal individuals [34, 35]. Importantly, no obvious side effect of TIV in XLA patients was observed. Our data suggest that influenza vaccine is able to induce some protection against influenza virus infection for XLA patients even though no protective antibodies can be generated. Live attenuated influenza vaccine (LAIV) is expected to induce T cell responses more efficiently than inactivated influenza vaccine, as it contains all the viral internal proteins. In fact, the frequency of influenza A virus-specific CD4 and CD8 T cells significantly increased after LAIV but not TIV immunization in children aged 5 to 9 years [36]. This suggests that LAIV might have more benefits than TIV in providing T cell-mediated protection against influenza virus in XLA patients, and this needs to be further confirmed by a well-designed case–control study in the future.
In conclusion, we have demonstrated that XLA patients have a normal DC and T cell response to influenza virus and B cells are dispensable for the generation and maintenance of influenza virus-specific memory T cells. Our data suggest that TIV is safe and could be an option for providing T cell-mediated protection against influenza virus infection in XLA patients. These data may also provide some valuable insights to the management and general vaccine strategy to alleviate illness severity for this particular group of immunodeficient patients.
References
Peiris JS, Tu WW, Yen HL. A novel H1N1 virus causes the first pandemic of the 21(st) century. Eur J Immunol. 2009;39(11):2946–54.
Conley ME. B cells in patients with X-linked agammaglobulinemia. J Immunol. 1985;134(5):3070–4.
Kinnon C, Hinshelwood S, Levinsky RJ, Lovering RC. X-linked agammaglobulinemia—gene cloning and future prospects. Immunol Today. 1993;14(11):554–8.
Rawlings DJ, Witte ON. The Btk subfamily of cytoplasmic tyrosine kinases: structure, regulation and function. Semin Immunol. 1995;7(4):237–46. doi:10.1006/smim.1995.0028.
Vetrie D, Vorechovsky I, Sideras P, Holland J, Davies A, Flinter F, et al. The gene involved in X-linked agammaglobulinaemia is a member of the Src family of protein-tyrosine kinases. Nature. 1993;361(6409):226–33. doi:10.1038/361226a0.
Gagliardi MC, Finocchi A, Orlandi P, Cursi L, Cancrini C, Moschese V, et al. Bruton's tyrosine kinase defect in dendritic cells from X-linked agammaglobulinaemia patients does not influence their differentiation, maturation and antigen-presenting cell function. Clin Exp Immunol. 2003;133(1):115–22.
Gray P, Dunne A, Brikos C, Jefferies CA, Doyle SL, O'Neill LA. MyD88 adapter-like (Mal) is phosphorylated by Bruton's tyrosine kinase during TLR2 and TLR4 signal transduction. J Biol Chem. 2006;281(15):10489–95. doi:10.1074/jbc.M508892200.
Kawakami Y, Inagaki N, Salek-Ardakani S, Kitaura J, Tanaka H, Nagao K, et al. Regulation of dendritic cell maturation and function by Bruton's tyrosine kinase via IL-10 and Stat3. Proc Natl Acad Sci U S A. 2006;103(1):153–8. doi:10.1073/pnas.0509784103.
Schmidt NW, Thieu VT, Mann BA, Ahyi AN, Kaplan MH. Bruton's tyrosine kinase is required for TLR-induced IL-10 production. J Immunol. 2006;177(10):7203–10.
Sochorova K, Horvath R, Rozkova D, Litzman J, Bartunkova J, Sediva A, et al. Impaired Toll-like receptor 8-mediated IL-6 and TNF-alpha production in antigen-presenting cells from patients with X-linked agammaglobulinemia. Blood. 2007;109(6):2553–6. doi:10.1182/blood-2006-07-037960.
Horwood NJ, Page TH, McDaid JP, Palmer CD, Campbell J, Mahon T, et al. Bruton's tyrosine kinase is required for TLR2 and TLR4-induced TNF, but not IL-6, production. J Immunol. 2006;176(6):3635–41.
Crockard AD, Boyd NA, McNeill TA, McCluskey DR. CD4 lymphocyte subset abnormalities associated with impaired delayed cutaneous hypersensitivity reactions in patients with X-linked agammaglobulinaemia. Clin Exp Immunol. 1992;88(1):29–34.
Plebani A, Fischer MB, Meini A, Duse M, Thon V, Eibl MM. T cell activity and cytokine production in X-linked agammaglobulinemia: implications for vaccination strategies. Int Arch Allergy Immunol. 1997;114(1):90–3.
Amedei A, Romagnani C, Benagiano M, Azzurri A, Fomia F, Torrente F, et al. Preferential Th1 profile of T helper cell responses in X-linked (Bruton's) agammaglobulinemia. Eur J Immunol. 2001;31(6):1927–34. doi:10.1002/1521-4141(200106)31:6<1927::AID-IMMU1927>3.0.CO;2-D.
Lee PP, Chen TX, Jiang LP, Chan KW, Yang W, Lee BW, et al. Clinical characteristics and genotype–phenotype correlation in 62 patients with X-linked agammaglobulinemia. J Clin Immunol. 2010;30(1):121–31. doi:10.1007/s10875-009-9341-5.
Lau YL, Levinsky RJ, Malcolm S, Goodship J, Winter R, Pembrey M. Genetic prediction in X-linked agammaglobulinaemia. Am J Med Genet. 1988;31(2):437–48. doi:10.1002/ajmg.1320310224.
Zheng J, Liu Y, Qin G, Lam KT, Guan J, Xiang Z, et al. Generation of human Th1-like regulatory CD4+ T cells by an intrinsic IFN-gamma- and T-bet-dependent pathway. Eur J Immunol. 2011;41(1):128–39. doi:10.1002/eji.201040724.
