Abstract
Background
Determination of the defibrillation safety margin (DSM) is the most common method of testing device effectiveness at the time of implantation of implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy defibrillator (CRTD). Low DSM remains a problem in clinical practice.
Objective
The purpose of this study is to ascertain the incidence and clinical predictors of low DSM and the treatment strategies for low DSM in ICD or CRTD recipients.
Methods
Selected ICD or CRTD recipients from January 2006 to May 2008 who underwent DSM test at the time of implantation were included. Low DSM patients were defined as patients who had a DSM within 10 J of the maximum delivered energy of the device. These patients were compared to patients who had DSM > 10 J.
Results
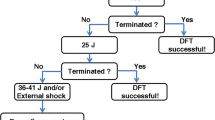
This study included 243 patients. Of these, 13 (5.3%) patients had low DSM, and 230 patients had adequate DSM. Patients with low DSM had a high prevalence of amiodarone use (69% vs 13%, p < 0.01), secondary prevention indications (69% vs 30%, p < 0.01), and a trend toward younger age (51 ± 18 vs 58 ± 15 years, p = 0.08). After adjustment for age and sex, amiodarone use was significantly associated with low DSM. All low DSM patients except one obtained adequate DSM after taking additional steps, including discontinuing amiodarone and starting sotalol, RV lead repositioning, adding a subcutaneous array or shock coil, changing single-coil to dual-coil lead, and upgrading to a high output device.
Conclusion
The incidence of low DSM patients is low with high-energy devices. Amiodarone use is associated with low DSM, and its discontinuation or substitution with sotalol is one of a variety of available options for low DSM patients.
Similar content being viewed by others
References
Birnie, D., Tung, S., Simpson, C., Crystal, E., Exner, D., Paredes, F. A., et al. (2008). Complications associated with defibrillation threshold testing: the Canadian experience. Heart Rhythm, 5, 387–390.
Marchlinski, F. E., Flores, B., Miller, J. M., Gottlieb, C. D., & Hargrove, W. C., 3rd. (1988). Relation of the intraoperative defibrillation threshold to successful postoperative defibrillation with an automatic implantable cardioverter defibrillator. The American Journal of Cardiology, 62, 393–398.
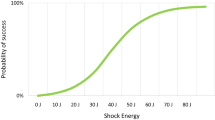
Strickberger, S. A., Daoud, E. G., Davidson, T., Weiss, R., Bogun, F., Knight, B. P., et al. (1997). Probability of successful defibrillation at multiples of the defibrillation energy requirement in patients with an implantable defibrillator. Circulation, 96, 1217–1223.
Neuzner, J., Liebrich, A., Jung, J., Himmrich, E., Pitschner, H. F., Winter, J., et al. (1999). Safety and efficacy of implantable defibrillator therapy with programmed shock energy at twice the augmented step-down defibrillation threshold: results of the prospective, randomized, multicenter low-energy Endotak trial. The American Journal of Cardiology, 83, 34D–39D.
Barold, S. S., Herweg, B., & Curtis, A. B. (2005). The defibrillation safety margin of patients receiving ICDs: a matter of definition. Pacing and Clinical Electrophysiology, 28, 881–882.
Gold, M. R., Higgins, S., Klein, R., Gilliam, F. R., Kopelman, H., Hessen, S., et al. (2002). Efficacy and temporal stability of reduced safety margins for ventricular defibrillation: primary results from the Low Energy Safety Study (LESS). Circulation, 105, 2043–2048.
Russo, A. M., Sauer, W., Gerstenfeld, E. P., Hsia, H. H., Lin, D., Cooper, J. M., et al. (2005). Defibrillation threshold testing: is it really necessary at the time of implantable cardioverter defibrillator insertion? Heart Rhythm, 2, 456–461.
Shukla, H. H., Flaker, G. C., Jayam, V., & Roberts, D. (2003). High defibrillation thresholds in transvenous biphasic implantable defibrillators: clinical predictors and prognostic implications. Pacing and Clinical Electrophysiology, 26, 44–48.
Mainigi, S. K., Cooper, J. M., Russo, A. M., Nayak, H. M., Lin, D., Dixit, S., et al. (2006). Elevated defibrillation thresholds in patients undergoing biventricular defibrillator implantation: incidence and predictors. Heart Rhythm, 3, 1010–1016.
