Abstract
Background
At peak COVID-19 lockdown, patients with symptomatic atrial fibrillation (AF) were faced with an equipoise between a palliative rate-control versus cautious rhythm-control strategy, including hospitalization for initiation of antiarrhythmic drug/s (AADs) and cardiac procedures which was impossible due to hospitalization restrictions.
Objectives
We aimed to evaluate the efficacy and safety of outpatient initiation of dofetilide in patients with AF using cardiac implantable electronic devices (CIEDs) for rhythm and QTc interval monitoring.
Methods
Adult patients with symptomatic AF with prior failure or intolerance to other AADs were enrolled if they were willing to in-office insertion of implantable loop recorders or already implanted with pacemakers or defibrillators capable of remote monitoring. Exclusion criteria were known medical contraindications of dofetilide and unable to provide consent. After making a shared management decision, dofetilide was initiated in a physician office, and rhythm and QTc intervals were monitored by ECGs and CIEDs. Patients were followed to assess the efficacy and safety of the treatment.
Results
The study cohort comprised of 30 patients, age 76 ± 7 years (mean ± standard deviation), 10 female (33%), CHA2DS2-VASc score 3.25 ± 1.3, ejection fraction 63.45% ± 8.52, and QTc interval 431.68 ± 45.09 ms. From 22 (73%) patients in AF at presentation, SR was restored in 14 (64%) patients after 4 doses of dofetilide. At 46 ± 59 days of follow-up, maintenance of SR in total 22 (73%) patients without cardiac adverse effects was accomplished.
Conclusion
Effective and safe outpatient initiation of dofetilide during the extenuating circumstance of COVID-19 lockdown was possible in patients with AF who had CIEDs.
Similar content being viewed by others
1 Introduction
The SARS-CoV-2 corona virus (COVID-19) pandemic has a profound impact on health care globally. At the peak of COVID-19, most hospitals closed or limited their inpatient admissions for patients with non-COVID illnesses, routine surgeries, and procedures. Given the real fear of the increased risk of viral transmission, caring for their patients with established non-COVID-19 illnesses and co-morbidities remains significantly difficult for physicians. Various new and innovative methods, including telemedicine, have become acceptable methods for providing counselling, follow-up, and treatment to patients. In such a situation, many patients with disabling and repetitive symptoms from paroxysmal and persistent atrial fibrillation (AF) and atrial flutter (AFL) despite multiple antiarrhythmic drugs (AADs), prior cardioversions to restore sinus rhythm (SR), some with cardiovascular implantable electronic devices (CIEDs), i.e., permanent pacemakers (PPMs), implantable cardioverter-defibrillators (ICDs), and implantable loop recorders (ILR), and some awaiting AF ablation but unable to do so due to the COVID-19 lockdown had to maintain an equipoise between a cautious and innovative intervention for the restoration and maintenance of SR versus a palliative rate-control strategy.
Dofetilide, a Vaughn-Williams class III AAD, with its selective blocking of the rapid component of the delayed rectifier outward potassium current (IKr), lack of toxicities such as bradycardia or betablockade effects, pulmonary and hepatic damage, becomes a viable treatment option in select patients with AF. The Danish Investigations of Arrhythmia and Mortality ON Dofetilide-Myocardial Infarction and Congestive Heart Failure (DIAMOND-MI and DIAMOND-CHF), the Symptomatic Atrial Fibrillation Investigative Research on Dofetilide (SAFIRE-D), and the European and Australian multicenter evaluative research on atrial fibrillation dofetilide (EMERALD) trials demonstrated the effectiveness of dofetilide in restoring and maintaining SR long term by chemical cardioversion of AF and AFL, and no adverse effect on mortality rates even in severely ill patients with left ventricular dysfunction and advanced heart failure [1,2,3,4]. The association between being in SR and lower mortality was also established in these trials [5]. However, a small but significant risk of QTc prolongation and development of torsades de pointes (TdP) polymorphic ventricular tachycardia was also observed with dofetilide leading to the recommendations that dofetilide be initiated in a hospital setting with continuous telemetry rhythm monitoring [6].
The purpose of this study was to evaluate whether dofetilide could be initiated effectively and safely as an outpatient in a select group of patients in whom continuous telemetry monitoring may be performed by CIEDs during the extenuating circumstances created by the COVID-19 pandemic.
