Abstract
Rapid re-endothelialization at an atherosclerotic lesion after stent employment is essential for reducing or preventing local thrombus formation and restenosis. To prevent these complications via enhanced rapid re-endothelialization, poly n-butyl methacrylate (PPBMA) coating was deposited on the stent surface through a radio-frequency plasma polymerization process, with oxygen as the carrier gas. Fourier transform infrared (FTIR) spectroscopy and X-ray photoelectron spectroscopy (XPS) characterization confirmed the occurrence of the plasma polymerization and the chemistry properties of the PPBMA. Scanning electron microscopy (SEM) revealed a smooth and dense surface. The wettability of the polymeric films measured by the contact angle indicated that the surface was more hydrophilic (2.0 ± 1°) than the original surface (24 ± 1°) by the introduction of the PPBMA coating, with a slight decrease even after 4 days. The results of the culture of human umbilical cord veins endothelial cells (HUVEC) in vitro showed that compared with the control of 316L stainless steel, the attachment and growth of cells on the PPBMA-coated surface was significantly enhanced, and a confluent endothelial cells layer was formed after a 4-day culture. A platelet adhesion experiment revealed that the blood compatibility of the substrate surface after PPBMA deposition was also obviously improved. The PPBMA coating remained intact on the stent surface after expansion according to the clinic protocol, indicating that the adhesive strength of PPBMA coating was high enough to withstand the external force in the process of stent expansion. This in vitro pilot study prior to in vivo experiments suggested that this plasma PPBMA was promising for coating stent materials for rapid re-endothelialization.
Similar content being viewed by others
1 Introduction
Coronary artery stenting is currently the most frequently performed percutaneous coronary intervention for the treatment of coronary artery disease. A coronary stent implantation, however, always provokes a cascade of cellular and biochemical events that induce pathophysiologic processes such as thrombus formation and the release of cytokines, which trigger the proliferation of smooth muscle cells (SMCs). Thus, the occurrence of reocclusion due to on-stent thrombus formation in the early period and in-stent restenosis in the later period after stent deployment is the principal drawback of coronary angioplasty [1, 2]. Previous studies have revealed that an important factor contributing to this reocclusion at the site of intravascular stent placement is injury to, and loss of, the endothelium [3], which provides an inherent nonthrombogenic potential and interrupts cytokine-driven activation of SMCs in vascular medial tissues, thus playing an integral part in maintaining vascular homeostasis and normal function. Therefore, rapid re-endothelialization of the arterial wall and endothelialization of the intravascular stents’ surface after implantation are of extreme importance [3–5]. For example, Michael et al. reported that if rapid re-endothelialization were achieved, then the stent thrombosis and neointimal hyperplasia would simultaneously be effectively inhibited [3].
To realize a rapid re-endothelialization, many attempts have been made to seed active endothelial cell layers prior to stent implantation, but the results have been mixed and sometimes poor [6, 7]. It turns out that a large part of the seeded cells are lost soon after blood flow is restored. Moreover, pre-seeding of vascular grafts is relatively expensive and time-consuming, and it is not trivial to collect good-quality endothelial cells from patients [1]. Allowing endothelial cells to attach and grow in situ to the grafts under pulsatile flow might be an alternative strategy to solve this problem [8, 9]. Re-endothelialization of the prosthetic surface can be achieved by the migration, attraction and adhesion of surrounding mature endothelial cells and circulating endothelial progenitor cells to the injured region, which then differentiate into endothelial-like cells. However, the intrinsic inert properties of metal, including 316L stainless steel, which is commonly used as vascular grafts, are unfavorable for endothelial cells adhesion and/or growth. So, it is necessary to modify the stent surface to make it suitable for endothelial cell attachment and proliferation, thus accelerating the re-endothelialization.
Many modifications have focused on modulating the interface properties of the implanted biomaterials, such as layer-by-layer assembly [10], coating or grafting adhesive proteins that mediate cellular attachment, such as fibronectin, laminine, collagen and peptides [11], ion implantation [12] and plasma-polymerized thin film [13]. Among these methods, plasma-polymerized thin film has been applied extensively in the biomaterials field because the films produced are very smooth, are pinhole and defect free and have good adhesive properties [14]. Meanwhile, another important advantage of this process is that it is substrate dependent, that is, the plasma-polymerized thin film can be deposited onto any substrate surface including those with complex geometries.
