Abstract
Purpose
The ablation index (AI) is a recently developed marker for ablation lesion quality that incorporates contact force (CF), time, and power in a weighted formula. There is a paucity of information on whether AI-guided pulmonary vein isolation (PVI) could improve the outcome in patients with atrial fibrillation (AF). We evaluated the optimal AI threshold for avoiding acute pulmonary vein reconnection (PVR), and to compare the efficacy of optimal AI-targeted PVI with that of conventional CF-guided PVI.
Methods
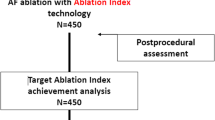
Seventy patients with AF (paroxysmal, 67%) were enrolled. In a phase 1 study, the patients underwent conventional CF-guided PVI (CON group), and the optimal AI threshold for avoiding acute PVR was identified. In phase 2, the patients underwent AI-guided PVI (OAI group). We compared the acute PVR rate between the CON group and the OAI group to demonstrate the efficacy of AI-guided PVI.
Results
In phase 1 (n = 38), acute PVR was observed in 57 of 532 (10.7%) segments. AI values of ≥ 450 at the anterior/roof segments and of ≥ 350 at the posterior/inferior/carina segments were identified as the optimal AI thresholds for avoiding acute PVR. In the phase 2 study targeting those AI values, the OAI group (n = 32) showed a significantly lower acute PVR rate than the CON group (4.2% vs. 10.7%, p < 0.001). The OAI group showed a higher minimum AI and smaller variations in AI values than the CON group.
Conclusions
Optimal AI-targeted PVI is feasible and could improve the acute outcome in patients with AF.
Trial registration
URL: https://www.clinicaltrials.gov. Unique identifier: NCT03389074.





Similar content being viewed by others
References
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962.
Ouyang F, Tilz R, Chun J, Schmidt B, Wissner E, Zerm T, et al. Long-term results of catheter ablation in paroxysmal atrial fibrillation: lessions from a 5-year follow-up. Circulation. 2010;122:2368–77.
Nery PB, Belliveau D, Nair GM, Bernick J, Redpath CJ, Szczotka A, et al. Relationship between pulmonary vein reconnection and atrial fibrillation recurrence: a systematic review and meta-analysis. JACC Clin Electrophysiol. 2016;2:474–83.
Barnett AS, Bahnson TD, Piccini JP. Recent advances in lesion formation for catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2016;9(5):e003299.
Natale A, Reddy VY, Monir G, Wilber DJ, Lindsay BD, McElderry HT, et al. Paroxysmal AF catheter ablation with a contact force sensing catheter: results of the prospective, multicenter SMART-AF trial. J Am Coll Cardiol. 2014;64:647–56.
Reddy VY, Dukkipati SR, Neuzil P, Natale A, Albengue JP, Kautzner J, et al. Randomized, controlled trial of the safety and effectiveness of a contact force-sensing irrigated catheter for ablation of paroxysmal atrial fibrillation: results of the TactiCath contact force ablation catheter study for atrial fibrillation (TOCCASTAR) study. Circulation. 2015;132:907–15.
Kautzner J, Neuzil P, Lambert H, Peichl P, Petru J, Cihak R, et al. EFFICAS II: optimization of catheter contact force improves outcome of pulmonary vein isolation for paroxysmal atrial fibrillation. Europace. 2015;17:1229–35.
Ullah W, McLean A, Tayebjee MH, Gupta D, Ginks MR, Haywood GA, et al. Randomized trial comparing pulmonary vein isolation using the SmartTouch catheter with or without real-time contact force data. Heart Rhythm. 2016;13:1761–7.
Das M, Loveday JJ, Wynn GJ, Gomes S, Saeed Y, Bonnett LJ, et al. Ablation index, a novel marker of ablation lesion quality: prediction of pulmonary vein reconnection at repeat electrophysiology study and regional differences in target values. Europace. 2017;19:775–83.
Wittkampf FH, Hauer RN, Robles de Medina EO. Control of radiofrequency lesion size by power regulation. Circulation. 1989;80:962–8.
David EH. Determinants of lesion size during radiofrequency catheter ablation: the role of electrode-tissue contact pressure and duration of energy delivery. J Cardiovasc Electrophysiol. 1991;6:509–15.
Ikeda A, Nakagawa H, Lambert H, Shah DC, Fonck E, Yulzari A, et al. Relationship between catheter contact force and radiofrequency lesion size and incidence of steam pop in the beating canine heart: electrogram amplitude, impedance, and electrode temperature are poor predictors of electrode-tissue contact force and lesion size. Circ Arrhythm Electrophysiol. 2014;7:1174–80.
Squara F, Latcu DG, Massaad Y, Mahjoub M, Bun SS, Saoudi N. Contact force and force-time integral in atrial radiofrequency ablation predict transmurality of lesions. Europace. 2014;16:660–7.