2 Methods
2.1 Study design
In this prospective clinical longitudinal study, conducted in a real-world practice setting, patients who had not responded to or had significant side effects from conventional AAD therapy and who could not be referred for ablation or cardioversion due to denial for hospital admissions, and reluctance to get hospitalized from COVID-19 pandemic lockdown situation that began in mid-February 2020 were considered for enrollment. Only patients who met the following inclusion criteria were enrolled: (i) age > 18 years, (ii) symptomatic paroxysmal or persistent AF that did not respond to or experienced significant side effects with other conventional AADs, and (iii) already implanted with CIEDs, i.e., PPMs for sinus node dysfunction, or ICDs for primary prevention of sudden cardiac death, and ILRs for AF management, or willingness for insertion of ILRs in physician’s office. Exclusion criteria for dofetilide initiation were (i) significant renal insufficiency (creatinine clearance < 20 mL/min), (ii) significant prolonged QTc (> 460 ms) at baseline, (iii) bradycardia, heart rate < 60 bpm, (iv) high grade to complete heart block causing ventricular pacing dependency, (v) a history of long QT syndromes, (vi) uncorrectable electrolyte and metabolic disturbances, (vii) contraindication to anticoagulation, (viii) any other known medical contraindications of dofetilide, and (ix) unable to provide informed consent.
After making a shared decision treatment plan following discussion and full disclosure about the benefits and risks of the drug, dofetilide was started in a modified controlled setting in patients with an adequate anticoagulation status. All PPMs and ICDs were programmed to provide a lower rate pacing at 70 beats per minute. Given different types of CIEDs and their manufacturers, ventricular high rate detection programming were individualized but as close as possible to detect > 160–170 beats per minute. Baseline characteristics, laboratory data, and medical history including dose strengths and total number and adjustment of doses, discontinuation, and occurrence of arrhythmias and adverse effects were recorded.
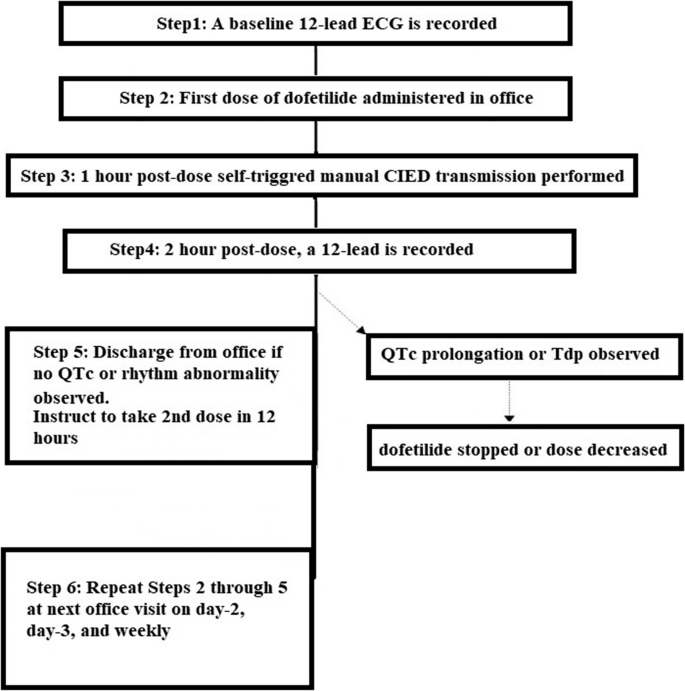
2.2 Dofetilide protocol
Treatment with dofetilide was initiated in a physician’s office facility equipped to provide advanced cardiac life support if necessary. All patients had their renal and hepatic function assessed prior to initiating treatment. Furthermore, all patients were appropriately anticoagulated prior to initiating treatment. Patients were started on the optimal dose calculated based on creatinine clearance (CrCl) using the Cockcroft formula. Dosages of dofetilide were 500 microgram (mcg) twice a day (bid), 250 microgram bid, and 125 microgram bid for patients with CrCl > 60 mL/min, 40 to 60 mL/min, and 20 to 40 mL/min respectively. Patients with significant renal insufficiency (CrCl < 20 mL/min) were not included in the study. Dofetilide was discontinued if after the second dose of dofetilide QTc prolonged to > 500 ms. Subsequently, the dose was adjusted based on the results of cardiac monitoring, if necessary [7].