In this respect, we have focused on development of a radio frequency plasma-polymerized n-butyl methacrylate (PPBMA) film on 316L stainless steel to accelerate the re-endothelialization of intravascular devices. Taking account of the fact that gas carriers are well known to modulate the properties of plasma polymer, oxygen was utilized in the plasma deposition. The chemical composition, morphology and wettability of the PPBMA deposited were characterized by Fourier transform infrared (FTIR) spectroscopy, X-ray photoelectron spectroscopy (XPS), scanning electron microscopy (SEM) and static contact angle measurement. And the ‘in vitro’ growth of endothelial cells and the platelet adhesion on the polymerized film surface were investigated. In addition, the adhesion strength between the PPBMA coating and 316L stainless steel stent was also examined. The results of the first-step experiments showed that the PPBMA film, which was formed through this simple plasma polymerization method, could effectively enhance the endothelial cell attachment and growth, demonstrating a promising coating technique for surface modification of the intravascular prosthesis.
2 Materials and methods
2.1 Plasma polymerization
BMA (99.5% purity), used as the monomer in plasma polymerization, was purchased from Shanghai Pharmaceutical Corp. Biomedical 316L stainless steel slides (Shanghai Biomedical Metal Company), 316L stainless steel stents (DeviceTeck Co, USA) and KBr slide were employed as substrates. The biomedical 316L stainless steel slides (1 × 1 cm2) were polished with Buehler Phoenix 4000 to mirror surfaces. The biomedical 316L stainless steel slides and stents were ultrasonically cleaned with acetone and isopropanol for 10 min to remove the surface containments.
The experimental set-up consists of a reactor system, gas flow system and an RF power source (13.56 MHz) with a matching network (Model-SP II), shielding and a vacuum system (Fig. 1). The reactor dimension was 100 × 8 cm2. The substrates were located on the platform in the center of the reaction chamber. Initially, the system was pumped down to a base pressure of 2.0 × 10−2 Pa or less. Prior to BMA deposition, the samples were subjected to brief oxygen plasma (20 Pa, 40 w, 20 s) to clean and activate the surface of the substrates. Following the oxygen plasma treatment, the system was evacuated to a background pressure of 2.0 × 10−2 Pa again. The reaction gases, a mixture of 90 vol.% BMA and 10 vol.% high-purity O2, were then introduced. The flow rate was controlled using mass flow controllers, and the total flow rate was 30 mL/min. After the reactor pressure was stabilized at 20 Pa, plasma was initiated and the output power was kept at 40 w for the deposition time of 30 min. After plasma deposition, the freshly coated specimens were allowed to remain in the presence of monomer gas for 10 min to terminate reactive species on the film surfaces.
2.2 Surface characterization and analysis
The chemical composition of the plasma-generated films on the KBr slides was characterized by FTIR spectrometer (5SXC, Nicolet Inc., USA) in the range of 400−4,000 cm−1 and X-ray photoelectron spectroscopy (MICROLAB MKαII, VG, England). X-rays were generated with an Mg anode at a power of 300 W. A constant take-off angle of 90°with respect to the sample surface was used. The base pressure in the analysis chamber was 1 × 10−6 Pa. The surface charge effect was neutralized by the flood gun. Wide-scan spectra in the 1200.0 eV binding energy range were recorded with a pass energy of 50 eV for all samples. Core level scans were taken for carbon at a pass energy of 0.1 eV. The morphology of the plasma PPBMA coating was examined using a JSM-6360 LV scanning electro microscope (JEOL Co., Japan).
To certify the change of the hydrophilicity of 316L stainless steel, the surfaces of 316L stainless steel uncoated and PPBMA-coated films were characterized by static water contact angle measurements using the JC2000 A system (Shanghai Zhongchen Digital Equipment Co. Ltd, China) equipped with a Panasonic GL350 camera. The changes of the water contact angle with the different exposure time in air were also investigated. For this purpose, water droplets of approximately 10 μL each were mounted over three different places on the surface of the substrate. The θ value was taken as an average of the number of measures taken.
2.3 In vitro cell culture
The human umbilical cord veins endothelial cells (HUVEC) were obtained from China Centre for Type Culture Collection and incubated in a culture medium consisting of 20% (v/v) fetal calf serum (FCS, Sijiqing Biotech. Co., China) and 80% RPMI1640 (Gibco BRL Co.) supplemented with 100 U/mL penicillin and 100 μg/mL streptomycin in humidified air containing 5% CO2 at 37 °C. For sterilization, the substrate 316L stainless steel (with and without PPBMA coating) was first rinsed gently with 70% ethanol following with air-blown drying, and then exposed to UV irradiation for 30 min under a 20 W mercury-vapor UV lamp (ZWS-UV 20 W, 50 Hz, Huanghai Lighting Co. China) integrated in the laminar air flow hood with a distance of 75 cm between samples and lamp. Repeated the above procedure once again.
