Abstract
Purpose
The use of oral anticoagulation (OAC) in the elderly population with atrial fibrillation (AF) treated in long-term care (LTC) facilities is inconsistent. We examined the magnitude and sources of the gap between indicated and prescribed OAC in the elderly population with AF.
Methods
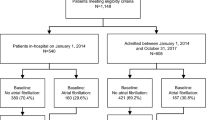
We retrospectively scanned the electronic medical record (EMR) and pharmacy data of 25 LTC facilities in Ontario, Canada. The diagnosis of AF was drawn from EMR. Different attributable risk factors for possible failure to prescribe OAC were examined.
Results
In total, 3378 active resident data were examined in the 25 LTC facilities. All the residents were ≥65 years old with mean age of 85 ± 8 years and 2449 (72%) were female. We identified 433 (13%) residents with AF with mean age 87 ± 7 years and mean CHADS2 score of 3 ± 1. Out of all residents with AF, 273 (63%) were on OAC therapy. Residents were mostly treated with warfarin (N = 114 (42%)), rivaroxaban (N = 71 (26%)) or apixaban (N = 62 (23%)) followed by dabigatran (N = 26 (10%)). Antiplatelet drugs as the only stroke prevention therapy were used in 88 (20%) residents, and 28 (6%) residents were on anticoagulation and antiplatelet drugs. Seventy-two (17%) residents were not on any antiplatelet or antithrombotic therapy. None of the potential attributable risks identified consistently correlated with the failure to prescribe indicated therapy.
Conclusions
This data set suggests that 37% of eligible elderly LTC residents failed to receive recommended stroke prevention therapies.

Similar content being viewed by others
References
Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–6.
Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke J Cereb Circ. 2005;36:1115–9.
Andersson T, Magnuson A, Bryngelsson IL, Frobert O, Henriksson KM, Edvardsson N, et al. Gender-related differences in risk of cardiovascular morbidity and all-cause mortality in patients hospitalized with incident atrial fibrillation without concomitant diseases: a nationwide cohort study of 9519 patients. Int J Cardiol. 2014;177:91–9.
Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124.
Verma A, Cairns JA, Mitchell LB, Macle L, Stiell IG, Gladstone D, et al. 2014 focused update of the Canadian Cardiovascular Society Guidelines for the management of atrial fibrillation. Can J Cardiol. 2014;30:1114–30.
Devereaux PJ, Anderson DR, Gardner MJ, Putnam W, Flowerdew GJ, Brownell BF, et al. Differences between perspectives of physicians and patients on anticoagulation in patients with atrial fibrillation: observational study. BMJ. 2001;323:1218–22.
Friberg L, Bergfeldt L. Atrial fibrillation prevalence revisited. J Intern Med. 2013;274:461–8.
Friberg L, Rosenqvist M, Lindgren A, Terent A, Norrving B, Asplund K. High prevalence of atrial fibrillation among patients with ischemic stroke. Stroke J Cereb Circ. 2014;45:2599–605.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67.
You JJ, Singer DE, Howard PA, Lane DA, Eckman MH, Fang MC, et al. Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis, 9th edn: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e531S-75S.
Lip GY, Larsen TB, Skjoth F, Rasmussen LH. Indirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillation. J Am Coll Cardiol. 2012;60:738–46.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62.
Ng KH, Shestakovska O, Connolly SJ, Eikelboom JW, Avezum A, Diaz R, et al. Efficacy and safety of apixaban compared with aspirin in the elderly: a subgroup analysis from the AVERROES trial. Age Ageing. 2016;45:77–83.
Angaran P, Dorian P, Tan MK, Kerr CR, Green MS, Gladstone DJ, et al. The risk stratification and stroke prevention therapy care gap in Canadian atrial fibrillation patients. Can J Cardiol. 2016;32:336–43.
Atarashi H, Inoue H, Okumura K, Yamashita T, Kumagai N, Origasa H, et al. Present status of anticoagulation treatment in Japanese patients with atrial fibrillation: a report from the J-RHYTHM registry. Circ J Offic J Japan Circ Soc. 2011;75:1328–33.
Hsu JCMTMKKF, Katz DF, Marzec LN, Lubitz SA, Gehi AK, Turakhia MP, et al. Oral anticoagulant therapy prescription in patients with atrial fibrillation across the spectrum of stroke risk insights from the NCDR PINNACLE registry. JAMA Cardiol. 2016.
Mahmud A, Bennett K, Okechukwu I, Feely J. National underuse of anti-thrombotic therapy in chronic atrial fibrillation identified from digoxin prescribing. Br J Clin Pharmacol. 2007;64:706–9.
McAlister FA. The end of the risk–treatment paradox? A rising tide lifts all boats. JACC. 2011;58(17):1766–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Sources of funding
None
Additional information
Abstract presentation
The gap between indicated and prescribed stroke prevention therapies in a high-risk geriatric population in Ontario. AHA Conference. Circulation. 2015;132:A17022
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 61 kb)
Rights and permissions
About this article
Cite this article
Shurrab, M., Crystal, E., O’Donnell, D. et al. The gap between indicated and prescribed stroke prevention therapies in a high-risk geriatric population. J Interv Card Electrophysiol 48, 261–266 (2017). https://doi.org/10.1007/s10840-017-0223-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-017-0223-0