Abstract
Purpose
The aim of this study was to explore the predictive role of microRNAs (miRNAs) from maternal serum exosomes in early recurrent pregnancy loss (RPL) and the related mechanism in early pregnancy.
Methods
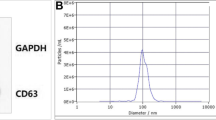
Maternal serum was collected from pregnant women with RPL history or women with ongoing pregnancy (OP); serum exosomes were extracted and identified. Differentially expressed (DE) miRNAs in exosomes were screened by RNA sequencing and further validated by qRT-PCR. Next, the predictive value of exosomal miRNA and the clinical indicators for subsequent miscarriage in RPL patients were evaluated. Additionally, we verified the regulatory relationship between miR-185-5p and vascular endothelial growth factor (VEGF) in decidual natural killer (dNK) cells by overloading or inhibiting the exosomal miR-185-5p level in trophoblast cells.
Results
The miRNA sequencing revealed 43 DE miRNAs between OP and RPL patients. The five most significant DE miRNAs (miR-22-3p, miR-185-5p, miR-335-3p, miR-362-5p, and miR-378a-3p) were selected for identification, and miR-185-5p was increased in RPL patients. The area under curve (AUC) of the receiver operating characteristic was 0.925 when using miR-185-5p as a biomarker for subsequent miscarriage in RPL patients. In addition, miR-185-5p in exosomes secreted from HTR-8 cells reduces VEGF expression of dNK cells.
Conclusions
The current study, for the first time, successfully constructed the correlation between maternal circulating exosomal miR-185-5p expression pattern and RPL, which may be involved in the pathogenesis of RPL by downregulating the VEGFA of dNK cells and perturbing angiogenesis at the maternal–fetal interface.







Similar content being viewed by others
Data availability
The data included in this article are available from the corresponding author upon reasonable request.
References
Quenby S, et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. 2021;397(10285):1658–67.
Bender AR, et al. ESHRE guideline: recurrent pregnancy loss. Hum Reprod Open. 2018;2018(2):hoy004.
Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2020;113(3):533–5.
Schieve LA, et al. Spontaneous abortion among pregnancies conceived using assisted reproductive technology in the United States. Obstet Gynecol. 2003;101(5 Pt 1):959–67.
Wang A, Kort J, Westphal L. Miscarriage history association with euploid embryo transfer outcomes. Reprod Biomed Online. 2019;39(4):617–23.
Bu Z, et al. Factors related to early spontaneous miscarriage during IVF/ICSI treatment: an analysis of 21,485 clinical pregnancies. Reprod Biomed Online. 2020;40(2):201–6.
Branch DW, Gibson M, Silver RM. Clinical practice recurrent miscarriage. N Engl J Med. 2010;363(18):1740–7.
Coomarasamy A, et al. Recurrent miscarriage: evidence to accelerate action. Lancet. 2021;397(10285):1675–82.
Liu XY, et al. Higher chromosomal abnormality rate in blastocysts from young patients with idiopathic recurrent pregnancy loss. Fertil Steril. 2020;113(4):853–64.
Magnus MC, et al. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019;364:l869.
Lv Y, et al. miRNA and target gene expression in menstrual endometria and early pregnancy decidua. Eur J Obstet Gynecol Reprod Biol. 2016;197:27–30.
Jairajpuri DS, et al. Differentially expressed circulating microRNAs associated with idiopathic recurrent pregnancy loss. Gene. 2021;768:145334.
Wang X, et al. Evidence that miR-133a causes recurrent spontaneous abortion by reducing HLA-G expression. Reprod Biomed Online. 2012;25(4):415–24.
Qin W, et al. Potential role of circulating microRNAs as a biomarker for unexplained recurrent spontaneous abortion. Fertil Steril. 2016;105(5):1247–1254.e3.
Zhou Y, et al. Circulating microRNA profile as a potential predictive biomarker for early diagnosis of spontaneous abortion in patients with subclinical hypothyroidism. Front Endocrinol (Lausanne). 2018;9:128.
Vashukova ES, et al. High-throughput sequencing of circulating microRNAs in plasma and serum during pregnancy progression. Life (Basel). 2021;11(10):1055.
Cui S, et al. Circulating microRNAs from serum exosomes as potential biomarkers in patients with spontaneous abortion. Am J Transl Res. 2021;13(5):4197–210.
Pegtel DM, Gould SJ. Exosomes. Annu Rev Biochem. 2019;88:487–514.
Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478):6977.
Jiang L, et al. Exosomes in pathogenesis, diagnosis, and treatment of Alzheimer's disease. Med Sci Monit. 2019;25:3329–35.
Lu M, et al. The exosome-derived biomarker in atherosclerosis and its clinical application. J Cardiovasc Transl Res. 2019;12(1):68–74.