After sterilization, the substrates were kept in 96-well plates and the HUVECs were seeded at an initial cell density of 1.35 × 104 cells per well. The cells were incubated for 4h and 12 h, respectively. After incubation, the samples were washed twice with PBS to remove the nonattached cells. The remaining cells were removed by digestion with 0.25% trypsin solution. The number of cells attached on the different surface was determined by hemocytometer counting [15]. The cell attachment was expressed as a percentage of the number of cells attached on the 316L stainless steel surface without PPBMA coating.
For cell growth studies, the sample preparation was the same as for the above-mentioned attachment assay. Cells were seeded at a density of 1.35 × 104 cells per well. The culture media was replenished every second day. The randomly selected wells were washed twice with PBS and digested with 0.25% trypsin solution per day for up to 4 days. The number of cells grown on the samples surfaces was determined by hemocytometer counting.
The morphologies of the cells on the different substrate after seeding 96 h was observed by SEM. 316L stainless steel coated and uncoated were washed with 0.1 M cacodylate buffer (pH 7.4) to remove the unattached cells. The HUVECs were fixed with 2.5% glutaraldehyde solution for 1 h at 4 °C. Then the samples were sequentially dehydrated in 75% and 95% aqueous ethanol solution, each for 15 min. The samples were further dehydrated for two times, first in acetone and then in isoamylacetate, each for 15 min. The samples were put in a pressure chamber with liquid CO2, and the CO2 was vaporized at a temperature above its critical point. The dried samples were coated with Au by a sputter coater and examined by scanning electron microscopy (SEM) (JEOL Co., Japan).
2.4 Platelet adhesion
For platelet adhesion studies, fresh human blood anticoagulated with acid citrate dextrose was centrifuged at 1,000 rpm for 10 min to obtain platelet-rich plasma (PRP). The coated and uncoated 316L stainless steel substrates were submerged with PRP for 1 h at 37 °C in an incubator. After washing gently with PBS to remove nonadhering platelets, fixing was done with 2.5% buffered glutaraldehyde solution for 1 h at 37 °C. Specimens were then dehydrated with 50, 70, 95 and 100 dilutions of ethanol and water and dried. All the specimens were coated with a gold layer and observed with SEM (JSM-6360 LV JEOL, Japan).
2.5 The adhesion strength of the PPBMA coating on stent
The PPBMA-coated 316L stainless steel stent (DeviceTeck Inc., USA) was loaded on the balloon site of a Multi-Link catheter (3.0 mm inflated diameter; DeviceTeck Inc., USA) and the balloon was inflated to expand the stent (inflation pressure 8 atm). After inflation, the stent was coated with Au by a sputter coater and examined by scanning electron microscopy (SEM) (JEOL Co., Japan).
2.6 Statistics analysis
All data were collected in eight independent experiments. Data were analyzed using the Student’s t-test. The difference between treatments was considered significant when p < 0.01 in a two-tail analysis.
3 Results
3.1 Chemistry of the plasma PPBMA coating
The successful deposition of PPBMA onto the substrate samples was directly evident from the chemical composition determined by FTIR and XPS analyses. Figure 2 shows the FTIR spectra of the BMA monomer and its plasma polymer. It can be seen that there were some differences, both in terms of intensity and in terms of location of the absorption band between the BMA monomer and its corresponding plasma polymer. As shown in Fig. 2, compared with the spectra of monomer, the C=O stretching band at 1720 cm−1 almost disappeared, and the C–O–C stretching bands at 1295, 1268, and 1168 cm−1 decreased significantly in the resultant PPBMA films. Whereas the C–H stretching bands of CH3 and CH2 groups were found at 2,963 and 2,875 cm−1, the band at 1,652 cm−1 due to the C–C stretching vibration still existed [16], indicative of significant unsaturation in the PPBMA films. This is unconventional in PBMA chemistry. Broad and strong absorption bands between 3,500 and 3,100 cm−1 were also observed, which may be attributed to the stretching vibrations of hydrogen-bonded hydroxides [17].
