Abstract
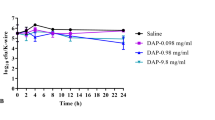
The reduction of implant related infections plays a pivotal role in orthopaedic surgery as an increasing number of people require implants (up to 200,000 per year in the United States (source: Joint Implant Surgery & Research Foundation 2010)). The aim of the current study is to prevent and thus decrease the number of bacterial infections. Both pre and post operative systemic antibiotic treatment and gentamicin containing bone cements (polymethylmethacrylate, PMMA) are commonly used strategies to overcome infections. In this study, the antimicrobial efficacy of gentamicin sulfate loaded bone cement was compared with titan discs coated with a new form of gentamicin, gentamicin palmitate. Adherence prevention, killing rates and killing kinetics were compared in an in vitro model, using Staphylococcus aureus (S. aureus), which together with Staphylococcus epidermidis (S. epidermidis) represents 60% of bacteria found responsible for hip implant infections (An and Friedman, 1996, J Hosp Infect 33(2):93–108). In our experiments gentamicin, which was applied as gentamicin palmitate on the surface of the implants, showed a high efficacy in eliminating bacteria. In contrast to gentamicin sulfate containing bone cements, gentamicin palmitate is released over a shorter period of time thus not inducing antibiotic resistance. Another benefit for clinical application is that it achieves high local levels of active ingredient which fight early infections and minimize toxic side effects. Furthermore, the short term hydrophobic effect of gentamicin palmitate can successfully impede biofilm formation. Thus, the use of self-adhesive antibiotic fatty acid complexes like gentamicin palmitate represents a new option for the anti-infective coating of cementless titan implants.


Similar content being viewed by others
Abbreviations
- Ti1a/Ti1b:
-
Titan discs with high/low concentration of gentamicin palmitate
- Ti2a/Ti2b:
-
Titan discs with high/low concentration of gentamicin palmitate
- Ti3a/Ti3b:
-
Titan discs with high/low concentration of gentamicin palmitate
- PMMA1:
-
Commercially available bone cement without gentamicin
- PMMA2:
-
Commercially available bone cement with gentamicin sulfate
References
Kadurugamuwa JL, Clarke AJ, Beveridge TJ. Surface action of gentamicin on Pseudomonas aeruginosa. J Bacteriol. 1993;175(18):5798–805.
Abou-Zeid AA, Shehata YM. Gentamicins. Zentralbl Bakteriol Parasitenkd Infektionskr Hyg. 1977;132(2):97–108.
Gillespie WJ, Walenkamp GH. Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database Syst Rev. 2010;3:CD000244.
Dunbar MJ. Antibiotic bone cements: their use in routine primary total joint arthroplasty is justified. Orthopedics 2009;32(9):10.3928/01477447-20090728-20.
Buchholz HW, Engelbrecht H. Depot effects of various antibiotics mixed with Palacos resins. Chirurg. 1970;41(11):511–5.
Wahlig H, Dingeldein E. Antibiotics and bone cements. Experimental and clinical long-term observations. Acta Orthop Scand. 1980;51(1):49–56.
van Loosdrecht MC, Lyklema J, Norde W, Zehnder AJ. Influence of interfaces on microbial activity. Microbiol Rev. 1990;54(1):75–87.
Clauss M, Trampuz A, Borens O, Bohner M, Ilchmann T. Biofilm formation on bone grafts and bone graft substitutes: comparison of different materials by a standard in vitro test and microcalorimetry. Acta Biomater. 2010;6(9):3791–7.
Erli HJ, Marx R, Paar O, Niethard FU, Weber M, Wirtz DC. Surface pretreatments for medical application of adhesion. Biomed Eng Online. 2003;2:15.
Vogt S, Kühn K-D, Gopp U, Schnabelrauch M. Resorbable antibiotic coatings for bone substitutes and implantable devices. Mat- wiss U Werkstofftechn. 2005;36:814–9.
Anagnostakos K, Wilmes P, Schmitt E, Kelm J. Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivo. Acta Orthop. 2009;80(2):193–7.
Tunney MM, Ramage G, Patrick S, Nixon JR, Murphy PG, Gorman SP. Antimicrobial susceptibility of bacteria isolated from orthopedic implants following revision hip surgery. Antimicrob Agents Chemother. 1998;42(11):3002–5.