Zhu T, et al. The role of exosome in autoimmune connective tissue disease. Ann Med. 2019;51(2):101–8.
Matsubara K, et al. Pathophysiology of preeclampsia: the role of exosomes. Int J Mol Sci. 2021;22(5):2572.
Ye Z, et al. Plasma exosomal miRNAs associated with metabolism as early predictor of gestational diabetes mellitus. Diabetes. 2022;71(11):2272–83.
Li Y, et al. Identification of endogenous controls for analyzing serum exosomal miRNA in patients with hepatitis B or hepatocellular carcinoma. Dis Markers. 2015;2015:893594.
Guo W, et al. Decreased human leukocyte antigen-G expression by miR-133a contributes to impairment of proinvasion and proangiogenesis functions of decidual NK cells. Front Immunol. 2017;8:741.
Zhang X, Wei H. Role of decidual natural killer cells in human pregnancy and related pregnancy complications. Front Immunol. 2021;12:728291.
Ma Y, et al. MicroRNA-30c promotes natural killer cell cytotoxicity via up-regulating the expression level of NKG2D. Life Sci. 2016;151:174–81.
Ostling H, et al. Placental expression of microRNAs in infants born small for gestational age. Placenta. 2019;81:46–53.
Luo L, et al. MicroRNA-378a-5p promotes trophoblast cell survival, migration and invasion by targeting nodal. J Cell Sci. 2012;125(Pt 13):3124–32.
Sun Y, et al. Identification of differentially expressed miRNAs in serum extracellular vesicles (EVs) of Kazakh sheep at early pregnancy. Reprod Domest Anim. 2021;56(5):713–24.
Yadava SM, et al. miR-15b-5p promotes expression of proinflammatory cytokines in human placenta by inhibiting Apelin signaling pathway. Placenta. 2021;104:8–15.
Tang XW, Qin QX. miR-335-5p induces insulin resistance and pancreatic islet beta-cell secretion in gestational diabetes mellitus mice through VASH1-mediated TGF-beta signaling pathway. J Cell Physiol. 2019;234(5):6654–66.
Zhang C, Zhao D. MicroRNA-362-5p promotes the proliferation and inhibits apoptosis of trophoblast cells via targeting glutathione-disulfide reductase. Bioengineered. 2021;12(1):2410–9.
DeVilbiss EA, et al. Prediction of pregnancy loss by early first trimester ultrasound characteristics. Am J Obstet Gynecol. 2020;223(2):242.e1–242.e22.
Puget C, et al. Serial hCG and progesterone levels to predict early pregnancy outcomes in pregnancies of uncertain viability: a prospective study. Eur J Obstet Gynecol Reprod Biol. 2018;220:100–5.
Wang Y, et al. The clinical value of 3D ultrasonic measurement of the ratio of gestational sac volume to embryo volume in IoT-based prediction of pregnancy outcome. J Healthc Eng. 2021;2021:6421025.
Wei J, Zhao Y. MiR-185-5p protects against angiogenesis in polycystic ovary syndrome by targeting VEGFA. Front Pharmacol. 2020;11:1030.
Zhang Z, et al. The possible role of visceral fat in early pregnancy as a predictor of gestational diabetes mellitus by regulating adipose-derived exosomes miRNA-148 family: protocol for a nested case-control study in a cohort study. BMC Pregnancy Childbirth. 2021;21(1):262.
Huang Q, et al. Androgen receptor increases hematogenous metastasis yet decreases lymphatic metastasis of renal cell carcinoma. Nat Commun. 2017;8(1):918.
Griebel CP, et al. Management of spontaneous abortion. Am Fam Physician. 2005;72(7):1243–50.
Pillai RN, et al. Role of serum biomarkers in the prediction of outcome in women with threatened miscarriage: a systematic review and diagnostic accuracy meta-analysis. Hum Reprod Update. 2016;22(2):228–39.
Xu N, et al. Integrative analysis of circulating microRNAs and the placental transcriptome in recurrent pregnancy loss. Front Physiol. 2022;13:893744.
Bruno V, et al. Low molecular weight heparin-induced miRNA changes in peripheral blood mononuclear cells in pregnancies with unexplained recurrent pregnancy loss. J Reprod Immunol. 2022;151:103502.
Sebastiani G, et al. Circulating microRNAs and diabetes mellitus: a novel tool for disease prediction, diagnosis, and staging? J Endocrinol Invest. 2017;40(6):591–610.
Yuan Q, et al. MiR-185-5p ameliorates endoplasmic reticulum stress and renal fibrosis by downregulation of ATF6. Lab Invest. 2020;100(11):1436–46.
Gerbaud P, Tasken K, Pidoux G. Spatiotemporal regulation of cAMP signaling controls the human trophoblast fusion. Front Pharmacol. 2015;6:202.