XPS survey scans (data not shown) of the constitute elements revealed carbon and oxygen as main elements, indicating that a uniform PPBMA coating completely covered the substrate and the thickness of the plasma coating exceeded the sampling depth of XPS (roughly 30–80 Å). Figure 3 shows the high resolution C1s scan of the PPBMA coating. Deconvolution of the spectra was carried out using a Gaussian curve fitting technique, and the contributions are assumed to be due to carbon bonding according to other reports [18]. The binding energies and relative fraction of the different moieties are listed in Table 1. As can be seen from Fig. 3, besides the characteristic carbon moieties of the conventional poly (BMA) sample (C–H (285.1 and 285.7 eV), C–O–C (287.3 eV) and O–C=O (288.5 eV)) [19], a new peak at 286.4 eV assigned to the C–OH bonding appeared on the C1s scan of the prepared PPBMA film. The measured areas of the C–H, C–O–C and O–C=O peaks from standard poly (BMA) were in relative fraction of 74.5%, 12.5%, and 12.5% [19]. But in this study, the relative fraction of C–H, C–O–C, O–C=O and C–OH was 73.2%, 7.1%, 5.6%, and 14.0, respectively. These results suggested that the plasma PPBMA film displayed similar CH x spectra, loss of C–O–C and O–C=O, and new C–OH moiety in comparison with the conventional poly (BMA). These results are in agreement with the FTIR.
3.2 Morphology and hydrophilicity of the PPBMA coating
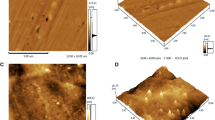
The plane view SEM image of the deposited PPBMA film was illustrated in Fig. 4. For comparison, the morphology of the plasma PPBMA film deposited in the absence of oxygen is also shown. It can be seen that the surface morphology of the polymer films was strongly affected by the oxygen carrier gas. A “dome-like” structure of nanometer size was observed on the surface of the PPBMA film deposited without oxygen, but not on that of the PPBMA film deposited with oxygen. The size of the domes was about 50 nm. The film deposited in the presence of oxygen had a uniform, smooth surface.
The hydrophilicity of the 316L stainless steel after the PPBMA deposition may be indicated by use of contact angle measurements. The results of hydrophilic modification are presented in Table 2. As shown in this table, the original water contact angle of the 316L stainless steel was 24°. After PPBMA deposition, the water drop spread immediately and the contact angle decreased to about 2.0°, indicative of a more hydrophilic surface after deposition of PPBMA. Meanwhile, these results also confirmed the occurrence of plasma polymerization on the 316L stainless steel. The changes of the hydrophilicity of the PPBMA coating with respect to the increase in exposed time showed that the PPBMAs maintained their hydrophilicity with a slight change for 4 days.
3.3 Endothelial cells attachment and proliferation
To compare the differences of the surfaces to endothelial cells, quantitative analyses were performed with respect to cell adhesion and proliferation on the 316L stainless steel with and without PPBMA coating. The data were analyzed using the Student’s t-test to determine whether there were any statistically significant differences among the experimental groups.
Attachment characteristics of HUVECs to the 316L stainless steel with and without PPBMA deposition were studied and the results are shown in Fig. 5. The values for attachment cells were reported as a proportion of the number of cells that attached to 316L stainless steel with the same incubation time. As shown in Fig. 5, the cell attachment was significantly better on the PPBMA coating (p < 0.01), and the adherent cells on the PPBMA-coated surfaces were around 72% and 90% higher after 4h and 12 h incubation when compared to that of the control. It suggested that cell attachment was strongly stimulated by the presence of plasma PPBMA deposition.
Attachment of endothelial cells on 316L stainless steel without and with PPBMA coating. The cell attachment was expressed as a percentage of the number of cells attached on the 316L stainless steel surface control. Results are the mean ± SEM from at least eight separate experiments (p < 0.01). The cells attachment was strongly stimulated by the presence of plasma PPBMA deposition
Figure 6 shows the growth curves of HUVECs on 316L stainless steel uncoated and coated over a period of 4 days. It was found that cells grew faster on the modified coating than that on the unaltered substrate. In particular after 2 days, a 1.5–2 fold increase of the cell numbers was observed on the PPBMA-coated surface, as compared with the control experiment with noncoated 316L stainless steel surface. These results imply that the cell viability on the hydrophilic surface of the PPBMA-coated 316L stainless steel was superior to the surface of the uncoated control.