On the day of the drug initiation, patients were asked to bring their CIED monitors with them to their office visit. They were instructed that their visit would last a minimum of 3 h, during which time they would take their first dose of dofetilide around 8.00 a.m. A 12-lead ECG was obtained to establish a baseline. Besides being monitored with a continuous cardiac telemetry via CIEDs for a minimum of 2 h, a mandatory manual transmission was obtained from the patient’s CIED at 1 h. Two hours after taking their initial dose, a 12-lead ECG was obtained. If no QTc changes were observed on CIED transmission or ECG, the patient was sent home and instructed to take a 2nd dose 12 h later and transmit a mandatory reading from their CIED monitor 1 h after taking dofetilide and development of any concerning symptoms such as dizziness. The procedure was repeated on their day 2 and day 3 office visit including CIED transmission. Provided no QTc changes or adverse cardiac events were observed, the patients were sent home with instructions to return in 1 week, 2 weeks, and 3 weeks. Patients were instructed to perform CIED transmission at least once during the week and whenever deemed necessary. For each return visit, the above protocol was followed. CIED transmission-based monitoring would thus provide more than 3 days of recommended rhythm monitoring for in-patient initiation of dofetilide in patients without CIEDs.
Very close clinical follow-up was maintained by means of frequent telephone and audio and video telemedicine consultations. Patients were asked not to travel and stay prepared to seek emergency medical help, including 911 calls, visit their local health care facility, and calling physicians in the event of serious symptoms such as episodes of dizziness and loss of consciousness. Patients were given oral K and Mg supplements as needed. Dofetilide dose was reduced and adjusted depending on the response, and if on steady dosage QTc prolongation > 15% from baseline or QTc > 500 ms occurred. Dofetilide was discontinued if after the second dose of dofetilide QTc prolonged to > 500 ms, or if the patients experienced dizziness, syncope, torsade de pointes (TdP), or any adverse side effects listed in the package insert [7]. Figure 1 summarizes our dofetilide administration protocol.
2.3 Ethics
The ethical standard of the study was observed as per the 1975 Declaration of Helsinki. Informed consent was obtained from each patient for implantation of FDA-approved CIEDs when necessary.
2.4 Statistical analysis
Statistical analyses were performed on the data sets collected during follow-up. Categorical data are expressed as count (percentage) and continuous variables as mean ± standard deviation (SD) and/or median with interquartile range (IQR) where appropriate. A t test was used for the comparison of variables where appropriate, and a p value of <0.05 was considered statistically significant.
3 Results
3.1 Patient characteristics
The study cohort comprised 30 patients, mean age 76.3 ± 6.7 years (± SD), median 78 years (IQR = 72–81 years), and 10 (33%) female patients. The CHA2DS2-VASc score and left ventricular ejection fraction (LVEF) were 3.25 ± 1.3 and 63.45 ± 8.52% respectively. All patients had a history of paroxysmal or persistent AF. The clinical characteristics are provided in Table 1. There were 26 (87%) patients with hypertension, 7 (23%) with diabetes mellitus, 11 (37%) with vascular disease, and 1 patient with heart failure with reduced ejection fraction (HFrEF) whose LVEF ranged between 30 and 35%. There were 10 patients who had PPMs (all for sick sinus syndrome [SSS]/sinus node dysfunction), 2 with ICDs (both for primary prevention of sudden cardiac death; in 1 patient LVEF improved to > 35% post-ICD), and 18 with ILRs (all previously implanted for AF management) (Table 2).
There were 19 patients taking concurrent medications that may potentially prolong QTc interval (Table 3). Among patients taking diuretics, one patient was taking hydrochlorothiazide (HCTZ). Although considered to be a contraindication, since he was taking a lower dose of 12.5 mg in a combination formulation with losartan for control of hypertension for a very long time, the risk of adverse effect per se for HCTZ was deemed low, and hence was not discontinued.
The presenting rhythm at the time of dofetilide initiation was AF in 22 (73%) patients and SR in 8 patients (27%). All patients had a history of paroxysmal or persistent AF. The average duration of AF prior to starting treatment was 524 days (± 469 days).
