Abstract
Purpose
To investigate if breast cancer stage and grade affect fertility preservation outcomes.
Methods
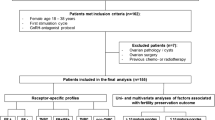
We performed a retrospective cohort study that included premenopausal women with breast cancer undergoing fertility preservation diagnosed between January 2011 and January 2019. The primary outcome measure was the number of mature oocytes (MII) per antral follicle count (AFC). Secondary outcome measures included total oocytes retrieved, total mature oocytes retrieved, and greater than 10 mature oocytes preserved. Univariate and multivariate models were used to assess the association of low vs. high stage (low stage I–II and high stage III–IV) and grade I vs. grade II/III with each outcome, with adjustment for confounders.
Results
A total of 267 premenopausal breast cancer patients undergoing fertility preservation were included in our study, with the majority presenting with low stage (N = 215, 80.5%), grade II/III (N = 235, 88.1%) disease. Baseline AFC, total gonadotropin dose, days of stimulation, and follicles \(\ge\) 13 mm on the day of trigger did not differ by stage or grade. After adjusting for age, BMI, and baseline AFC, we found that the mean MII per AFC did not differ by stage (1.0 vs. 1.1, P = 0.3) or grade (1.0 vs. 1.0, P = 0.92). Similarly, total oocytes retrieved, total MII retrieved, and percentage of patients who were able to preserve greater than 10 MII did not differ by breast cancer stage or grade (all P > 0.2).
Conclusion
Breast cancer grade and stage do not impact ovarian stimulation or fertility preservation outcome.
Similar content being viewed by others
Data availability
We are unable to provide our data due to its identified nature.
Code Availability
Code may be made available upon request.
References
Society. AC. Breast Cancer Facts & Figures 2019–2020. In: Society AC, ed., 2019.
Ethics Committee of the American Society for Reproductive Medicine. Electronic address Aao. Fertility preservation and reproduction in patients facing gonadotoxic therapies: an Ethics Committee opinion. Fertil Steril. 2018;110:380–65.
Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36:1994–2001.
Anazodo A, Ataman-Millhouse L, Jayasinghe Y, Woodruff TK. Oncofertility-an emerging discipline rather than a special consideration. Pediatr Blood Cancer. 2018;65:e27297.
Letourneau JM, Sinha N, Wald K, Harris E, Quinn M, Imbar T, et al. Random start ovarian stimulation for fertility preservation appears unlikely to delay initiation of neoadjuvant chemotherapy for breast cancer. Hum Reprod. 2017;32:2123–9.
Letourneau JM, Wald K, Sinha N, Juarez-Hernandez F, Harris E, Cedars MI, et al. Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 43 months after fertility-preservation consultation. Cancer. 2020;126:487–95.
Moravek MB, Confino R, Smith KN, Kazer RR, Klock SC, Lawson AK, et al. Long-term outcomes in cancer patients who did or did not pursue fertility preservation. Fertil Steril. 2018;109:349–55.
Baker JA, Buck GM, Vena JE, Moysich KB. Fertility patterns prior to testicular cancer diagnosis. Cancer Causes Control. 2005;16:295–9.
Hendry WF, Stedronska J, Jones CR, Blackmore CA, Barrett A, Peckham MJ. Semen analysis in testicular cancer and Hodgkin’s disease: pre- and post-treatment findings and implications for cryopreservation. Br J Urol. 1983;55:769–73.
Spermon JR, Ramos L, Wetzels AM, Sweep CG, Braat DD, Kiemeney LA, et al. Sperm integrity pre- and post-chemotherapy in men with testicular germ cell cancer. Hum Reprod. 2006;21:1781–6.
Viviani S, Ragni G, Santoro A, Perotti L, Caccamo E, Negretti E, et al. Testicular dysfunction in Hodgkin’s disease before and after treatment. Eur J Cancer. 1991;27:1389–92.
