Abstract
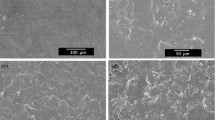
The release behavior of vancomycin (VAN) from beta-tricalciumphosphate (βTCP), hydroxyapatite (HA), glass ceramic (GC) and sponge-like collagen βTCP granule composite (sponge) was studied. Vacuum and drip loading methods were compared. The influence of VAN concentration and pH on release behavior was analyzed with respect to a stable release level of VAN above the minimum inhibitory concentration over 14 days. Initially the morphology of the granule carrier systems was examined with ESEM, stereomicroscopy, µCT-imaging and Camsizer® regarding porosity, interconnecting pores and granule size. Drug release patterns following a vacuum and a drip loading method with VAN at concentrations of 5 and 50 mg/ml were compared. The influence of pH 7.4 compared to pH 5.0 on release behavior was studied. The drug was released in bidistilled water at 37 °C, the concentration determined by photometry at 220 nm. For statistical purposes, the mean and standard deviation were calculated and analyzed by Origin 9.1 Professional SR1 (OriginLab). Due to low interconnectivity and low porosity, the vacuum loading method was unable to attain complete drug loading of the ceramic granules. The sponge showed an inhomogeneous distribution of βTCP granules. Drug release was high at pH 7.4, at pH 5.0 it practically did not occur. All samples except for the collagen-complex show an initial VAN burst release with a following steady release. Loading with 5 mg/ml concentrated VAN resulted in a higher percentage of available drug being released. However, when loaded with 50 mg/ml, the absolute amount of drug released was higher.
Graphical abstract








Similar content being viewed by others
References
König DP, Peters KM. Fortbildung Osteologie. Darmstadt: Steinkopff; 2006.
Holtom PD, Smith AM. Introduction to Adult Posttraumatic Osteomyelitis of the Tibia. Clin Orthop Relat Res. 1999;360:6–13. https://doi.org/10.1097/00003086-199903000-00003.
Musil HE. Trauma und Carcinom?: Ursache und Folge der Osteomyelitis. Arch Orthop Unf-Chir. 1976;84:257–60. https://doi.org/10.1007/BF00416083.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-Joint Infections. N Engl J Med. 2004;351:1645–54. https://doi.org/10.1056/NEJMra040181.
Darouiche RO. Treatment of infections associated with surgical implants. N Engl J Med. 2004;350:1422–9. https://doi.org/10.1056/NEJMra035415.
Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364:369–79. https://doi.org/10.1016/S0140-6736(04)16727-5.
Niethard FU, Pfeil J, Biberthaler P. Orthopädie und Unfallchirurgie: 78 Tabellen; [inklusive Video CD-ROM]. 6th ed. Stuttgart: Thieme; 2009.
Zimmerli WFU. Classification and microbiology of osteomyelitis. Orthopade. 2004;33:267–72.
Kayser et al. Medizinische Mikrobiologie. Stuttgart: Thieme; 2011.
Cunningham R, Cockayne A, Humphreys H. Clinical and molecular aspects of the pathogenesis of Staphylococcus aureus bone and joint infections. J Med Microbiol. 1996;44:157–64.
Leonova SN, Malyshev VV. Mechanisms of disturbance in regenerative processes in chronic traumatic osteomyelitis. Vestn Ross Akad Med Nauk. 2009;44:13–7.
Jesserer H. Knochenkrankheiten. München: Urban & Schwarzenberg; 1971.
Chen W-H, Jiang L-S, Dai L-Y. Surgical treatment of pyogenic vertebral osteomyelitis with spinal instrumentation. Eur Spine J. 2007;16:1307–16. https://doi.org/10.1007/s00586-006-0251-4.
Tetsworth K, Cierny G. Osteomyelitis Debridement Techniques. Clin Orthop Relat Res. 1999;360:87–96. https://doi.org/10.1097/00003086-199903000-00011.
