Abstract
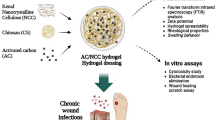
Chronic wounds are a major cause for both suffering and economical losses. Management of chronic non-healing wounds requires multipronged approach. They are polymicrobial and agonizing for the patient due to associated pain. Moist dressing providing antimicrobial action is a highly desirable chronic wound management option. Here we report a hydrogel based dressing that possesses the antimicrobial properties of acidified sodium nitrite and the homeostatic property of a hydrogel. The dressing was developed by combining citric acid cross-linked cotton gauze and sodium nitrite loaded gelatin. The cotton gauze was cross-linked with citric acid by pad-dry-curing in presence of nano-titania catalyst. The cotton gauze-gelatin hydrogel combination was gamma-irradiated and freeze-dried. At the time of application, the freeze-dried dressing is wetted by sodium nitrite solution. The dressing has a fluid uptake ability of 90 % (w/v) and the water vapour evaporation rate was estimated to be 2,809 ± 20 g/m2/day. The dressing showed significant antimicrobial activity against both planktonic and biofilm forms and was effective during consecutive re-uses. Cytotoxicity study showed inhibition of fibroblasts, but to a lesser extent than clinically administered concentrations of antiseptic like povidone iodine. Storage at 37 °C over a 3 month period resulted in no significant loss of its antimicrobial activity.





Similar content being viewed by others
References
Markova A, Mostow EN. US Skin disease assessment: ulcer and wound care. Dermatol Clin. 2012;30(1):107–11.
Ammons MCB. Anti-biofilm strategies and the need for innovations in wound care. Recent Pat Anti-infect Drug Discov. 2010;5:10–7.
Fonseca AP. Biofilms in wounds: an unsolved problem? EWMA J. 2011;11:10–23.
Hampton S, Collins F. Tissue viability a comprehensive guide. London: Whurr Publications; 2007.
White RJ, Cutting K, Kingsley A. Topical antimicrobials in the control of wound bioburden. Ostomy Wound Manag. 2006;52(8):26–58.
Bechtle M, Chen S, Efferth T. Neglected diseases caused by bacterial infections. Curr Med Chem. 2010;19:42–60.
Ghaffari A, Miller CC, McMullin B, Ghahary A. Potential application of gaseous nitric oxide as a topical antimicrobial agent. Nitric Oxide. 2006;14(1):21–9.
Davey ME, O’toole GA. Microbial biofilms: from ecology to molecular genetics. Microbiol Mol Biol Rev. 2000;64(4):847–67.
Davies D. Understanding biofilm resistance to antibacterial agents. Nat Rev Drug Discov. 2003;2(2):114–22.
Sternberg C, Christensen BB, Johansen T, Nielsen AT, Andersen JB, Givskov M. Distribution of bacterial growth activity in flow-chamber biofilms. Appl Environ Microbiol. 1999;65(9):4108–17.
Kevil CG, Kolluru GK, Pattillo CB, Giordano T. Inorganic nitrite therapy: historical perspective and future directions. Free Radic Biol Med. 2011;51(3):576–93.
Phillips R, Kuijper S, Benjamin N, Wansbrough-Jones M, Wilks M, Kolk AHJ. In vitro killing of Mycobacterium ulcerans by acidified nitrite. Antimicrob Agents Chemother. 2004;48(8):3130–2.
Phillips R, Adjei O, Lucas S, Benjamin N, Wansbrough-Jones M. Pilot randomized double-blind trial of treatment of Mycobacterium ulcerans disease (Buruli ulcer) with topical nitrogen oxides. Antimicrob Agents Chemother. 2004;48(8):2866–70.
Martinez-Ruiz A, Lamas S. S-nitrosylation: a potential new paradigm in signal transduction. Cardiovasc Res. 2004;62:43–52.
Fang FC. Perspectives series: host-pathogen interactions. Mechanisms of nitric oxide-related antimicrobial activity. J Clin Investig. 1997;99(12):2818–25.
Ormerod AD, White MI, Shah SA, Benjamin N. Molluscum contagiosum effectively treated with a topical acidified nitrite, nitric oxide liberating cream. Braz J Dermatol. 1999;141(6):1051–3.
Weller R, Ormerod AD, Hobson RP, Benjamin NJ. A randomized trial of acidified nitrite cream in the treatment of tinea pedis. J Am Acad Dermatol. 1998;38(4):559–63.
Flanagan M. Wound management. Philadelphia: Elsevier Health Sciences; 1997.
Fleck CA. Wound pain: assessment and management. Wound Care Canada. 2007;5(1):10–7.
Nazari A, Montazer M, Rashidi A, Yazdanshenas M, Anary-Abbasinejad M. Nano TiO2 photo-catalyst and sodium hypophosphite for cross-linking cotton with poly carboxylic acids under UV and high temperature. Appl Catal A. 2009;371(1–2):10–6.
Quinn KJ, Courtney JM, Evans JH, Gaylor JDS, Reid WH. Principles of burn dressings. Biomaterials. 1985;6(6):369–77.
Balakrishnan B, Mohanty M, Umashankar PR, Jayakrishnan A. Evaluation of an in situ forming hydrogel wound dressing based on oxidized alginate and gelatin. Biomaterials. 2005;26(32):6335–42.
Phillips R, Adjei O, Lucas S, Benjamin N, Wansbrough-Jones M. Pilot randomized double-blind trial of treatment of Mycobacterium ulcerans disease (Buruli ulcer) with topical nitrogen oxides. Antimicrob Agents Chemother. 2004;48(8):2866–70.