The morphologies of HUVECs after 96 h of incubation on 316L stainless steel control and plasma modified coating observed by SEM were shown in Fig. 7. The focal points of the endothelial cells can be seen clearly. It can be seen that the cultured cells had attached to the surface of the 316L stainless steel before and after modification within 96 h cultivation. HUVECs could not spread well following a wound-shaped morphology on the 316L stainless steel control surface. However, on the plasma PPBMA-coated 316L stainless steel, the HUVECs showed the typical cobblestone-like appearance and reached confluence. The HUVECs spread out in only one plane on the surface and there was little or no overlapping of cells due to contact inhibition. Further, HUVECs were larger and more elongated than those cultured on the 316L stainless steel control.
Morphologies of HUVECs seeded on (a) control and (b) PPBMA-coated 316L stainless steel. Cell seeding density 1.35 × 104 cells per well. Cells cultured for 96 h. HUVECs on 316L stainless steel control surface exhibited a wound-shaped morphology. On the plasma PPBMA-coated 316L stainless steel, the HUVECs showed the typical cobblestone-like appearance and reached confluence
3.4 Platelet adhesion
The platelet adhesion on 316L stainless steel before and after plasma deposition was investigated and the results are illustrated in Fig. 8. It can be seen that the unmodified 316L stainless steel surface had more platelet adhesion and some platelets were aggregated, while the platelets on PPBMA coating surface were decreased and less platelets were aggregated. By plasma deposition PPBMA onto stainless steel surface, the blood compatibility was apparently improved.
3.5 Adhesion strength of the PPBMA coating on stents
In order to investigate the adhesive strength of PPBMA on the stent, the PPBMA-coated stent was expanded in vitro according to the clinic protocol. The PPBMA-coated stent was observed under SEM before and after stent expansion, and the results were presented in Fig. 9. From the figure, it can be seen that after balloon expansion, the entire coating layer remained intact on the stent struts except at the micropore, which suggested that the adhesion strength of the PPBMA coating was sufficient to maintain the shear stress during the stent expansion process. This ability is critical for effective surface modification of an intravascular stent device.
4 Discussion
An angioplastic procedure with a metallic stent is a standard of percutaneous therapy of coronary artery disease. Stenting, however, causes significant injury to the vascular wall and endothelium, resulting in inflammation, repair and the development of neointimal hyperplasia. To solve these problems associated with intravascular stenting, enhancement of rapid re-endothelialization, re-endothelium-paving or relining at denudated regions has been proposed and attempted using a number of techniques [1–2, 20–22]. In particular, coating of stent surface with an endothelial cells-compatible layer can stimulate the attachment and proliferation of the surrounding mature endothelial cells and the circulating endothelial progenitor cells to/on stents’ surface, accelerating the formation of an active endothelial cells layer after prosthesis implantation. This is an attractive strategy for the simultaneous prevention of thrombus formation and neointimal hyperplasia [8].
Therefore, to construct a more endothelial cells-compatible coating on the 316L stainless steel, a PPBMA coating, which has been used as a barrier coating to control the drug release [19], was successfully deposited on the vascular prosthesis through plasma polymerization in the presence of oxygen in this experiment. The plasma PPBMA which contains a great deal of hydrogen-bonded OH group was preferably selected [23]. The chemical composition, the morphology and wettability, the in vitro behavior of human vascular endothelial cells (HUVEC) as well as platelet adhesion of the 316L stainless steel without and with PPBMA coating were investigated in detail. In addition, the adhesion strength of the PPBMA coating on the stent was also studied.
The principle of the polymerization in the plasma discharge condition is totally different from that of the traditional chemical method. Under plasma discharge, the monomer would be induced and reactive species could be produced under the interaction between ions. Thus, the reactive species produced would react with each other to form polymer deposits on the substrates. A carrier gas, such as Ar, O2, or H2, can effectively excite monomer and introduce more radicals or functional groups into the deposition, affecting the properties of some plasma polymers [24, 25]. In this study, oxygen was used as the carrier gas.