Mao H, Tu W, Qin G, Law HK, Sia SF, Chan PL, et al. Influenza virus directly infects human natural killer cells and induces cell apoptosis. J Virol. 2009;83(18):9215–22. doi:10.1128/JVI.00805-09.
Liu E, Tu W, Law HK, Lau YL. Decreased yield, phenotypic expression and function of immature monocyte-derived dendritic cells in cord blood. Br J Haematol. 2001;113(1):240–6.
Zheng J, Liu Y, Lau YL, Tu W. CD40-activated B cells are more potent than immature dendritic cells to induce and expand CD4(+) regulatory T cells. Cell Mol Immunol. 2010;7(1):44–50. doi:10.1038/cmi.2009.103.
Zheng J, Liu Y, Qin G, Chan PL, Mao H, Lam KT, et al. Efficient induction and expansion of human alloantigen-specific CD8 regulatory T cells from naive precursors by CD40-activated B cells. J Immunol. 2009;183(6):3742–50. doi:10.4049/jimmunol.0901329.
Tu W, Chen S, Sharp M, Dekker C, Manganello AM, Tongson EC, et al. Persistent and selective deficiency of CD4+ T cell immunity to cytomegalovirus in immunocompetent young children. J Immunol. 2004;172(5):3260–7.
Tu W, Mao H, Zheng J, Liu Y, Chiu SS, Qin G, et al. Cytotoxic T lymphocytes established by seasonal human influenza cross-react against 2009 pandemic H1N1 influenza virus. J Virol. 2010;84(13):6527–35. doi:10.1128/JVI.00519-10.
Zeman AM, Holmes TH, Stamatis S, Tu W, He XS, Bouvier N, et al. Humoral and cellular immune responses in children given annual immunization with trivalent inactivated influenza vaccine. Pediatr Infect Dis J. 2007;26(2):107–15. doi:10.1097/01.inf.0000253251.03785.9b00006454-200702000-00003.
Qin G, Liu Y, Zheng J, Ng IH, Xiang Z, Lam KT, et al. Type 1 responses of human V{gamma}9V{delta}2 T cells to influenza A viruses. J Virol. 2011;85(19):10109–16. doi:10.1128/JVI.05341-11.
Tu W, Zheng J, Liu Y, Sia SF, Liu M, Qin G, et al. The aminobisphosphonate pamidronate controls influenza pathogenesis by expanding a gammadelta T cell population in humanized mice. J Exp Med. 2011;208(7):1511–22. doi:10.1084/jem.20110226.
Taneichi H, Kanegane H, Sira MM, Futatani T, Agematsu K, Sako M, et al. Toll-like receptor signaling is impaired in dendritic cells from patients with X-linked agammaglobulinemia. Clin Immunol. 2008;126(2):148–54.
Bayry J, Lacroix-Desmazes S, Donkova-Petrini V, Carbonneil C, Misra N, Lepelletier Y, et al. Natural antibodies sustain differentiation and maturation of human dendritic cells. Proc Natl Acad Sci U S A. 2004;101(39):14210–5. doi:10.1073/pnas.04021831010402183101.
Di Rosa F, Matzinger P. Long-lasting CD8 T cell memory in the absence of CD4 T cells or B cells. J Exp Med. 1996;183(5):2153–63.
Epstein MM, Di Rosa F, Jankovic D, Sher A, Matzinger P. Successful T cell priming in B cell-deficient mice. J Exp Med. 1995;182(4):915–22.
Linton PJ, Harbertson J, Bradley LM. A critical role for B cells in the development of memory CD4 cells. J Immunol. 2000;165(10):5558–65.
Lund FE, Randall TD. Effector and regulatory B cells: modulators of CD4(+) T cell immunity. Nat Rev Immunol. 2010;10(4):236–47. doi:10.1038/nri2729.
Paroli M, Accapezzato D, Francavilla V, Insalaco A, Plebani A, Balsano F, et al. Long-lasting memory-resting and memory-effector CD4+ T cells in human X-linked agammaglobulinemia. Blood. 2002;99(6):2131–7.
Rastogi D, Wang C, Mao X, Lendor C, Rothman PB, Miller RL. Antigen-specific immune responses to influenza vaccine in utero. J Clin Invest. 2007;117(6):1637–46. doi:10.1172/JCI29466.
Terajima M, Cruz J, Leporati AM, Orphin L, Babon JA, Co MD, et al. Influenza A virus matrix protein 1-specific human CD8+ T-cell response induced in trivalent inactivated vaccine recipients. J Virol. 2008;82(18):9283–7. doi:10.1128/JVI.01047-08.
He XS, Holmes TH, Zhang C, Mahmood K, Kemble GW, Lewis DB, et al. Cellular immune responses in children and adults receiving inactivated or live attenuated influenza vaccines. J Virol. 2006;80(23):11756–66. doi:10.1128/JVI.01460-06.
Acknowledgments
We thank the help from Ms. Winnie Wai Sim Lau to recruit the patients. This work was supported in part by the General Research Fund, Research Grants Council of Hong Kong (HKU768108, HKU 777108M, W.T. and Y.L.L), the Area of Excellence program on Influenza supported by the University Grants Committee of the Hong Kong SAR, China (project no. AoE/M-12/06, Y.L.L. and W.T.), and Research Fund for the Control of Infectious Diseases, Diseases of the Food and Health Bureau of the Hong Kong SAR (HK-09-03-05).
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Yinping Liu and Yuet Wu contributed equally to this work.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Liu, Y., Wu, Y., Lam, KT. et al. Dendritic and T Cell Response to Influenza is Normal in the Patients with X-Linked Agammaglobulinemia. J Clin Immunol 32, 421–429 (2012). https://doi.org/10.1007/s10875-011-9639-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-011-9639-y