Kinik H, Karaduman M. Cierny-Mader Type III chronic osteomyelitis: the results of patients treated with debridement, irrigation, VAN beads and systemic antibiotics. Int Orthop. 2008;32:551–8. https://doi.org/10.1007/s00264-007-0342-9.
Parsons B, Strauss E. Surgical management of chronic osteomyelitis. Am J Surg. 2004;188:57–66. https://doi.org/10.1016/S0002-9610(03)00292-7.
Gentry LO. Management of osteomyelitis. Int J Antimicrob Agents. 1997;9:37–42.
Becker DE, Reed KL, Essentials of local anesthetic pharmacology. Anesth Prog. 2006;53:98–109. https://doi.org/10.2344/0003-3006(2006)53[98:EOLAP]2.0.CO;2.
Anand A, Pundir R, Pandian CS, Saraf S, GuptaH.Cefoperazone sodium impregnated polycaprolactone composite implant for osteomyelitis. Indian J Pharm Sci. 2009;71:377–81. https://doi.org/10.4103/0250-474X.57285.
Frommelt L. Principles of systemic antimicrobial therapy in foreign material associated infection in bone tissue, with special focus on periprosthetic infection. Injury. 2006;37:S87–94. https://doi.org/10.1016/j.injury.2006.04.014.
Walenkamp G, Vree T, van Rens T. Gentamicin-PMMA beads. Pharmacokinetic and nephrotoxicological study. Clin Orthop Relat Res. 1986;205:171–83.
Mayr HO, Suedkamp NP, Hammer T, Hein W, Hube R, Roth PV, Bernstein A. Beta-tricalcium phosphate for bone replacement: stability and integration in sheep. J Biomech. 2015;48:1023–31. https://doi.org/10.1016/j.jbiomech.2015.01.040
Sailer HF, Weber FE. Knochenersatzmaterialie. Mund Kiefer Gesicht. 2000;4:384–91.
LeGeros RZ. Calcium phosphates in oral biology and medicine. Basel, New York, NY: Karger; 1991.
McKee MD, Wild LM, Schemitsch EH, Waddell JP. The use of an antibiotic-impregnated, osteoconductive, bioabsorbable bone substitute in the treatment of infected long bone defects: early results of a prospective trial. J Orthop Trauma. 2002;16:622–7.
Gitelis S, Brebach GT. The treatment of chronic osteomyelitis with a biodegradable antibiotic-impregnated implant. J Orthop Surg (Hong Kong). 2002;10:53–60.
Otsuka M. Drug release from a novel self-setting bioactive glass bone cement containing cephalexin and its physicochemical properties. J Biomed Mater Res. 1995;29:33–8.
Radin S, Campbell J, Ducheyne P, Cuckler J. Calcium phosphate ceramic coating as VAN carriers. Biomaterials. 1997;18:777–82.
Nandi SK, Mukherjee P, Roy S, Kundu B, De DK, Basu D. Local antibiotic delivery systems for the treatment of osteomyelitis – A review. Mater Sci Eng: C. 2009;29:2478–85. https://doi.org/10.1016/j.msec.2009.07.014.
Kanellakopoulou K, Giamarellos-Bourboulis E. Carrier systems for the local delivery of antibiotics in bone infections. Drugs. 2000;59:1223.
Epple M. Biomaterialien und Biomineralisation: Eine Einführung für Naturwissenschaftler, Mediziner und Ingenieure. Wiesbaden: Vieweg+Teubner Verlag; 2003.
Uchida A, Nade S, McCartney E, Ching W. The use of ceramics for bone replacement. A comparative study of three different porous ceramics. J Bone Jt Surg Br. 1984;66:269–75.
Klawitter JJ, Hulbert SF. Application of porous ceramics for the attachment of load bearing internal orthopedic applications. J Biomed Mater Res Symp. 1971;2:161–229.
Lu J. Role of interconnections in porous bioceramics on bone recolonization in vitro and in vivo. J Mater Sci Mater Med. 1999;10:111–20.
Chang B. Osteoconduction at porous hydroxyapatite with various pore configurations. Biomaterials. 2000;21:1291–8.