We can see from the FTIR spectra of BMA monomer and PPBMA coating (Fig. 2) that the fragments made significant contributions to the film deposition, instead of the BMA monomer itself. This result is in agreement with the pioneering work of Oehr and co-workers, who reported that the starting monomer in the plasma polymerization process is highly degraded and the resulting fragments are scrambled, causing the deposited film to be significantly different from that obtained from conventional polymer [26]. On the other hand, it can be deduced from the spectra of FTIR and XPS that the C–H and C=C structure still remains in the plasma-polymerized film, but the C=O and C–O–C bonds were obviously decreased. The observed results are somewhat unexpected. The presence of oxygen in the plasma would seem to indicate the creation of more oxygen-bearing groups, such as carboxyl and carbonyl moieties. However, the data deny that hypothesis, presumably derived from the plasma deposition mechanism. Rabek found that there were two mechanisms for the loss of ester functionality in the plasma polymerization [27]. One is via the scission of the C–OR bond, creating a radical site on the carbonyl carbon available for crosslinking or initiation reactions. The other is removal of the entire ester group via scission of the C–COOR bond, which decreases the concentration of both oxygen and carbon moieties. Observance of decreasing O–C moieties in the PPBMA indicated that some degree of functional loss is due to the scission of the C–COOR bond. More experimentation is necessary to systematically determine the mechanism of BMA plasma polymerization and the effect of oxygen carrier gas.
Additionally, from the FTIR and XPS, the existence of the –OH groups in the PPBMA film can be determined. In general, there are some free radicals left on the plasma polymer surface available to capture oxygen and water from air, thereby resulting in the formation of –OH groups.
Figure 4 revealed a pronounced effect of oxygen carrier gas on the surface roughness of the plasma PPBMA films. We believe that this is an effect of the plasma deposition process. Generally speaking, during the plasma polymerization process, reaction in the gas phase can lead to the production of powders; reaction at the surface can result in very flat films [18]. It is believed that oxygen has two basic effects in the plasma deposition. One is, of course, the dilution effect. As the total flow rate was constant, the addition of oxygen diluted the reactive species that formed in the plasma. The other one, which is more important, is a chemical effect on the composition of plasma. Oxygen atoms are excited from ground states to excited states by absorbing energy. This energy of the atom can dissociate the intermediate molecules via collision. Addition of oxygen to the reaction could decrease the rate of film deposition by reducing the number of polymer forming radicals in the gas phase [28]. Consequently, polymerization in the presence of oxygen occurred mainly on the surface and not in the plasma volume, resulting in a smooth and dense film.
Water plays an important role in determining the biocompatibility characteristic of the biomaterial. It is well known that high water levels on the surface of the biomaterial providing a low interfacial tension with blood, which would reduce fibrinogen adsorption and enhance cell adhesion on the surface. Contact angle measurement indicated that the PPBMA coating by radio-frequency plasma polymerization appreciably improved the surface hydrophilicity of the substrate (Table 2). In general, the surface wettability is greatly dependent on the hydrophilic groups, such as –OH, C=O, etc. In addition, the aging property of the hydrophilicity is also important for maintaining the biomedical apparatus in a clinical application. Yang and co-workers have reported that there were some defects when plasma treatment was utilized as the sole method to modify the materials, because the hydrophilicity of material surfaces would decrease with an increase in the preserving time, in particular in the initial time, owing to the surface mobility [29]. Somewhat contradictory to our results is that the high wettability of PPBMA coating deposited on the 316L stainless steel was very stable, with a slight decrease even after 4 days. A potential explanation for this phenomenon might involve the inherent property of plasma-polymerized film, which is highly branched and cross-linked with strong mechanical and chemical stability [30].
It is likely that a favorable response to a biomaterials substrate is controlled by the nature of the substrate surface in vitro and in vivo. This is especially true for endothelial cells, which are known to be functional cellular components of vascular tissues. Studies on different model surfaces with defined physicochemical properties point toward a dependence of endothelial cells responses (such as cellular adhesion, spreading and proliferation) on the surface characteristics like hydrophilicity, charge, and chemistry [31, 32]. The reason why the PPBMA deposited in the current experiment promotes endothelial cells adhesion and growth was considered. First, the PPBMA coating deposited by plasma polymerization in the presence of oxygen contained high oxygen-bearing functionality, especially the –OH, which improved surface hydrophilicity, and subsequently enhanced the cell spreading and proliferation. Second, appropriate surface concentration of hydrophilic groups was formed on the PPBMA polymer, which is conducive to improving the ECs-material compatibility. The lower hydrophilic group does not stimulate cell attachment and growth, and the higher hydrophilic grafting degree leads to the resistance of cell anchorage [31]. So, from this viewpoint, the PPBMA coating deposited in this experiment possesses an appropriate concentration of hydrophilic groups. Third, the positive charges on the surface can be greatly improved by RF discharge [33], which would advantageously adsorb the cells that carried negative charge [33, 34]. It is also worthwhile to note that after PPBMA deposition, the adhesion force between the endothelial cells and the substrate was also enhanced. The adhesion force of the cells is closely related to the cell morphology. With a strong adhesion force exerting on the extra-cellular matrix, the cells assume a flat morphology and the adhesion cells are extensive. These results may be helpful for the promotion of re-endothelialization by endothelial cells to repair the injured vascular surface, inhibit the formation of thrombus, and inhibit the stimulation of SMCs.