Neuzil P, Reddy VY, Kautzner J, Petru J, Wichterle D, Shah D, et al. Electrical reconnection after pulmonary vein isolation is contingent on contact force during initial treatment: results from the EFFICAS I study. Circ Arrhythm Electrophysiol. 2013;6:327–33.
Nakagawa H, Ikeda A, Govari A, Papaioannou T, Constantine G, Bar-Tal M. Prospective study using a new formula incorporating contact force, radiofrequency power and application time (force-power-time index) for quantifying lesion formation to guide long continuous atrial lesions in the beating canine heart. Circulation. 2013;128:A12104.
Suenari K, Nakano Y, Hirai Y, Ogi H, Oda N, Makita Y, et al. Left atrial thickness under the catheter ablation lines in patients with paroxysmal atrial fibrillation: insights from 64-slice multidetector computed tomography. Heart Vessel. 2013;28:360–8.
Ganesan AN, Shipp NJ, Brooks AG, Kuklik P, Lau DH, Lim HS, et al. Long-term outcomes of catheter ablation of atrial fibrillation: a systemic review and meta-analysis. J Am Heart Assoc. 2018;2:e004549.
Shah DC, Lambert H, Nakagawa H, Langenkamp A, Aeby N, Leo G. Area under the real-time contact force curve (force-time integral) predicts radiofrequency lesion size in an in vitro contractile model. J Cardiovasc Electrophysiol. 2010;21:1038–43.
Kumar S, Morton JB, Lee J, Halloran K, Spence SJ, Gorelik A, et al. Prospective characterization of catheter-tissue contact force at different anatomic sites during antral pulmonary vein isolation. Circ Arrhythm Electrophysiol. 2012;5:1124–9.
Schluermann F, Krauss T, Biermann J, Hartmann M, Trolese L, Pache G, et al. In vivo contact force measurements and correlation with left atrial anatomy during catheter ablation of atrial fibrillation. Europace. 2015;17:1526–32.
Reddy VY, Pollak S, Lindsay BD, McElderry HT, Natale A, Kantipudi C, et al. Relationship between catheter stability and 12-month success atrial pulmonary vein isolation: a subanalysis of the SMART-AF trial. JACC Clin Electrophysiol. 2016;2:691–9.
Münkler P, Kröger S, Liosis S, Abdin A, Lyan E, Eitel C, et al. Ablation index for catheter ablation of atrial fibrillation – clinical applicability and comparison with force-time integral. Circ J. 2018;82:2722–7. https://doi.org/10.1253/circj.CJ-18-0361.
El Haddad M, Taghji P, Phlips T, Wolf M, Demolder A, Choudhury R, et al. Determinants of acute and late pulmonary vein reconnection in contact force-guided pulmonary vein isolation: identifying the weakest link in the ablation chain. Circ Arrhythm Electrophysiol. 2017;10(4):3004867.
Taghji P, El Haddad M, Phlips T, Wolf M, Knecht S, Vandekerckhove Y, et al. Evaluation of a strategy aiming to enclose the pulmonary veins with contiguous and optimized radiofrequency lesions in paroxysmal atrial fibrillation: a pilot study. JACC Clin Electrophysiol. 2018;4:99–108.
Hussein A, Das M, Riva S, Morgan M, Ronayne C, Sahni A, et al. Use of ablation index-guided ablation results in high rates of durable pulmonary vein isolation and freedom from arrhythmia in persistent atrial fibrillation patients. Circ Arrhythm Electrophysiol. 2018;11:e006576.
Phlips T, Taghji P, El Haddad M, Wolf M, Knecht S, Vandekerckhove Y, et al. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. Europace. 2018;20:f419–27. https://doi.org/10.1093/europace/eux376.
Tanaka N, Inoue K, Tanaka K, Toyoshima Y, Oka T, Okada M, et al. Automated ablation annotation algorithm reduces re-conduction of isolated pulmonary vein and improves outcome after catheter ablation for atrial fibrillation. Circ J. 2017;81:1596–602.
Acknowledgments
We thank Cho-Rong Jeong, Ji Seon Park, Jiseon Lee, and Junyeop Yeo for their assistance.
Funding
This research was conducted with support from the investigator-initiated study program of Biosense Webster, Inc. (IIS 457).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SRL, EJL, WSC, MJC, SO declare that they have no conflict of interest. EKC received a research grant from Daiichi-Sankyo, BMS/Pfizer, and Biosense Webster.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 1345 kb)
Rights and permissions
About this article
Cite this article
Lee, SR., Choi, EK., Lee, EJ. et al. Efficacy of the optimal ablation index–targeted strategy for pulmonary vein isolation in patients with atrial fibrillation: the OPTIMUM study results. J Interv Card Electrophysiol 55, 171–181 (2019). https://doi.org/10.1007/s10840-019-00565-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00565-4