Theuns, D. A., Szili-Torok, T., & Jordaens, L. J. (2005). Defibrillation efficacy testing: long-term follow-up and mortality. Europace, 7, 509–515.
de Lima, C. E., Martinelli Filho, M., Silva, R. T., Tamaki, W. T., de Oliveira, J. C., Martins, D. C., et al. (2008). ICD patients with elevated defibrillation threshold: clinical behavior and therapeutic alternatives. Arquivos Brasileiros de Cardiologia, 90(3), 160–166.
Gold, M. R., Khalighi, K., Kavesh, N. G., Daly, B., Peters, R. W., & Shorofsky, S. R. (1997). Clinical predictors of transvenous biphasic defibrillation thresholds. The American Journal of Cardiology, 79(12), 1623–1627.
Pinski, S. L., Vanerio, G., Castle, L. W., Morant, V. A., Simmons, T. W., Trohman, R. G., et al. (1991). Patients with a high defibrillation threshold: clinical characteristics, management, and outcome. American Heart Journal, 122(1 Pt 1), 89–95.
Higgins, S., Mann, D., Calkins, H., Estes, N. A., Strickberger, S. A., Breiter, D., et al. (2005). One conversion of ventricular fibrillation is adequate for implantable cardioverter-defibrillator implant: an analysis from the Low Energy Safety Study (LESS). Heart Rhythm, 2(2), 117–122.
Epstein, A. E., Ellenbogen, K. A., Kirk, K. A., Kay, G. N., Dailey, S. M., & Plumb, V. J. (1992). Clinical characteristics and outcome of patients with high defibrillation thresholds: a multicenter study. Circulation, 86, 1206–1216.
Raitt, M. H., Johnson, G., Dolack, G. L., Poole, J. E., Kudenchuk, P. J., & Bardy, G. H. (1995). Clinical predictors of the defibrillation threshold with the unipolar implantable defibrillation system. Journal of the American College of Cardiology, 25, 1576–1583.
Khalighi, K., Daly, B., Leino, E. V., Shorofsky, S. R., Kavesh, N. G., Peters, R. W., et al. (1997). Clinical predictors of transvenous defibrillation energy requirements. The American Journal of Cardiology, 79(2), 150–153.
Fain, E. S., Lee, J. T., & Winkle, R. A. (1987). Effects of acute intravenous and chronic oral amiodarone on defibrillation energy requirements. American Heart Journal, 114(1 Pt 1), 8–17.
Hohnloser, S. H., Dorian, P., Roberts, R., Gent, M., Israel, C. W., Fain, E., et al. (2006). Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation, 114(2), 104–109.
Kühlkamp, V., Mewis, C., Suchalla, R., Mermi, J., Dörnberger, V., & Seipel, L. (1999). Effect of amiodarone and sotalol on the defibrillation threshold in comparison to patients without antiarrhythmic drug treatment. International Journal of Cardiology, 69(3), 271–279.
Huang, S. K., Tan de Guzman, W. L., Chenarides, J. G., Okike, N. O., & Vander Salm, T. J. (1991). Effects of long-term amiodarone therapy on the defibrillation threshold and the rate of shocks of the implantable cardioverter-defibrillator. American Heart Journal, 122(3 Pt 1), 720–727.
Schuger, C., Ellenbogen, K. A., Faddis, M., Knight, B. P., Yong, P., Sample, R., & VENTAK CHF/CONTAK CD Study Investigators. (2006). Defibrillation energy requirements in an ICD population receiving cardiac resynchronization therapy. Journal of Cardiovascular Electrophysiology, 17(3), 247–250.
Zima, E., Gergely, M., Soós, P., Gellér, L. A., Nemes, A., Acsády, G., et al. (2006). The effect of induction method on defibrillation threshold and ventricular fibrillation cycle length. Journal of Cardiovascular Electrophysiology, 17(4), 377–381.
Huang, J., Skinner, J. L., Rogers, J. M., Smith, W. M., Holman, W. L., & Ideker, R. E. (2002). The effects of acute and chronic amiodarone on activation patterns and defibrillation threshold during ventricular fibrillation in dogs. Journal of the American College of Cardiology, 40(2), 375–383.
Frame, L. H. (1989). The effect of chronic oral and acute intravenous amiodarone administration on ventricular defibrillation threshold using implanted electrodes in dogs. Pacing and Clinical Electrophysiology, 12(2), 339–346.
Arredondo, M. T., Guillen, S. G., & Quinteiro, R. A. (1986). Effect of amiodarone on ventricular fibrillation and defibrillation thresholds in the canine heart under normal and ischemic conditions. European Journal of Pharmacology, 125(1), 23–28.
