Abstract
Background
Atrial fibrillation (AF) is the most common cardiac arrhythmia. AF incidence increases with age. AF ablation procedures are routinely performed under deep sedation with propofol. The purpose of the study was to evaluate if propofol deep sedation during AF ablation is safe in elderly patients.
Methods
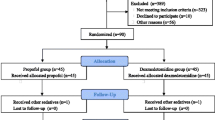
Four hundred one consecutive patients (mean age, 61.4 ± 11.1 years; range, 20–82; 66.3 % men) who were presented to our institution for ablation of symptomatic AF were enrolled. Patients were divided into three groups: Patients in group A were ≤50 years old; patients in group B were 51–74 years old; and patients in group C were ≥75 years old. Procedures were performed under deep sedation with propofol, midazolam, and piritramide. SaO2, electrocardiogram, arterial blood pressure, and arterial blood gas were monitored throughout the procedure. Sedation-related complications, intraprocedural complications, and other adverse events were evaluated. Fisher exact or χ 2 tests were used for comparison of adverse events and complications among groups. Analysis of variance was used to compare sedation- and procedure-related parameters.
Results
Fifty-three (13.2 %) elderly patients were in group C and were compared to 73 (18.2 %) patients in group A and 275 (68.8 %) in group B. No significant differences in sedation-related or intraprocedural complications were seen (group A, 1.4 %; group B, 1.1 %; group C, 3.7 %; p = 0.336). Despite a significantly greater drop in systolic blood pressure in under sedation in group C (group A, 15.5 ± 9.5 mmHg; group B, 18.9 ± 16.3 mmHg; group C, 32.3 ± 15.5 mmHg; p < 0.001), no prolonged hypotension was observed. The rate of other adverse events (delirium, respiratory infection, renal failure) was significantly higher in group C (9.4 %), compared to group A (0 %) and group B (2.2 %; p = 0.004).
Conclusion
Deep sedation with propofol and midazolam during AF ablation did not result in an increased rate in sedation-related complications in elderly patients. Similarly, the rate of procedural complications was not significantly different among the study groups. The rate of respiratory infections and renal failure was significantly higher in the elderly. All adverse events were treated successfully without any remaining sequelae.
Similar content being viewed by others
References
Camm, A. J., Lip, G. Y., De Caterina, R., Savelieva, I., Atar, D., Hohnloser, S. H., et al. (2012). 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. European Heart Journal, 33(21), 2719–2747.
Miyasaka, Y., Barnes, M. E., Gersh, B. J., Cha, S. S., Bailey, K. R., Abhayaratna, W. P., et al. (2006). Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation, 114(2), 119–125.
Reynolds, M. R., & Essebag, V. (2012). Economic burden of atrial fibrillation: implications for intervention. American Journal of Pharmacy Benefits, 4(2), 58–65.
Calkins, H., Kuck, K. H., Cappato, R., Brugada, J., Camm, A. J., Chen, S. A., et al. (2012). 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Journal of Interventional Cardiac Electrophysiology, 33, 171–257.
Yamada, T., & Kay, G. N. (2009). Catheter ablation of atrial fibrillation in the elderly. Pacing and Clinical Electrophysiology, 32(8), 1085–1091.
Miner, J. R., & Burton, J. H. (2007). Clinical practice advisory: emergency department procedural sedation with propofol. Annals of Emergency Medicine, 50(2), 182–187.
Coté, G. A., Hovis, R. M., Ansstas, M. A., Waldbaum, L., Azar, R. R., Early, D. S., Edmundowicz, S. A., Mullady, D. K., Jonnalagadda, S. S., et al. (2010). Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clinical Gastroenterology and Hepatology, 8(2), 137–142.
Lü, F., Lin, J., & Benditt, D. G. (2013). Conscious sedation and anesthesia in the cardiac electrophysiology laboratory. Journal of Cardiovascular Electrophysiology, 24, 237–245.
Wutzler, A., Rolf, S., Huemer, M., Parwani, A. S., Boldt, L. H., Herberger, E., et al. (2012). Safety aspects of deep sedation during catheter ablation of atrial fibrillation. Pacing and Clinical Electrophysiology, 35, 38–43.
Salukhe, T. V., Willems, S., Drewitz, I., Steven, D., Hoffmann, B. A., Heitmann, K., et al. (2012). Propofol sedation administered by cardiologists without assisted ventilation for long cardiac interventions: an assessment of 1000 consecutive patients undergoing atrial fibrillation ablation. Europace, 14(3), 325–330.