Neut D, van de Belt H, van Horn JR, van der Mei HC, Busscher HJ. Residual gentamicin-release from antibiotic-loaded polymethylmethacrylate beads after 5 years of implantation. Biomaterials. 2003;24(10):1829–31.
Kalicke T, Schierholz J, Schlegel U, Frangen TM, Koller M, Printzen G, et al. Effect on infection resistance of a local antiseptic and antibiotic coating on osteosynthesis implants: an in vitro and in vivo study. J Orthop Res. 2006;24(8):1622–40.
Vogt S, Schnabelrauch M, Kühn K-D. Porous implants with antibiotic coating, their preparation and use. Antimicrob Agents Chemother. 2008;52(6):1957–63.
Matl FD, Obermeier A, Repmann S, Friess W, Stemberger A, Kuehn KD. New anti-infective coatings of medical implants. Antimicrob Agents Chemother. 2008;52(6):1957–63.
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1):128–33.
Swanson TE, Cheng X, Friedrich C. Development of chitosan-vancomycin antimicrobial coatings on titanium implants. J Biomed Mater Res A. 2011;97(2):167–76.
Fini M, Giavaresi G, Setti S, Martini L, Torricelli P, Giardino R. Current trends in the enhancement of biomaterial osteointegration: biophysical stimulation. Int J Artif Organs. 2004;27(8):681–90.
Epinette JA, Manley MT. Uncemented stems in hip replacement–hydroxyapatite or plain porous: does it matter? Based on a prospective study of HA Omnifit stems at 15-years minimum follow-up. Hip Int. 2008;18(2):69–74.
Zilberman M, Kraitzer A, Grinberg O, Elsner JJ. Drug-eluting medical implants. Handb Exp Pharmacol. 2010;197:299–341.
Strobel C, Schmidmaier G, Wildemann B. Changing the release kinetics of gentamicin from poly(D,L-lactide) implant coatings using only one polymer. Int J Artif Organs. 2011;34(3):304–16.
El-Husseiny M, Patel S, MacFarlane RJ, Haddad FS. Biodegradable antibiotic delivery systems. J Bone Joint Surg Br. 2011;93(2):151–7.
Parvizi J, Saleh KJ, Ragland PS, Pour AE, Mont MA. Efficacy of antibiotic-impregnated cement in total hip replacement. Acta Orthop. 2008;79(3):335–41.
Kühn K. In vitro release of gentamicinpalmitate coating in uncemented titanium implants. IJNBM. 2010;3(1):94–106.
Schafer JA, Hovde LB, Rotschafer JC. Consistent rates of kill of Staphylococcus aureus by gentamicin over a 6-fold clinical concentration range in an in vitro pharmacodynamic model (IVPDM). J Antimicrob Chemother. 2006;58(1):108–11.
Kühn KD, Brünke J. Effectiveness of a novel gentamicinpalmitate coating on biofilm formation of Staphylococcus aureus and Staphylococcus epidermidis. IJNBM. 2010;3(1):107–17.
Everaert EP, Mahieu HF, Wong Chung RP, Verkerke GJ, van der Mei HC, Busscher HJ. A new method for in vivo evaluation of biofilms on surface-modified silicone rubber voice prostheses. Eur Arch Otorhinolaryngol. 1997;254(6):261–3.
van de Belt H, Neut D, Schenk W, van Horn JR, van der Mei HC, Busscher HJ. Infection of orthopedic implants and the use of antibiotic-loaded bone cements. A review. Acta Orthop Scand. 2001;72(6):557–71.
Hetrick EM, Schoenfisch MH. Reducing implant-related infections: active release strategies. Chem Soc Rev. 2006;35(9):780–9.
An YH, Friedman RJ. Prevention of sepsis in total joint arthroplasty. J Hosp Infect. 1996;33(2):93–108.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kittinger, C., Marth, E., Windhager, R. et al. Antimicrobial activity of gentamicin palmitate against high concentrations of Staphylococcus aureus . J Mater Sci: Mater Med 22, 1447–1453 (2011). https://doi.org/10.1007/s10856-011-4333-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-011-4333-4