Baino F, Vitale-Brovarone C. Three-dimensional glass-derived scaffolds for bone tissue engineering: current trends and forecasts for the future. J Biomed Mater Res A. 2011;97:514–35. https://doi.org/10.1002/jbm.a.33072.
El-Ghannam A. Bone reconstruction: from bioceramics to tissue engineering. Expert Rev Med Devices. 2005;2:87–101. https://doi.org/10.1586/17434440.2.1.87.
Kundu B, Lemos A, Soundrapandian C, Sen PS, Datta S, Ferreira JMF, Basu D. Development of porous HAp and β-TCP scaffolds by starch consolidation with foaming method and drug-chitosan bilayered scaffold based drug delivery system. J Mater Sci Mater Med. 2010;21:2955–69. https://doi.org/10.1007/s10856-010-4127-0.
Hidayat LK, Hsu D, Quist, Shriner R, Wong-Beringer KA, High-dose A. VAN therapy for methicillin-resistant Staphylococcus aureus infections: efficacy and toxicity. Arch Intern Med. 2006;166:2138–44. https://doi.org/10.1001/archinte.166.19.2138.
Mader JT. Antibiotic therapy for musculoskeletal infections: American Volume. J Bone Jt Surg. 2001;83:1878–90.
Huang X, Brazel CS. On the importance and mechanisms of burst release in matrix-controlled drug delivery systems. J Control Release. 2001;73:121–36. https://doi.org/10.1016/S0168-3659(01)00248-6.
El-Ghannam A, Jahed K, Govindaswami M. Resorbable bioactive ceramic for treatment of bone infection. J Biomed Mater Res A. 2010;94:308–16. https://doi.org/10.1002/jbm.a.32705.
Silverman LD, Lukashova L, Herman OT, Lane JM, Boskey AL. Release of gentamicin from a tricalcium phosphate bone implant. J Orthop Res. 2007;25:23–9. https://doi.org/10.1002/jor.20284.
Eitenmüller J. Die Freisetzungsverzögerung verschiedener Antibiotica aus resorbierbarem Tricalciumphosphat-Keramikgranulat durch die Verwendung löslicher Überzüge zur lokalen Behandlung der Osteomyelitis. Lange Arch für Chir. 1983;360:193–206. https://doi.org/10.1007/BF01259235.
Seidenstücker M, Mrestani Y, Neubert RHH, Bernstein A, Mayr HO. Release kinetics and antibacterial efficacy of microporous -TCP coatings. J Nanomater. 2013;2013:1–8. https://doi.org/10.1155/2013/842951.
Itokazu M, Yang W, Aoki T, Ohara A, Kato N. Synthesis of antibiotic-loaded interporous hydroxyapatite blocks by vacuum method and in vitro drug release testing. Biomaterials. 1998;19:817–9.
Laurent F, Bignon A, Goldnadel J, Chevalier J, Fantozzi G, Viguier E, et al. A new concept of gentamicin loaded HAP/TCP bone substitute for prophylactic action: in vitro release validation. J Mater Sci Mater Med. 2008;19:947–51. https://doi.org/10.1007/s10856-007-0163-9.
DiCicco M, Goldfinger A, Guirand F, Abdullah A, Jansen SA. In vitro tobramycin elution analysis from a novel beta-tricalcium phosphate-silicate-xerogel biodegradable drug-delivery system. J Biomed Mater Res Part B Appl Biomater. 2004;70:1–20. https://doi.org/10.1002/jbm.b.30014.
Faigle G. Zur Antibiotikafreisetzung aus Calciumphosphat-Kermikgranulaten: Dissertation. School of Medicine, Universität Freiburg. Submitted. 2016.
Curasan AG. Datenblatt CerasorbM®-Granulat. 2nd edn. 2007. http://curasaninc.com/products.
Curasan AG. Datenblatt OsBone®. 3rd edn. 2009. http://curasaninc.com/products.
Curasan AG. Datenblatt Osseolive®. 2nd edn. 2010. http://curasaninc.com/products.
Curasan AG. Datenlatt CeraCell®. 5th edn. 2011. http://curasaninc.com/products.