Zhou, L., Chen, B. P., Kluger, J., Fan, C., & Chow, M. S. (1998). Effects of amiodarone and its active metabolite desethylamiodarone on the ventricular defibrillation threshold. Journal of the American College of Cardiology, 31(7), 1672–1678.
Boriani, G., Biffi, M., Frabetti, L., Maraschi, M., & Branzi, A. (2000). High defibrillation threshold at cardioverter defibrillator implantation under amiodarone treatment: favorable effects of D, L-sotalol. Heart & Lung, 29(6), 412–416.
Pelosi, F., Jr., Oral, H., Kim, M. H., Sticherling, C., Horwood, L., Knight, B. P., et al. (2000). Effect of chronic amiodarone therapy on defibrillation energy requirements in humans. Journal of Cardiovascular Electrophysiology, 11(7), 736–740.
Nielsen, T. D., Hamdan, M. H., Kowal, R. C., Barbera, S. J., Page, R. L., & Joglar, J. A. (2001). Effect of acute amiodarone loading on energy requirements for biphasic ventricular defibrillation. The American Journal of Cardiology, 88(4), 446–448.
Daoud, E. G., Man, K. C., Horwood, L., Morady, F., & Strickberger, S. A. (1997). Relation between amiodarone and desethylamiodarone plasma concentrations and ventricular defibrillation energy requirements. The American Journal of Cardiology, 79(1), 97–100.
Jung, W., Manz, M., Pizzulli, L., Pfeiffer, D., & Lüderitz, B. (1992). Effects of chronic amiodarone therapy on defibrillation threshold. The American Journal of Cardiology, 70(11), 1023–1027.
Ware, D. L., Brooks, M. J., Atkinson, J. B., & Echt, D. S. (1993). Ventricular defibrillation in canines with chronic infarction, and effects of lidocaine and procainamide. Pacing and Clinical Electrophysiology, 16, 337–346.
Echt, D. S., Black, J. N., Barbey, J. T., Coxe, D. R., & Cato, E. (1989). Evaluation of antiarrhythmic drugs on defibrillation energy requirements in dogs: sodium channel block and action potential prolongation. Circulation, 79, 1106–1117.
Simon, R. D., Sturdivant, J. L., Leman, R. B., Wharton, J. M., & Gold, M. R. (2009). The effect of dofetilide on ventricular defibrillation thresholds. Pacing and Clinical Electrophysiology, 32(1), 24–28.
Torp-Pedersen, C., Møller, M., Bloch-Thomsen, P. E., Køber, L., Sandøe, E., Egstrup, K., et al. (1999). Dofetilide in patients with congestive heart failure and left ventricular dysfunction. Danish Investigations of Arrhythmia and Mortality on Dofetilide Study Group. The New England Journal of Medicine, 341(12), 857–865.
Dorian, P., Fain, E. S., Davy, J. M., & Winkle, R. A. (1986). Lidocaine causes a reversible, concentration-dependent increase in defibrillation energy requirements. Journal of the American College of Cardiology, 8(2), 327–332.
Dorian, P., Newman, D., Sheahan, R., Tang, A., Green, M., & Mitchell, J. (1996). d-Sotalol decreases defibrillation energy requirements in humans: a novel indication for drug therapy. Journal of Cardiovascular Electrophysiology, 7(10), 952–961.
Wang, M., & Dorian, P. (1989). DL and D sotalol decrease defibrillation energy requirements. Pacing and Clinical Electrophysiology, 12(9), 1522–1529.
Dorian, P., Newman, D., Harris, L., & Downar, E. (1994). Sotalol in patients with implanted automatic defibrillators: effects on defibrillation and comparison with amiodarone. Canadian Journal of Cardiology, 10(2), 193–200.
Fotuhi, P. C., Kenknight, B. H., Melnick, S. B., Smith, W. M., Baumann, G. F., & Ideker, R. E. (1997). Effect of a passive endocardial electrode on defibrillation efficacy of a nonthoracotomy lead system. Journal of the American College of Cardiology, 29(4), 825–830.
Usui, M., Walcott, G. P., KenKnight, B. H., Walker, R. G., Rollins, D. L., Smith, W. M., et al. (1995). Influence of malpositioned transvenous leads on defibrillation efficacy with and without a subcutaneous array electrode. Pacing and Clinical Electrophysiology, 18(11), 2008–2016.
Winter, J., Zimmermann, N., Lidolt, H., Dees, H., Perings, C., Vester, E. G., et al. (2000). Optimal method to achieve consistently low defibrillation energy requirements. The American Journal of Cardiology, 86(9A), 71K–75K.