Kottkamp, H., Hindricks, G., Eitel, C., Müller, K., Siedziako, A., Koch, J., et al. (2011). Deep sedation for catheter ablation of atrial fibrillation: a prospective study in 650 consecutive patients. Journal of Cardiovascular Electrophysiology, 22(12), 1339–1343.
Rostykus, P. S., McDonald, G. B., & Albert, R. K. (1980). Upper intestinal endoscopy induces hypoxemia in patients with obstructive pulmonary disease. Gastroenterology, 78, 488–491.
Nishikawa, K., Kanaya, N., Kawamata, M., & Namiki, A. (2004). Left ventricular mechanical performance in elderly patients after induction of anaesthesia. A comparison of inhalational induction with sevoflurane and intravenous induction with fentanyl and propofol. Anaesthesia, 59(10), 948–953.
Tang, R. B., Dong, J. Z., Zhao, W. D., Liu, X. P., Kang, J. P., Long, D. Y., et al. (2007). Unconscious sedation/analgesia with propofol versus conscious sedation with fentanyl/midazolam for catheter ablation of atrial fibrillation: a prospective, randomized study. Chinese Medical Journal, 120, 2036–2038.
Raftery, S., & Sherry, E. (1992). Total intravenous anaesthesia with propofol and alfentanil protects against postoperative nausea and vomiting. Canadian Journal of Anaesthesia, 39, 37–40.
Nishikawa, K., Nakayama, M., Omote, K., & Namiki, A. (2004). Recovery characteristics and post-operative delirium after long-duration laparoscope-assisted surgery in elderly patients: propofol-based vs. sevoflurane-based anesthesia. Acta Anaesthesiologica Scandinavica, 48(2), 162–168.
Beller, J. P., Pottecher, T., Mangin, P., Fratte, C., & Otteni, J. C. (1987). Long-term sedation with propofol during intensive care. Preliminary results of the recovery and pharmacokinetics. Annales Françaises d’Anesthésie et de Réanimation, 6, 334–335.
Weaver, C. S., Terrell, K. M., Bassett, R., Swiler, W., Sandford, B., Avery, S., et al. (2011). ED procedural sedation of elderly patients: is it safe? The American Journal of Emergency Medicine, 29(5), 541–544.
Piccini, J. P., Sinner, M. F., Greiner, M. A., Hammill, B. G., Fontes, J. D., Daubert, J. P., et al. (2012). Outcomes of medicare beneficiaries undergoing catheter ablation for atrial fibrillation. Circulation, 126(18), 2200–2207.
Kusumoto, F., Prussak, K., Wiesinger, M., Pullen, T., & Lynady, C. (2009). Radiofrequency catheter ablation of atrial fibrillation in older patients: outcomes and complications. Journal of Interventional Cardiac Electrophysiology, 25(1), 31–35.
Evans, C. T., LaVela, S. L., Weaver, F. M., Priebe, M., Sandford, P., Niemiec, P., et al. (2008). Epidemiology of hospital-acquired infections in veterans with spinal cord injury and disorder. Infection Control and Hospital Epidemiology, 29(3), 234–242.
Laurent, M., Bories, P. N., Le Thuaut, A., Liuu, E., Ledudal, K., Bastuji-Garin, S., et al. (2012). Impact of comorbidities on hospital-acquired infections in a geriatric rehabilitation unit: prospective study of 252 patients. Journal of the American Medical Directors Association, 13(8), 760.e7–760.e12.
Kikuchi, R., Watabe, N., Konno, T., Mishina, N., Sekizawa, K., & Sasaki, H. (1994). High incidence of silent aspiration in elderly patients with community acquired pneumonia. American Journal of Respiratory and Critical Care Medicine, 150(1), 251–253.
Bowles, C. J., Leicester, R., Romaya, C., Swarbrick, E., Williams, C. B., & Epstein, O. (2004). A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut, 53(2), 277–283.
Marik, P. E. (2001). Aspiration pneumonitis and aspiration pneumonia. The New England Journal of Medicine, 344(9), 665–671.
Green, S. M., & Krauss, B. (2002). Pulmonary aspiration risk during emergency department procedural sedation—an examination of the role of fasting and sedation depth. Academic Emergency Medicine, 9(1), 35–42.
Conflict of interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wutzler, A., Loehr, L., Huemer, M. et al. Deep sedation during catheter ablation for atrial fibrillation in elderly patients. J Interv Card Electrophysiol 38, 115–121 (2013). https://doi.org/10.1007/s10840-013-9817-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-013-9817-3