As a blood-contacting biomedical device, the stent surface should not only promote formation of a confluent endothelial cell layer, but also prevent thrombus, especially in the initial stage after prosthesis implantation. The sudden occlusion due to on-stent thrombus formation always occurs in the early period [1]. The adhesion and aggregation of platelets are important steps in the process of thrombus formation, whereby the potential of platelets adhesion on the uncoated and PPBMA-coated 316L stainless steel was investigated. Bare 316L stainless steel is thrombogenic and is easy to initiate platelet adhesion and activation. The platelet adhesion, however, after PPBMA deposition, was greatly reduced, indicative of the improvement of blood compatibility. This good blood compatibility of the PPBMA films can be attributed to the high hydrophilicity, surface free energy arising from the –OH, C=O, and C–O functionalities and the smooth surface deposited in the presence of oxygen.
During the stent deployment process, the coating and stent is inevitably expanded and sheared by the flow of body fluid. Then, one important question is whether the PPBMA coating on vascular prosthesis could endure the shear stress during the stent deployment. The weakly adhered coating, if detached from the intravascular stent, would enter into the blood and induce many diseases. From Fig. 9 ex vivo expansion experiment of the plasma PPBMA-coated stent, it is clear that the adhesion strength between the PPBMA coating and stent was sufficient to endure the shear stress in the stent expansion. The ultra-thin-film deposition and good adhesion to substrate are inherent advantages of the plasma polymer, which may contribute to the good adherence of the PPBMA coating.
We can show that the metallic stent surface, which normally does not allow good growth of endothelial cells, does so after PPBMA deposition. Also, the PPBMA coating does not decrease the blood-compatibility of the prosthesis. Rather, a significant decrease in platelets aggregation is observed. Moreover, the PPBMA coating can also withstand the shear stress in the stent expansion. Ongoing research about in vivo re-endothelialization potential of this PPBMA-coated stents is underway in our group. These preliminary results are convincing, which might open new possibilities for the use of PPBMA in cardiovascular stent surface modification, since plasma PPBMA deposition prior to implantation is an easy, cost-effective and substrate-dependent way to improve cardiovascular implants. Additionally, our data imply that the field of vascular tissue engineering might benefit, by improving the interaction between endothelial cells and biomaterials.
5 Conclusion
To realize the rapid re-endothelialization of intravascular stent devices after implantation, a poly n-butyl methacrylate coating was deposited through a radio-frequency plasma polymerization process in the present study. Oxygen was applied as a carrier gas to modulate the coating properties. The deposited PPBMA coating maintained a high hydrophilicity even after 4 days of exposure, as well as smooth and dense coverage. Compared with that on the uncoated 316L stainless steel, the attachment and proliferation of the endothelial cells on the PPBMA-coated were significantly increased and the platelet adhesion was also reduced, implying that the deposited PPBMA coating could simultaneously promote formation of a confluent endothelial cell layer and prevent thrombus formation. In addition, after expansion, the PPBMA coating still remained on the stent. Thereby, it is concluded that surface modification by this method appeared to be a promising strategy for in situ rapid re-endothelialization of vascular devices.