Rashba, E. J., Bonner, M., Wilson, J., Shorofsky, S. R., Peters, R. W., & Gold, M. R. (2003). Distal right ventricular coil position reduces defibrillation thresholds. Journal of Cardiovascular Electrophysiology, 14(10), 1036–1040.
Winter, J., Heil, J. E., Schumann, C., Lin, Y., Schannwell, C. M., Michel, U., et al. (1998). Effect of implantable cardioverter/defibrillator lead placement in the right ventricle on defibrillation energy requirements. A combined experimental and clinical study. European Journal of Cardio-Thoracic Surgery, 14(4), 419–425.
Roberts, P. R., Allen, S., Betts, T., Urban, J. F., Euler, D. E., Crick, S., et al. (2000). A multifilamented electrode in the middle cardiac vein reduces energy requirements for defibrillation in the pig. Heart, 84(4), 425–430.
Roberts, P. R., Urban, J. F., Euler, D. E., Kallok, M. J., & Morgan, J. M. (1999). The middle cardiac vein—a novel pathway to reduce the defibrillation threshold. Journal of Interventional Cardiac Electrophysiology, 3(1), 55–60.
Roberts, P. R., Urban, J. F., Betts, T., Allen, S., Dietz, A., Euler, D. E., et al. (2000). Reduction in defibrillation threshold using an auxiliary shock delivered in the middle cardiac vein. Pacing and Clinical Electrophysiology, 23(8), 1278–1282.
Paisey, J. R., Yue, A. M., Bessoule, F., Roberts, P. R., & Morgan, J. M. (2006). Passive electrode effect reduces defibrillation threshold in bi-filament middle cardiac vein defibrillation. Europace, 8(2), 113–117.
Roberts, P. R., Paisey, J. R., Betts, T. R., Allen, S., Whitman, T., Bonner, M., et al. (2003). Comparison of coronary venous defibrillation with conventional transvenous internal defibrillation in man. Journal of Interventional Cardiac Electrophysiology, 8(1), 65–70.
Kuhlkamp, V., Dornberger, V., Khalighi, K., Mewis, C., Suchalla, R., Ziemer, G., et al. (1998). Effect of a single element subcutaneous array electrode added to a transvenous electrode configuration on the defibrillation field and the defibrillation threshold. Pacing and Clinical Electrophysiology, 21(12), 2596–2605.
Gradaus, R., Block, M., Seidl, K., Brunn, J., Isgro, F., Hammel, D., et al. (2001). Defibrillation efficacy comparing a subcutaneous array electrode versus an “active can” implantable cardioverter defibrillator and a subcutaneous array electrode in addition to an “active can” implantable cardioverter defibrillator: results from active can versus array trials I and II. Journal of Cardiovascular Electrophysiology, 12(8), 921–927.
Jordaens, L., Vertongen, P., & van Belleghem, Y. (1993). A subcutaneous lead array for implantable cardioverter defibrillators. Pacing and Clinical Electrophysiology, 16(7 Pt 1), 1429–1433.
Higgins, S. L., Alexander, D. C., Kuypers, C. J., & Brewster, S. A. (1995). The subcutaneous array: a new lead adjunct for the transvenous ICD to lower defibrillation thresholds. Pacing and Clinical Electrophysiology, 18(8), 1540–1548.
Gold, M. R., Olsovsky, M. R., Pelini, M. A., Peters, R. W., & Shorofsky, S. R. (1998). Comparison of single- and dual-coil active pectoral defibrillation lead systems. Journal of the American College of Cardiology, 31(6), 1391–1394.
Rashba, E. J., Olsovsky, M. R., Shorofsky, S. R., Kirk, M. M., Peters, R. W., & Gold, M. R. (2001). Temporal decline in defibrillation thresholds with an active pectoral lead system. Journal of the American College of Cardiology, 38(4), 1150–1155.
Mainigi, S. K., & Callans, D. J. (2006). How to manage the patient with a high defibrillation threshold. Heart Rhythm, 3(4), 492–495.
Conflict of interest
Paul J Wang is consultant for Medtronic, Inc. No other conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cheng, Z., Turakhia, M., Lo, R. et al. Incidence and clinical predictors of low defibrillation safety margin at time of implantable defibrillator implantation. J Interv Card Electrophysiol 34, 93–100 (2012). https://doi.org/10.1007/s10840-011-9648-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-011-9648-z