Abstract
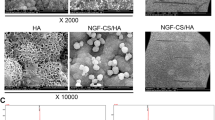
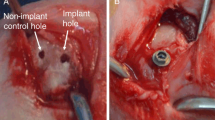
Dental implants are an established therapy for oral rehabilitation. High success rates are achieved in healthy bone, however, these rates decrease in compromised host bone. Coating of dental implants with components of the extracellular matrix is a promising approach to enhance osseointegration in compromised peri-implant bone. Dental titanium implants were coated with an artificial extracellular matrix (aECM) consisting of collagen type I and either one of two regioselectively low sulfated hyaluronan (sHA) derivatives (coll/sHA1Δ6s and coll/sHA1) and compared to commercial pure titanium implants (control). After extraction of the premolar teeth, 36 implants were inserted into the maxilla of 6 miniature pigs (6 implants per maxilla). The healing periods were 4 and 8 weeks, respectively. After animal sacrifice, the samples were evaluated histomorphologically and histomorphometrically. All surface states led to a sufficient implant osseointegration after 4 and 8 weeks. Inflammatory or foreign body reactions could not be observed. After 4 weeks of healing, implants coated with coll/sHA1Δ6s showed the highest bone implant contact (BIC; coll/sHA1Δ6s: 45.4 %; coll/sHA1: 42.2 %; control: 42.3 %). After 8 weeks, a decrease of BIC could be observed for coll/sHA1Δ6s and controls (coll/sHA1Δ6s: 37.3 %; control: 31.7 %). For implants coated with coll/sHA1, the bone implant contact increased (coll/sHA1: 50.8 %). Statistically significant differences could not be observed. Within the limits of the current study, aECM coatings containing low sHA increase peri-implant bone formation around dental implants in maxillary bone compared to controls in the early healing period.





Similar content being viewed by others
References
Buser D, Janner SFM, Wittneben J, Bragger U, Ramseier CA, Salvi GE. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012. doi:10.1111/j.1708-8208.2012.00456.x.
Alsaadi G, Quirynen M, Komarek A, van Steenberghe D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J Clin Periodontol. 2007. doi:10.1111/j.1600-051X.2007.01077.x.
Branemark PI, Hansson BO, Adell R, Breine U, Lindstrom J, Hallen O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132.
Prince CW, Navia JM. Glycosaminoglycan alterations in rat bone due to growth and fluorosis. J Nutr. 1983;113(8):1576–82.
Taylor KR, Gallo RL. Glycosaminoglycans and their proteoglycans: host-associated molecular patterns for initiation and modulation of inflammation. FASEB J. 2006. doi:10.1096/fj.05-4682rev.
Almond A. Hyaluronan. Cell Mol Life Sci. 2007. doi:10.1007/s00018-007-7032-z.
Takahashi K, Goomer RS, Harwood F, Kubo T, Hirasawa Y, Amiel D. The effects of hyaluronan on matrix metalloproteinase-3 (MMP-3), interleukin-1β(IL-1β), and tissue inhibitor of metalloproteinase-1 (TIMP-1) gene expression during the development of osteoarthritis. Osteoarthr Cartil. 1999. doi:10.1053/joca.1998.0207.
Toole BP. Hyaluronan in morphogenesis. Semin Cell Dev Biol. 2001. doi:10.1006/scdb.2000.0244.
Sasaki T, Watanabe C. Stimulation of osteoinduction in bone wound healing by high-molecular hyaluronic acid. Bone. 1995;16(1):9–15.
Nagahata M, Tsuchiya T, Ishiguro T, Matsuda N, Nakatsuchi Y, Teramoto A, Hachimori A, Abe K. A novel function of N-cadherin and Connexin43: marked enhancement of alkaline phosphatase activity in rat calvarial osteoblast exposed to sulfated hyaluronan. Biochem Biophys Res Commun. 2004. doi:10.1016/j.bbrc.2004.01.098.
Hintze V, Moeller S, Schnabelrauch M, Bierbaum S, Viola M, Worch H, Scharnweber D. Modifications of hyaluronan influence the interaction with human bone morphogenetic protein-4 (hBMP-4). Biomacromolecules. 2009. doi:10.1021/bm9008827.
Hintze V, Miron A, Moeller S, Schnabelrauch M, Wiesmann H, Worch H, Scharnweber D. Sulfated hyaluronan and chondroitin sulfate derivatives interact differently with human transforming growth factor-β1 (TGF-β1). Acta Biomater. 2012. doi:10.1016/j.actbio.2012.03.021.