Whitehead E, Shalet SM, Blackledge G, Todd I, Crowther D, Beardwell CG. The effects of Hodgkin’s disease and combination chemotherapy on gonadal function in the adult male. Cancer. 1982;49:418–22.
Turan V, Quinn MM, Dayioglu N, Rosen MP, Oktay K. The impact of malignancy on response to ovarian stimulation for fertility preservation: a meta-analysis. Fertil Steril. 2018;110:1347–55.
Volodarsky-Perel A, Cohen Y, Arab S, Son WY, Suarthana E, Dahan MH, et al. Effects of cancer stage and grade on fertility preservation outcome and ovarian stimulation response. Hum Reprod. 2019;34:530–8.
Volodarsky-Perel A, Cai E, Tulandi T, Son WY, Suarthana E, Buckett W. Influence of stage and grade of breast cancer on fertility preservation outcome in reproductive-aged women. Reprod Biomed Online. 2020;40:215–22.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 2002;41:154–61.
Chung K, Irani J, Knee G, Efymow B, Blasco L, Patrizio P. Sperm cryopreservation for male patients with cancer: an epidemiological analysis at the University of Pennsylvania. Eur J Obstet Gynecol Reprod Biol. 2004;113(Suppl 1):S7-11.
Tal R, Botchan A, Hauser R, Yogev L, Paz G, Yavetz H. Follow-up of sperm concentration and motility in patients with lymphoma. Hum Reprod. 2000;15:1985–8.
Padron OF, Sharma RK, Thomas AJ Jr, Agarwal A. Effects of cancer on spermatozoa quality after cryopreservation: a 12-year experience. Fertil Steril. 1997;67:326–31.
Rueffer U, Breuer K, Josting A, Lathan B, Sieber M, Manzke O, et al. Male gonadal dysfunction in patients with Hodgkin’s disease prior to treatment. Ann Oncol. 2001;12:1307–11.
Rubin H. Systemic effects of cancer: role of multiple proteases and their toxic peptide products. Med Sci Monit. 2005;11:RA221-8.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Almog B, Azem F, Gordon D, Pauzner D, Amit A, Barkan G, et al. Effects of cancer on ovarian response in controlled ovarian stimulation for fertility preservation. Fertil Steril. 2012;98:957–60.
Alvarez RM, Ramanathan P. Fertility preservation in female oncology patients: the influence of the type of cancer on ovarian stimulation response. Hum Reprod. 2018;33:2051–9.
Das M, Shehata F, Moria A, Holzer H, Son WY, Tulandi T. Ovarian reserve, response to gonadotropins, and oocyte maturity in women with malignancy. Fertil Steril. 2011;96:122–5.
Quinn MM, Cakmak H, Letourneau JM, Cedars MI, Rosen MP. Response to ovarian stimulation is not impacted by a breast cancer diagnosis. Hum Reprod. 2017;32:568–74.
Acknowledgements
We would like to make a special thanks to our nurses and care coordinators who provided patient education and fertility preservation coordination.
Funding
This study was supported by departmental research funding within the University of California, San Francisco Department of Obstetrics, Gynecology, and Reproductive Sciences.
Author information
Authors and Affiliations
Contributions
K.W, A.W., M.K.A., and J.R.M.’s roles included data collection, data analysis, and manuscript writing; J.M.L.’s roles included study design and data collection; E.M.L., M.I.C., and M.R.’s roles included study design and manuscript writing. All author roles meet the following criteria: (1) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be published, and (4) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of California, San Francisco (UCSF) Committee on Human Research and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
As part of the consent process, all participants gave written consent to use de-identified information for research purposes and publications.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kaitlyn Wald and Ange Wang are joint first authors.
Rights and permissions
About this article
Cite this article
Wald, K., Wang, A., Abel, M.K. et al. Breast cancer grade and stage do not affect fertility preservation outcomes. J Assist Reprod Genet 39, 1155–1161 (2022). https://doi.org/10.1007/s10815-022-02473-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02473-5