3.2 Efficacy and adverse effects of dofetilide
The presenting index rhythm at the time of dofetilide initiation was AF, mean rate 79.46 ± 18.47 bpm, in 22 (73%) patients and SR, 68 ± 12.71 bpm, in 8 patients (27%). All patients had a history of paroxysmal or persistent AF. The average duration of AF prior to starting treatment was 524 days (± 469 days).
The baseline QTc was 431.68 ± 45.09 which prolonged at a steady state to 456.6 ± 43.03 after 14 doses. As such, patients with high grade to complete heart block causing ventricular pacing dependency at baseline were excluded from the study, but additionally, none of the patients developed conduction block needing ventricular pacing. QTc measurements were hence made in normally conducted ventricular complexes. QTc interval changes are presented graphically in Fig. 2. Heart rate changes are presented graphically in Fig. 3. QTc prolongation (> 15% from baseline or > 500 ms) which required dose adjustment occurred in 17% (5/30) of patients. Dofetilide resulted in the successful restoration of normal SR, 83.75 ± 17.35 bpm after a mean number of 4 doses in 64% (14/22) of patients who presented in AF. In these and an additional 8 patients who were in SR at presentation, SR at 72.64 ± 15.27 bpm was maintained in 73% (22/30) during the 46 ± 59 days of the follow-up period. Effective maintenance dosage of dofetilde was 500 mcg bid in 14 patients, 250 mcg bid in 15 patients, and 125 mcg in 1 patient after initiating the drug.
Two patients discontinued dofetilide due to intractable nausea. One patient died from gastrointestinal bleeding. The patient who died was 79 years of age and had a St Jude Medical/Abbott dual-chamber PPM implanted 8 years ago for SSS. He had obesity, diabetes mellitus, hyperlipidemia, diastolic heart failure, and CHA2DS2-VASc score of 4. Following his death, as we routinely retrieve CIEDs for possible re-use in poor patients in the developing countries through our charity work [8], the device was removed by the funeral director and interrogated. The device interrogation did not show QT prolongation, or episodes of AF or ventricular tachycardia prior to his death confirming that there was no association between the cause of his death and dofetilide.
3.3 CIED performance
No CIED malfunction or premature battery depletion due to continuous monitoring and mandatory manual transmissions was seen during the study duration.
4 Discussion
4.1 Major findings
Our study results demonstrate that dofetilide may be safely initiated in an outpatient setting provided the patient’s cardiac rhythm and QT intervals are being continuously monitored with a CIED and a close clinical follow-up is maintained with physical office visits and frequent telemedicine encounters.
There were several factors which contributed in our decision-making for initiating dofetilide treatment in an outpatient setting, despite conventional guidelines. First and foremost, we were dealing with clinical care of patients during the extenuating circumstances created by the COVID-19 pandemic. All patients were highly symptomatic with AF and had not responded to or had significant side effects from prior AAD therapy. These patients could not be referred for ablation or other procedures, given the COVID-19 lockdown; and the hospitals were closed down for EP procedures. There were no guidelines available, and even the Heart Rhythm Society, the American College of Cardiology, and the American Heart Association COVID-19 Task Force’s practice guidance document for electrophysiologists, although useful, did not become available till later in the pandemic [9]. After discussing with full disclosure about the benefits and risks of the drug, and taking a shared decision for treatment plans, our patients were prepared to accept the risk of potential adverse effects from dofetilide if they could achieve restoration and maintenance of SR without having to go to the emergency room of the local hospital, undergo external cardioversion under anesthesia, and face a very real risk of nosocomial COVID-19 transmission. These patients, being in a difficult situation of symptomatic AF, and the fear, anxiety, and apprehension of catching COVID-19 infection, chose a cautious and innovative intervention for the restoration and maintenance of SR versus a palliative rate-control strategy.
High efficacy of dofetilide in restoring and maintaining SR without significant adverse effect on mortality rates even in severely ill patients with left ventricular dysfunction and advanced heart failure has been shown in large clinical trials [1, 2]. For example, in the SAFIRE study which had included patients with AF and AFL, pharmacological cardioversions with dofetilide were achieved in 70% and 91% of patients in 24 h and 36 h respectively, with a high probability of remaining in SR at 1 year [3]. In contrast to the SAFIRE-D study which included patients with both AF and AFL, our study cohort comprised entirely of paroxysmal and persistent AF patients. And, yet we were able to accomplish the goal of successful restoration and maintenance of SR in 73% of patients with dofetilide. Compared to the observed results in larger clinical trials [3, 4, 10], we observed a higher success rate of SR restoration which we attribute to multiple factors including patient selection criteria, increasing baseline heart rate to 70 bpm by cardiac pacing, and continuous CIED remote monitoring systems to optimize pharmacotherapy. In our study, one patient died from gastrointestinal bleeding, but no fatality was observed due to dofetilide. The association between a lower mortality and being in SR was firmly established in a DIAMOND substudy which showed a risk ratio of 0.44 (95% CI, 0.30 to 0.64), with a very significant p value of 0.0001 for reduction of mortality when the rhythm was restored to SR from AF [5].