Hempel U, Moller S, Noack C, Hintze V, Scharnweber D, Schnabelrauch M, Dieter P. Sulfated hyaluronan/collagen I matrices enhance the osteogenic differentiation of human mesenchymal stromal cells in vitro even in the absence of dexamethasone. Acta Biomater. 2012. doi:10.1016/j.actbio.2012.06.039.
Hess R, Jaeschke A, Neubert H, Hintze V, Moeller S, Schnabelrauch M, Wiesmann H, Hart DA, Scharnweber D. Synergistic effect of defined artificial extracellular matrices and pulsed electric fields on osteogenic differentiation of human MSCs. Biomaterials. 2012. doi:10.1016/j.biomaterials.2012.08.056.
Hintze V, Miron A, Moller S, Schnabelrauch M, Heinemann S, Worch H, Scharnweber D. Artificial extracellular matrices of collagen and sulphated hyaluronan enhance the differentiation of human mesenchymal stem cells in the presence of dexamethasone. J Tissue Eng Regen Med. 2012. doi:10.1002/term.1528.
Kliemt S, Lange C, Otto W, Hintze V, Moller S, von Bergen M, Hempel U, Kalkhof S. Sulfated hyaluronan containing collagen matrices enhance cell-matrix-interaction, endocytosis, and osteogenic differentiation of human mesenchymal stromal cells. J Proteome Res. 2013. doi:10.1021/pr300640h.
Salbach J, Kliemt S, Rauner M, Rachner TD, Goettsch C, Kalkhof S, von Bergen M, Moller S, Schnabelrauch M, Hintze V, Scharnweber D, Hofbauer LC. The effect of the degree of sulfation of glycosaminoglycans on osteoclast function and signaling pathways. Biomaterials. 2012. doi:10.1016/j.biomaterials.2012.08.028.
Franz S, Allenstein F, Kajahn J, Forstreuter I, Hintze V, Moller S, Simon JC. Artificial extracellular matrices composed of collagen I and high-sulfated hyaluronan promote phenotypic and functional modulation of human pro-inflammatory M1 macrophages. Acta Biomater. 2013. doi:10.1016/j.actbio.2012.11.016.
Kunze R, Rosler M, Moller S, Schnabelrauch M, Riemer T, Hempel U, Dieter P. Sulfated hyaluronan derivatives reduce the proliferation rate of primary rat calvarial osteoblasts. Glycoconj J. 2010. doi:10.1007/s10719-009-9270-9.
Becher J, Möller S, Weiss D, Schiller J, Schnabelrauch M. Synthesis of new regioselectively sulfated hyaluronans for biomedical application. Macromol Symp. 2010;269:446–52.
Bierbaum S, Douglas T, Hanke T, Scharnweber D, Tippelt S, Monsees TK, Funk RHW, Worch H. Collageneous matrix coatings on titanium implants modified with decorin and chondroitin sulfate: characterization and influence on osteoblastic cells. J Biomed Mater Res A. 2006. doi:10.1002/jbm.a.30572.
Junqueira LC, Bignolas G, Mourao PA, Bonetti SS. Quantitation of collagen-proteoglycan interaction in tissue sections. Connect Tissue Res. 1980;7(2):91–6.
Walsh BJ, Thornton SC, Penny R, Breit SN. Microplate reader-based quantitation of collagens. Anal Biochem. 1992;203(2):187–90.
Farndale RW, Buttle DJ, Barrett AJ. Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue. Biochim Biophys Acta. 1986;883(2):173–7.
Donath K, Breuner G. A method for the study of undecalcified bones and teeth with attached soft tissues. The Sage-Schliff (sawing and grinding) technique. J Oral Pathol. 1982;11(4):318–26.
Friberg B, Jemt T, Lekholm U. Early failures in 4,641 consecutively placed Brånemark dental implants: a study from stage 1 surgery to the connection of completed prostheses. Int J Oral Maxillofac Implants. 1991;6(2):142–6.
Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991. doi:10.1902/jop.1991.62.1.2.
Schliephake H, Aref A, Scharnweber D, Bierbaum S, Sewing A. Effect of modifications of dual acid-etched implant surfaces on peri-implant bone formation. Part I: organic coatings. Clin Oral Implants Res. 2009. doi:10.1111/j.1600-0501.2008.01603.x.
Stadlinger B, Pilling E, Huhle M, Mai R, Bierbaum S, Bernhardt R, Scharnweber D, Kuhlisch E, Hempel U, Eckelt U. Influence of extracellular matrix coatings on implant stability and osseointegration: an animal study. J Biomed Mater Res Part B Appl Biomater. 2007. doi:10.1002/jbm.b.30787.
Stadlinger B, Hintze V, Bierbaum S, Moller S, Schulz MC, Mai R, Kuhlisch E, Heinemann S, Scharnweber D, Schnabelrauch M, Eckelt U. Biological functionalization of dental implants with collagen and glycosaminoglycans-a comparative study. J Biomed Mater Res A. 2011. doi:10.1002/jbm.b.31953.