Pastorino D, Canal C, Ginebra M-P. Drug delivery from injectable calcium phosphate foams by tailoring the macroporosity–drug interaction. Acta Biomater. 2015;12:250–9. https://doi.org/10.1016/j.actbio.2014.10.031.
Otsuki B, Takemoto M, Fujibayashi S, Neo M, Kokubo T, Nakamura T. Pore throat size and connectivity determine bone and tissue ingrowth into porous implants: three-dimensional micro-CT based structural analyses of porous bioactive titanium implants. Biomaterials. 2006;27:5892–900. https://doi.org/10.1016/j.biomaterials.2006.08.013.
Canal C, Pastorino D, Mestres G, Schuler P, Ginebra MP. Relevance of microstructure for the early antibiotic release of fresh and pre-set calcium phosphate cements. Acta Biomater. 2013;9:8403–12. https://doi.org/10.1016/j.actbio.2013.05.016.
Dorozhkin SV. Calcium orthophosphate cements for biomedical application. J Mater Sci. 2008;43:3028–57. https://doi.org/10.1007/s10853-008-2527-z.
Seidenstücker M. Herstellung eines Kompositmaterials bestehend aus einer porösen ß-Tricalciumphosphatkeramik und einem Drug-Release-System mit kontinuierlicher Wirkstofffreisetzung [Dissertation]. Freiburg i. Br.: Albert-Ludwigs-Universität; 2015. https://doi.org/10.6094/UNIFR/10383.
Kundu B, Soundrapandian C, Nandi SK, Mukherjee P, Dandapat N, Roy S, et al. Development of new localized drug delivery system based on ceftriaxone-sulbactam composite drug impregnated porous hydroxyapatite: a systematic approach for in vitro and in vivo animal trial. Pharm Res. 2010;27:1659–76. https://doi.org/10.1007/s11095-010-0166-y.
Sasaki T, Ishibashi Y, Katano H, Nagumo A, Toh S. In vitro elution of VAN from calcium phosphate cement. J Arthroplast. 2005;20:1055–9. https://doi.org/10.1016/j.arth.2005.03.035.
Suchy T, Supova M, Klapkova E, Horny L, Ryglova S, Zaloudkova M, et al. The Sustainable release of VAN and its degradation products from nanostructured collagen/hydroxyapatite composite layers. J Pharm Sci. 2016;105:1288–94. https://doi.org/10.1016/S0022-3549(15)00175-6.
Stigter M, Bezemer J, Groot K, de, Layrolle P. Incorporation of different antibiotics into carbonated hydroxyapatite coatings on titanium implants, release and antibiotic efficacy. J Control Release. 2004;99:127–37. https://doi.org/10.1016/j.jconrel.2004.06.011.
Brinkrolf P, Klaas C, Horn D. Medikationsfehler in der Intensivmedizin. Intensivmed up2date. 2015;11:125–40. https://doi.org/10.1055/s-0041-101463.
Sedláček O, Studenovský M, Větvička D, Ulbrich K, Hrubý M. Fine tuning of the pH-dependent drug release rate from polyHPMA-ellipticinium conjugates. Bioorg & Med Chem. 2013;21:5669–72. https://doi.org/10.1016/j.bmc.2013.07.038.
Acknowledgements
The authors express their gratitude to Curasan for the provision of the materials. The authors also wish to thank Frank Syrowatka from the interdisciplinary center of materials science (CMAT) of the Martin Luther University of Halle for the EDX measurements. The authors extend their gratitude to Prof. Mülhaupt's group at the Freiburg Materials Research Center (FMF) for their support in measuring porosity as well as to Dr. Simon Procz at the Freiburg Materials Research Center (FMF) for the µCT measurements. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Faigle, G., Bernstein, A., Suedkamp, N.P. et al. Release behavior of VAN from four types of CaP-ceramic granules using various loading methods at two different degrees of acidity. J Mater Sci: Mater Med 29, 12 (2018). https://doi.org/10.1007/s10856-017-6006-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-017-6006-4