Dofetilide has been also reported to be safe and effective when rapidly switched from amiodarone and also when administered for “re-initiation” as an outpatient [11, 12]. The results of a well-conducted survey in the real-world clinical settings of 347 practicing cardiologists, the majority of whom were electrophysiologists, regarding their practice preferences concerning initiation and re-initiation of dofetilide were quite interesting; (i) 78% expressed that dofetilide re-initiation can be done on outpatient basis in the presence of normal serum K+, Mg+2, and baseline QT interval; (ii) 37% of the responders admitted patients in hospital only 10% of the time; (iii) 70% of the physicians reported no major adverse events; (iv) only 32% reported checking serum potassium, magnesium, and creatinine clearance; and (v) only 17% of the physicians checked QT interval at 48 h after the first dose of dofetilide during re-initiation [12].
The ability to discern QTc prolongation on CIED investigation is another favorable reason in terms of initiating dofetilide on an outpatient basis. One of the major limitations of prior major trials is that the technology for continuous remote telemonitoring was not available at that time [1, 4]. Hence, extrapolating data of these trials in the current population of patients with AF who may have various CIEDs may be subjected to further scrutiny. Remote monitoring of CIEDs has become a normal and essential component of the standard of care in patients with cardiac arrhythmias [13,14,15,16]. We have previously reported the utility of the technology in optimizing antiarrhythmic and anticoagulation therapy, including the safe withdrawal of long-term oral anticoagulation in some AF patients with a high risk of bleeding [17, 18]. It is also noteworthy that we were able to detect QTc prolongation using CIEDs at the similar and comparable rates that have been observed in the real-world studies where conventional methods of QTc monitoring were used [19, 20]. Interestingly, we did not observe any TdP or other ventricular arrhythmias in our study population. There were 18 patients in our study who already had ILRs implanted for AF management. Although no patient required ILR insertion during the study duration that involved COVID-19 pandemic lockdown, if required, we would have still chosen ILRs over external ambulatory ECG devices. The latter if disconnected intentionally or accidentally would result in the interruption of recording, and further if not connected correctly may produce significant artifacts disrupting and compromising the quality of recording. Also, there still remains uncertainty as to how long the COVID-19 pandemic would last, and in such situation, ILR by virtue of providing long-term monitoring compared to external ambulatory ECG devices remains the technology of choice for AF management. The ILR insertion procedure can be safely performed in physicians’ offices. Interestingly, the COVID-19 Task Force’s practice guidance document encourages the use of remote monitoring technology in the midst of the pandemic [9]. Along those lines, we were able to meet our study objective of evaluation of outpatient initiation of dofetilide in a select group of patients with CIEDs which provide continuous telemetry monitoring during the COVID-19 pandemic situation.
As regards following the stringent protocol of dofetilide initiation, a study conducted at a highly reputable cardiac arrhythmia specialist center led by cardiac electrophysiologists showed that almost half of their patients (49%, 93/189) had a deviation from the protocol, and some patients had recurrent deviation during their initiation process [21]. While ours was an unusual circumstance related to the COVID-19 pandemic, apparent deviation from conventional protocol was related to the FDA’s recent determination that the Risk Evaluation and Mitigation Strategy (REMS) certifications would be no longer required for dofetilide [22]. Previously, the manufacturer of dofetilide, trade name Tikosyn (Pfizer Inc; USA), had restricted its sale and use exclusively to the USA in spite of the fact that the major trials were performed outside of the USA, in the European countries, notably Denmark. Furthermore, dofetilide has now become available in a generic formulation [7], making it more cost-effective and accessible to pharmacies and physicians. Moreover, pharmacies no longer require physician approval prior to dispensation of the medication [22]. These recent developments have lowered the barrier of accessibility and increased physicians’ experience in using dofetilide safely and effectively.