Saha B, et al. TEAD4 ensures postimplantation development by promoting trophoblast self-renewal: an implication in early human pregnancy loss. Proc Natl Acad Sci U S A. 2020;117(30):17864–75.
Ferrara N, et al. Molecular and biological properties of the vascular endothelial growth factor family of proteins. Endocr Rev. 1992;13(1):18–32.
Liu Y, et al. Decidual natural killer cells: a good nanny at the maternal-fetal interface during early pregnancy. Front Immunol. 2021;12:663660.
Zhou G, et al. miR-219a suppresses human trophoblast cell invasion and proliferation by targeting vascular endothelial growth factor receptor 2 (VEGFR2). J Assist Reprod Genet. 2021;38(2):461–70.
Dubinsky V, et al. Role of regulatory and angiogenic cytokines in invasion of trophoblastic cells. Am J Reprod Immunol. 2010;63(3):193–9.
Cabar FR, et al. Vascular endothelial growth factor and beta-human chorionic gonadotropin are associated with trophoblastic invasion into the tubal wall in ectopic pregnancy. Fertil Steril. 2010;94(5):1595–600.
An HJ, et al. 3'-UTR polymorphisms in the vascular endothelial growth factor gene (VEGF) contribute to susceptibility to recurrent pregnancy loss (RPL). Int J Mol Sci. 2019;20(13):3319. https://doi.org/10.3390/ijms20133319.
Huang Z, et al. Placental angiogenesis in mammals: a review of the regulatory effects of signaling pathways and functional nutrients. Adv Nutr. 2021;12(6):2415–34.
Mayhew TM, Charnock-Jones DS, Kaufmann P. Aspects of human fetoplacental vasculogenesis and angiogenesis III. Changes in complicated pregnancies. Placenta. 2004;25(2-3):127–39.
Andraweera PH, Dekker GA, Roberts CT. The vascular endothelial growth factor family in adverse pregnancy outcomes. Hum Reprod Update. 2012;18(4):436–57.
Bagheri A, et al. Association of angiogenic cytokines (VEGF-A and VEGF-C) and clinical characteristic in women with unexplained recurrent miscarriage. Bratisl Lek Listy. 2017;118(5):258–64.
Scarpellini F, et al. Immunohistochemical study on the expression of G-CSF, G-CSFR, VEGF, VEGFR-1, Foxp3 in first trimester trophoblast of recurrent pregnancy loss in pregnancies treated with G-CSF and controls. Int J Mol Sci. 2019;21(1):285.
Ying X, et al. Exosomes released from decidual macrophages deliver miR-153-3p, which inhibits trophoblastic biological behavior in unexplained recurrent spontaneous abortion. Int Immunopharmacol. 2020;88:106981.
Acknowledgements
We are indebted to the individuals who participated in the research. We are very grateful to nurse Rong Zhang for helping to coordinate the collection of samples and data. We thank the National Natural Science Foundation of China for supporting this project. We thank John Myers at AJE for editing the language of this manuscript.
Funding
This research was supported by a grant from the National Natural Science Foundation of China (No. 81871182).
Author information
Authors and Affiliations
Contributions
Y.J.X., Z.F., J.D., S.Q.C., and X.H.W. contributed to conceiving and designing the study and to data acquisition. W.L.Z. and L.H. contributed to sample acquisition and article revision. Y.J.X., J.Q.M., J.Z. Z.F., J.D., and X.H.W contributed to data analysis, data interpretation, and drafting and revising the article. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Tangdu Hospital Ethics Committee (code no. TDLL2018-03-39). Informed consents were acquired from all subjects involved in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1:
Supplemental Table 1. List of the miRNA/mRNA PCR primers for real-time PCR
ESM 2:
Supplemental Fig. 1 Identification of isolated dNK cells. Flow cytometry was performed to identify the density of CD3-CD56+ dNK cells before and after sorting. Supplemental Fig. 2 Principal component analysis (PCA) plot of DE miRNAs between 4 RPL patients and 5 OP women. Supplemental Fig. 3 Comparison of the expression levels of miR-185-5p among the RPL group and the OP subgroups. (a) Relative expression of miR-185-5p in the OP1 group (patients who maintained a pregnancy without RPL history) and OP2 group (patients who maintained a pregnancy with RPL history). (b) Relative expression of miR-185-5p in the OP1 group and RPL group. (c) Relative expression of miR-185-5p in the OP2 group and RPL group, **** P<0.0001, Mann–Whitney U test was used.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiong, Y., Fang, Z., Dong, J. et al. Maternal circulating exosomal miR-185-5p levels as a predictive biomarker in patients with recurrent pregnancy loss. J Assist Reprod Genet 40, 553–566 (2023). https://doi.org/10.1007/s10815-023-02733-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02733-y