Kim IY, Yoo MK, Seo JH, Park SS, Na HS, Lee HC, et al. Evaluation of semi-interpenetrating polymer networks composed of chitosan and poloxamer for wound dressing application. Int J Pharm. 2007;341(1–2):35–43.
Diggle SP, Griffin AS, Campbell GS, West SA. Cooperation and conflict in quorum-sensing bacterial populations. Nature. 2007;450(7168):411–4.
Trotonda MP, Manna AC, Cheung AL, Lasa I, Penadés JR. SarA positively controls bap-dependent biofilm formation in Staphylococcus aureus. J Bacteriol. 2005;187(16):5790–8.
Hetrick EM, Shin JH, Paul HS, Schoenfisch MH. Anti-biofilm efficacy of nitric oxide-releasing silica nanoparticles. Biomaterials. 2009;30(14):2782–9.
Lee RJ, Low PS. Folate-mediated tumor cell targeting of liposome-entrapped doxorubicin in vitro. Biochim Biophys Acta. 1995;1233(2):134–44.
Anyim M, Benjamin N, Wilks M. Acidified nitrite as a potential antifungal agent. Int J Antimicrob Agents. 2005;26(1):85–7.
Carlsson S, Govoni M, Wiklund NP, Weitzberg E, Lundberg JO. In vitro evaluation of a new treatment for urinary tract infections caused by nitrate-reducing bacteria. Antimicrob Agents Chemother. 2003;47(12):3713–8.
Lamke LO, Nilsson GE, Reithner HL. The evaporative water loss from burns and the water-vapour permeability of grafts and artificial membranes used in the treatment of burns. Burns. 1977;3(3):159–65.
Kickhöfen B, Wokalek H, Scheel D, Ruh H. Chemical and physical properties of a hydrogel wound dressing. Biomaterials. 1986;7(1):67–72.
Dalton T, Dowd SE, Wolcott RD, Sun Y, Watters C, Griswold JA, et al. An in vivo polymicrobial biofilm wound infection model to study interspecies interactions. PLoS One. 2011;6(11):e27317. doi:10.1371/journal.pone.0027317.
Siddiqui AR, Bernstein JM. Chronic wound infection: facts and controversies. Clin Dermatol. 2010;28(5):519–26.
Lexchin J. Promoting resistance? Essential Drugs Monitor. 2000;28&29:11.
Dryden M, Johnson AP, Ashiru-Oredope D, Sharland M. Using antibiotics responsibly: right drug, right time, right dose, right duration. J Antimicrob Chemother. 2011;66(11):2441–3.
Davis SC, Martinez L, Kirsner R. The diabetic foot: the importance of biofilms and wound bed preparation. Curr Diab Rep. 2006;6(6):439S–45S.
Anthony WS. Biofilms and antibiotic therapy: Is there a role for combating bacterial resistance by the use of novel drug delivery systems? Adv Drug Deliv Rev. 2005;57(10):1539–50.
Werner S, Krieg T, Smola H. Keratinocyte–fibroblast interactions in wound healing. J Invest Dermatol. 2007;127(5):998–1008.
Wong T, McGrath JA, Navsaria H. The role of fibroblasts in tissue engineering and regeneration. Braz J Dermatol. 2007;156(6):1149–55.
Weyermann J, Lochmann D, Zimmer A. A practical note on the use of cytotoxicity assays. Int J Pharm. 2005;288(2):369–76.
Pyo HC, Kim YK, Whang KU, Park YL, Eun HC. A comparative study of cytotoxicity of topical antimicrobials to cultured human keratinocytes and fibroblasts. Korean J Dermatol. 1995;33(5):895–906.
Du Toit DF, Page BJ. An in vitro evaluation of the cell toxicity of honey and silver dressings. J Wound Care. 2009;18(9):383–9.
Lam PK, Chan ES, Ho WS, Liew CT. In vitro cytotoxicity testing of a nanocrystalline silver dressing (Acticoat) on cultured keratinocytes. Braz J Biomed Sci. 2004;61(3):125–7.
Liu X, Zhu YK, Wang H, Kohyama T, Wen F, Rennard SI. Effect of nitric oxide donors on human lung fibroblast proliferation in vitro. Chest. 2001;120(1 suppl):S13–4.
Espey DK, Djomand G, Diomande I, Dosso M, Saki MZ, Kanga J-M, et al. Pilot study of treatment of Buruli ulcer with rifampin and dapsone. Int J Infect Dis. 2002;6(1):60–5.
Acknowledgments
The authors acknowledge their colleague Dr. Pushpalata Rajesh for her help in the irradiation facility. We are also thankful to Dr. Iñigo Lasa, Instituto De Agrobiotecnologia, Universidad Publica de Navarra/Consejo Superior de Investigaciones Científicas, Campus de Arrosadia, Spain for providing us Staphylococcus aureus strain and Prof. Stephen P. Diggle, Institute of Infection, Immunity and Inflammation, Centre for Biomolecular Sciences, University Park, University of Nottingham, Nottingham, UK for providing us with Pseudomonas aeruginosa strain. The customer service cell, Biomedical Technology Wing at Sree Chitra Tirunal Institute for Medical Sciences & Technology (SCTIMST), Trivandrum for the cell-cytotoxicity analysis and Evonik Industries, Germany for the nano-titania catalyst are acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dave, R.N., Joshi, H.M. & Venugopalan, V.P. Biomedical evaluation of a novel nitrogen oxides releasing wound dressing. J Mater Sci: Mater Med 23, 3097–3106 (2012). https://doi.org/10.1007/s10856-012-4766-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4766-4