As the world is currently gripped by the SARS-COV-2 corona virus (COVID-19) pandemic, most hospitals may follow stringent protocols including closure and restrictions regarding their inpatient admissions for patients with non-COVID illnesses. Our study demonstrated that in carefully selected patients who are symptomatic with paroxysmal and persistent AF, refractory to other AADs, and baseline sinus or paced rate is higher, dofetilide may be initiated safely in an outpatient setting using CIEDs for continuous monitoring. Careful patient selection is thus very important. The ability to initiate dofetilide therapy as an outpatient provides a safer alternative to patients with symptomatic AF who have failed other therapies, not to mention a very real risk of nosocomial COVID-19 transmission during hospitalization, and the monetary cost incurred to the patient [23]. A 3-day admission for drug initiation is an expensive proposition for any patient; replacing that protocol with 3 consecutive outpatient visits and periodic outpatient monitoring greatly reduces the cost to the patient [23, 24].
4.2 Study limitations
Our study is subjected to limitations as it has neither a randomized design nor a large cohort. Similar and perhaps larger series from other investigators would help to conclusively demonstrate the feasibility and safety of initiating dofetilide in an outpatient setting in a selected group of patients. Furthermore, our study essentially is a longitudinal clinical observational study conducted during the unique situation of the COVID-19 pandemic. Our study findings hence need to be taken in the context of the extenuating circumstances rather than in a more universal way. Our study, however, provokes and generates a hypothesis to test the strategy of outpatient initiation of dofetilide in patients with CIEDs in future studies of larger sample size and longer follow-up period, and perhaps even randomized with standard in-patient initiation to further validate our findings. If proven to be effective and safe, a stronger case could be potentially made to use the protocol once the COVID-19 pandemic is over.
5 Conclusion
Dofetilide is a safe and effective antiarrhythmic agent which may be used in carefully selected patients even in the extenuating circumstances created by COVID-19. Our study provokes and generates a hypothesis to test the strategy of outpatient initiation of dofetilide in patients with CIEDs in future studies of larger sample size and longer follow-up period, and perhaps even randomized with standard in-patient initiation to further validate our findings.
Data expressed as number (%) or mean + standard deviation
TIA transient ischemic attack
References
Køber L, Bloch Thomsen PE, Møller M, Torp-Pedersen C, Carlsen J, Sandøe E, et al. Camm AJ; Danish Investigations of Arrhythmia and Mortality on Dofetilide (DIAMOND) Study Group. Effect of dofetilide in patients with recent myocardial infarction and left-ventricular dysfunction: a randomised trial. Lancet. 2000;356(9247):2052–8.
Torp-Pedersen C, Møller M, Bloch-Thomsen PE, Køber L, Sandøe E, Egstrup K, et al. Dofetilide in patients with congestive heart failure and left ventricular dysfunction. Danish Investigations of Arrhythmia and Mortality on Dofetilide Study Group. N Engl J Med. 1999;341(12):857–65.
Singh S, Zoble RG, Yellen L, Brodsky MA, Feld GK, Berk M, et al. Efficacy and safety of oral dofetilide in converting to and maintaining sinus rhythm in patients with chronic atrial fibrillation or atrial flutter: the symptomatic atrial fibrillation investigative research on dofetilide (SAFIRE-D) study. Circulation. 2000;102(19):2385–90.
Greenbaum R, Campbell T, Channer K, Dairymple H, Kingma J, Santini M, et al. Conversion of atrial fibrillaton and maintenance of sinus rhythm by dofetilide: the EMERALD (European and Australian multicenter evaluative research on atrial fibrillation dofetilide) study. Circulation. 1998;98:633.
Pedersen OD, Bagger H, Keller N, Marchant B, Køber L, Torp-Pedersen C. Efficacy of dofetilide in the treatment of atrial fibrillation-flutter in patients with reduced left ventricular function: a Danish investigations of arrhythmia and mortality on dofetilide (DIAMOND) substudy. Circulation. 2001;104(3):292–6.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071–104.
Pfizer. Tikosyn™ (dofetilide). U.S. Food and Drug Administration website. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/020931s017lbl.pdf. Revised August 2019. Accessed October 3, 2020.