Wang S, Liu Y, Fang D, Shi S. The miniature pig: a useful large animal model for dental and orofacial research. Oral Dis. 2007. doi:10.1111/j.1601-0825.2006.01337.x.
Weaver ME, Sorenson FM, Jump EB. The miniature pig as an experimental animal in dental research. Arch Oral Biol. 1962;7:17–23.
Misch CE. Density of bone: effect on treatment plans, surgical approach, healing, and progressive boen loading. Int J Oral Implantol. 1990;6(2):23–31.
Germanier Y, Tosatti S, Broggini N, Textor M, Buser D. Enhanced bone apposition around biofunctionalized sandblasted and acid-etched titanium implant surfaces. A histomorphometric study in miniature pigs. Clin Oral Implants Res. 2006. doi:10.1111/j.1600-0501.2005.01222.x.
Hermann JS, Jones AA, Bakaeen LG, Buser D, Schoolfield JD, Cochran DL. Influence of a machined collar on crestal bone changes around titanium implants: a histometric study in the canine mandible. J Periodontol. 2011. doi:10.1902/jop.2011.090728.
Bernhardt R, Kuhlisch E, Schulz MC, Eckelt U, Stadlinger B. Comparison of bone-implant contact and bone-implant volume between 2D-histological sections and 3D-SRmicroCT slices. Eur Cell Mater. 2012;23:237–47 discussion 247–8.
Rammelt S, Illert T, Bierbaum S, Scharnweber D, Zwipp H, Schneiders W. Coating of titanium implants with collagen. RGD peptide and chondroitin sulfate. Biomaterials. 2006. doi:10.1016/j.biomaterials.2006.06.034.
Kajahn J, Franz S, Rueckert E, Forstreuter I, Hintze V, Moeller S, Simon JC. Artificial extracellular matrices composed of collagen I and high sulfated hyaluronan modulate monocyte to macrophage differentiation under conditions of sterile inflammation. Biomatter. 2012. doi:10.4161/biom.22855.
Astachov L, Vago R, Aviv M, Nevo Z. Hyaluronan and mesenchymal stem cells: from germ layer to cartilage and bone. Front Biosci. 2011;16:261–76.
Bastow ER, Byers S, Golub SB, Clarkin CE, Pitsillides AA, Fosang AJ. Hyaluronan synthesis and degradation in cartilage and bone. Cell Mol Life Sci. 2008. doi:10.1007/s00018-007-7360-z.
Itoh S, Matubara M, Kawauchi T, Nakamura H, Yukitake S, Ichinose S, Shinomiya K. Enhancement of bone ingrowth in a titanium fiber mesh implant by rhBMP-2 and hyaluronic acid. J Mater Sci Mater Med. 2001;12(7):575–81.
Morra M, Cassinelli C, Cascardo G, Fini M, Giavaresi G, Giardino R. Covalently-linked hyaluronan promotes bone formation around Ti implants in a rabbit model. J Orthop Res. 2009. doi:10.1002/jor.20797.
Stadlinger B, Bierbaum S, Grimmer S, Schulz MC, Kuhlisch E, Scharnweber D, Eckelt U, Mai R. Increased bone formation around coated implants. J Clin Periodontol. 2009. doi:10.1111/j.1600-051X.2009.01435.x.
Rutten S, Nolte PA, Korstjens CM, van Duin MA, Klein-Nulend J. Low-intensity pulsed ultrasound increases bone volume, osteoid thickness and mineral apposition rate in the area of fracture healing in patients with a delayed union of the osteotomized fibula. Bone. 2008. doi:10.1016/j.bone.2008.04.010.
Terheyden H, Lang NP, Bierbaum S, Stadlinger B. Osseointegration–communication of cells. Clin Oral Implants Res. 2012. doi:10.1111/j.1600-0501.2011.02327.x.
Acknowledgments
The study was supported by the Transregio 67 grant of the German Research Foundation DFG (A2, A3, B6). The implants were donated by Thommen Medical AG, Waldenburg, Switzerland. The authors are grateful to Dr. Roland Jung and Dr. Kathrin Spekl for their support during the animal experiments. Furthermore, the authors wish to thank Diana Jünger, Heike Zimmermann and Sarah Beckmann for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schulz, M.C., Korn, P., Stadlinger, B. et al. Coating with artificial matrices from collagen and sulfated hyaluronan influences the osseointegration of dental implants. J Mater Sci: Mater Med 25, 247–258 (2014). https://doi.org/10.1007/s10856-013-5066-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-013-5066-3