References
T. SHIROTA, H. YASUI and H. SHIMOKAW, Biomaterials 24 (2003) 2295
A. SUWAIDI, P. B. BERGER and J. DR HOLMES, J. Am. Med. Assoc. 284 (2000) 1828
K. MICHAEL, J. C. ROBERT and M. R. STEPHEN, US2003/0229393A1, Dec 11, 2003
A. S. EUGENE and A. T. SAN, US 6,140,127, Oct 31, 2000
J. AOKI and P. W. SERRUYS, J. Am. College. Cardio. 45 (2005) 1574
A. M. SEIFALIAN, A. TIWARI, G. HAMILTON and H. J. SALACINSKI, Art. Organs. 26 (2002) 307
K. J. PAWLOWSKI, S. E. RIRRGERS, S. P. SCHMIDT and G. L. BOWLIN, Front. Biosci. 9 (2004) 1412
L. W. K. MENNO, B. J. A. YVETTE and H. K. LEO, Biomaterials 27 (2006) 2813
A. T. L. ONG, J. AOKI, M. KUTRYK and P. W. SRRUYS, Archives Des Maladies Du Coeur Et Des Vaisseaux 98 (2005) 123
Y. X. LIU, T. HE and C. Y. GAO, Colloids. Surf. B Biointerf.. 46 (2005) 117
M. MORRA, Eur. Cells. Mater. 12 (2006) 1
L. PRAMATAROVA, E. PECHEVA and V. KRASTEV, J. Mater. Sci. Mater. Med. 18 (2007) 435
G. H. RYU, W. S. YANG and H. W. ROH, Surf. Coat. Technol. 193 (2005) 60
V. PATRICK, G. THOMAS and D. UPULIE, J. Colloid. Interf. Sci. 259 (2003) 13
J. G. STEELE, G. JOHNSON, W. D. NORRIS and P. A. UNDERWOOD, Biomaterials 12 (1991) 531
H. PENG, S. Y. CHENG and Z. Q. FAN, J. Appl. Polym. Sci. 92 (2004) 532
I. GANCARZ, J. BRYJAK and M. BRYJAK, Eur. Polym. J. 39 (2003) 1615
M. KARDAR, Physica A. 281 (2000) 295
C. S. KWOK, T. A. HORBETT and B. D. RATNER, J. Control. Release 62 (1999) 301
M. S. CONTE, G. A. VANMETER, L. M. AKST, T. CLEMONS, M. KASHGARIAN and J. R. BENDER, Cardiovasc. Res. 53 (2002) 502
B. STEPHANE, A. MIREILLE and M. B. JACQUELINE, Biomaterials 26 (2005) 4567
M. C. YONG, S. NOZOMI and S. HIDEO, Biomaterials 26(2005) 4588
Y. YUAN, C. S. LIU and Y. ZHANG, Surf. Coat. Technol. 201 (2007) 6861
B. JOLANTA, I. GANCARZ, G. POZNIAK and W. TYLUS, Eur. Polym. J. 38 (2002) 717
I. GANCARZ, G. POZNIAK, M. BRYJAK and W. TYLUS, Eur. Polym. J. 39 (2003) 1615
C. OEHR, M. MULLER, B. ELKIN, D. HEGEMANN and U. VOHRER, Surf. Coat. Technol. 116–119 (1999) 25
J. F. RABEK, “Polymer Photodegradation: Mechanisms and Experimental Methods” (Chapman & Hall, London, 1995) 130
N. SHIRTCLIFFE, P. THIEMANN and M. STRATMANN, Surf. Coat. Technol. 142–144 (2001) 1121
J. YANG, J. BEI and S. WANG, Biomaterials 23 (2002) 2607
Z. Y. WU, Y. H. YONG, G. L. SHEN and R. Q. YU, Anal. Chim. Acta. 412 (2000) 29–35
Y. B. ZHU, C. Y. GAO, J. J. GUAN and J. C. SHEN, Biomed. Mater. Res. 67A (2003) 1367
P. B. VAN WACHEM and T. BEUGELING, Biomaterials 6 (1985) 403
X. F. FENG, J. ZHANG and H. K. XIEL, Surf. Coat. Technol. 171 (2003) 96
J. J. GUAN, C. Y. GAO, L. X. FENG and J. C. SHENG, J. Biomater. Sci. Polymer. Edn. 11 (2000) 523
Acknowledgments
The authors appreciate financial support from the National Science Fund for Distinguished Young Scholars of China (Grant No. 20425621), the Major State Basic Research Program of China (No. 2005CCA01000), the Basic Research Foundation of the Shanghai Science and Technology Committee (05DJ14005) and the Shanghai Foundation for Cultivation of Excellent Young Teachers. The authors also gave thanks to Paula Stevenson of the Ohio State University for English improvement of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yuan, Y., Liu, C. & Yin, M. Plasma polymerized n-butyl methacrylate coating with potential for re-endothelialization of intravascular stent devices. J Mater Sci: Mater Med 19, 2187–2196 (2008). https://doi.org/10.1007/s10856-007-3319-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-007-3319-8