Kantharia BK, Patel SS, Kulkarni G, Shah AN, Lokhandwala Y, Mascarenhas E, et al. Reuse of explanted permanent pacemakers donated by funeral homes. Am J Cardiol. 2012;109(2):238–40.
Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M, et al. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Circulation. 2020;141(21):e823–31. https://doi.org/10.1161/CIRCULATIONAHA.120.047063.
Campbell T, Greenbaum R, Channer K, Dalrymple H, Kingma JH, Santini M, et al. Mortality in patients with atrial fibrillation-1 year follow up of EMERALD (European and Australian multicenter evaluative research on atrial fibrillation dofetilide). J Am Coll Cardiol. 2000;35:154A–5A.
Sharma SP, Turagam M, Atkins D, Bommana S, Jeffrey C, Newton D, et al. Safety of rapid switching from amiodarone to dofetilide in atrial fibrillation patients with an implantable cardioverter-defibrillator. Heart Rhythm. 2019;16(7):990–5.
Turagam MK, Afzal MR, Reddy M, Pillarisetti J, Lavu M, Atkins D, et al. Practice variation in the re-initiation of dofetilide: an observational study. Int J Cardiol. 2017;236:221–5.
Daoud EG, Glotzer TV, Wyse DG, Ezekowitz MD, Hilker C, Koehler J. Ziegler PD; TRENDS Investigators. Temporal relationship of atrial tachyarrhythmias, cerebrovascular events, and systemic emboli based on stored device data: a subgroup analysis of TRENDS. Heart Rhythm. 2011;8(9):1416–23.
Turakhia MP, Ziegler PD, Schmitt SK, Chang Y, Fan J, Than CT, et al. Atrial fibrillation burden and short-term risk of stroke: case-crossover analysis of continuously recorded heart rhythm from cardiac electronic implanted devices. Circ Arrhythm Electrophysiol. 2015;8(5):1040–7.
Glotzer TV, Daoud EG, Wyse DG, Singer DE, Ezekowitz MD, Hilker C, et al. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009;2(5):474–80.
Mascarenhas DA, Sharma M. Revisiting the role of antiarrhythmic drugs in prevention of atrial fibrillation recurrence: a single center retrospective review. Cardiol Res. 2018;9(3):165–70.
Mascarenhas DAN, Sharma M, Ziegler PD, Kantharia BK. Role of cardiovascular implantable electronic devices in delivering individualized disease-guided management of patients with non-valvular atrial fibrillation and high bleeding risk. Acta Cardiol. 2019;74(2):131–9.
Mascarenhas DA, Farooq MU, Ziegler PD, Kantharia BK. Role of insertable cardiac monitors in anticoagulation therapy in patients with atrial fibrillation at high risk of bleeding. Europace. 2016;18(6):799–806.
Anand V, Vakil K, Tholakanahalli V, Li JM, McFalls E, Adabag S. Discontinuation of dofetilide from QT prolongation and ventricular tachycardia in the real world. JACC Clin Electrophysiol. 2016;2(7):777–81.
Yarlagadda B, Vuddanda V, Dar T, Jazayeri MA, Parikh V, Turagam MK, et al. Safety and efficacy of inpatient initiation of dofetilide versus sotalol for atrial fibrillation. J Atr Fibrillation. 2017;10(4):1805.
Dar T, Murtaza G, Yarlagadda B, Madoukh B, Bravin L, Vuddanda V, et al. Dofetilide initiation and implications of deviation from the standard protocol - a real world experience. J Atr Fibrillation. 2019;12(4):2265.
Dofetilide - StatPearls - NCBI Bookshelf (n.d.) https://www.ncbi.nlm.nih.gov/books/NBK459154/
Coyne KS, Paramore C, Grandy S, Mercader M, Reynolds M, Zimetbaum P. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health. 2006;9(5):348–56.
Lee WC, Lamas GA, Balu S, Spalding J, Wang Q, Pashos CL. Direct treatment cost of atrial fibrillation in the elderly American population: a Medicare perspective. J Med Econ. 2008;11(2):281–98.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mascarenhas, D.A.N., Mudumbi, P.C. & Kantharia, B.K. Outpatient initiation of dofetilide: insights from the complexities of atrial fibrillation management during the COVID-19 lockdown. J Interv Card Electrophysiol 63, 21–28 (2022). https://doi.org/10.1007/s10840-021-00942-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-00942-y