Abstract
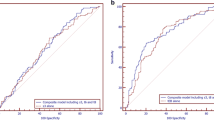
In order to maintain pregnancy rates following single embryo transfer, optimisation of embryo culture and selection is vital. Time-lapse monitoring (TLM) has the potential to play a crucial role by providing sequential images of embryo development and minimal disturbance. Therefore, in this study morphometric assessment of blastocyst area and maximum width was performed in order to evaluate if these parameters are associated with pregnancy outcomes in IVF/ICSI cycles. This is a retrospective study of 664 patients who had elective single blastocyst transfer (eSBT). The EmbryoScope drawing tools were used to measure specific variables such as the maximum blastocyst width and blastocyst area. Our results show that women who were pregnant had significantly (P < 0.01) larger blastocyst width [median (range) μm] 184 (125–239) versus non-pregnant, 160 (120–230)] and area [median (range) μm2] 26099 (12101–45,280) versus non-pregnant women, 22,251 (10992–37,931)]. A univariate logistic regression performed showed that blastocyst width [(OR = 1.026, 95% CI = (1.019, 1.033)] was significant (P < 0.01) and for every μm increase of blastocyst width, the odds of clinical pregnancy increase by 2.6%. A univariate logistic regression performed showed that blastocyst area [(OR = 1.00008, 95% CI = (1.00006, 1.00011)] was significant with P < 0.01. For every μm2 increase of blastocyst area, our data showed the odds of clinical pregnancy increase by 0.008%. Hosmer-Lemeshow tests of calibrations were performed to verify calibration. Although our findings show a clear correlation between blastocyst dimensions and the clinical pregnancy rate, further studies are necessary to confirm these observations.






Similar content being viewed by others
References
Steptoe P, Edwards RG. Birth after the reimplantation of a human embryo. Lancet. 1978;2:366.
Wang SX. The past, present and future of embryo selection in in vitro fertilization: Frontiers in Reproductive Conference Yale J Biol Med. 2011;84:487–90.
De Geyter C, Calhaz-Jorge C, Kupka MS, Wyns C, Mocanu E, Motrenko T, et al. Goossens V; European IVF-monitoring consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). ART in Europe, 2014: results generated from European registries by ESHRE: the European IVF- monitoring consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod. 2018 Sep 1;33(9):1586–601.
Johnston J, Gusmano MK, Patrizio P. Preterm births, multiples, and fertility treatment: recommendations for changes to policy and clinical practices. Fertil Steril. 2014;102:36–9.
Pinborg A, Loft A, Nyobe AA. Neonatal outcome in a Danish national cohort of 8602 children born after in vitro fertilizationorintracystoplasmic sperm injection: theroleoftwinpregnancy. Acta Obstet Gynecol Scand. 2004;83(11):1071–8.
Braude P, Bolton V, Moore S. Human gene expression first occurs between the four- and eight-cell stages of preimplantation development. Nature. 1988;332:459–61.
Aparicio-Ruiz B, Basile N, Perez Albala S, Bronet F, Remohi J, Meseguer M. Automatic time-lapse instrument is superior to singlepoint morphology observation for selecting viable embryos: retrospective study in oocyte donation. FertilSteril 2016 Nov 106 (6): 1379, 1385.e10.
Yoon HG, Yoon SH, Son WY, Im KS, Lim JH. High implantation and pregnancy rates with transfer of human hatching day 6 blastocysts. Fertil Steril. 2001;75:832–3.
Chimote NM, Chimote NN, Nath NM, Mehta BN. Transfer of spontaneously hatching or hatched blastocyst yields better pregnancy rates than expanded blastocyst transfer. J Hum Reprod Sci. 2013 Jul;6(3):183–8.
Balaban B, Urman B, Sertac A, Alatas C, Aksoy S, Mercan R. Blastocyst quality affects the success of blastocyst-stage embryo transfer. Fertil Steril. 2000;74:282–7.
Hartshorne GM, Elder K, Crow J, Dyson H, Edwards RG. The influence of in-vitro development upon post-thaw survival and implantation of cryopreserved human blastocysts. Hum Reprod. 1991;6:136–41.
Ahlstrom A, Westin C, Reismer E, Wikland M, Hardarson T. Trophectoderm morphology: an important parameter for predicting live birth after single blastocyst transfer. Hum Reprod. 2011;26:3289–96.
Van den Abbeel E, Balaban B, Ziebe S, Lundin K, Cuesta MJG, Liein BM, et al. Association between blastocyst morphology and outcome of single-blastocyst transfer. Reprod BioMed Online. 2013;27:353–61.
Subira J, Craig J, Turner K, Bevan A, Ohuma E, McVeigh E, et al. Grade of the inner cell mass, but not trophectoderm, predicts live birth in fresh blastocyst single transfers. Hum Fertil (Camb). 2016 Dec;19(4):254–61 Epub 2016 Sep 14.
Hill MJ, Richter KS, Heitmann RJ, Graham JR, Tucker MJ, DeCherney AH, et al. Trophectoderm grade predicts outcomes of single-blastocyst transfers. Fertil Steril. 2013 Apr;99(5):1283–9.
Alikani M, Calderon G, Tomkin G, Garrisi J, Kokot M, Cohen J. Cleavage anomalies in early human embryos and survival after prolonged culture in-vitro. Hum Reprod. 2000;15:2634–43.
Sciorio R, Thong JK, Pickering SJ. Comparison of the development of human embryos cultured in either an EmbryoScope or benchtop incubator. J Assist Reprod Genet. 2018 Mar;35(3):515–22.
Cutting R, Morroll D, Roberts SA, Pickering S J, Rutherford A; BFS and ACE 2008. Elective single embryo transfer: guidelines for practice British fertility society and Association of Clinical Embryologists. Hum Fertil (Camb) 2008; Sep 11(3):131–146.
Gardner DK, Schoolcraft WB. Culture and transfer of human blastocysts. Curr Opin Obstet Gynecol Jun 1999; 11(3):307–11 Review.
Almagor M, Harir Y, Fieldust S, Or Y, Shoham Z. Ratio between inner cell mass diameter and blastocyst diameter is correlated with successful pregnancy outcomes of single blastocyst transfers. Fertil Steril. 2016 Nov;106(6):1386–91.
Huang TTF, Chinn K, Kosasa T, Ahn HJ, Kessel B. Morphokinetics of human blastocyst expansion in vitro. Reprod BioMed Online. 2016;33:659–67.
van Montfoort A. P, Dumoulin JC, Land JA, Coonen E, Derhaag JG, Evers JL. Elective single embryo transfer (eSET) policy in the first three IVF/ICSI treatment cycles. Hum Reprod 2005;20: 433–436.
Chamayou S, Patrizio P, Storaci G, Tomaselli V, Alecci C, Ragolia C, et al. The use of morphokinetic parameters to select all embryos with full capacity to implant. J Assist Reprod Genet. 2013 Jun;30(5):703–10.
Lemmen JG, Agerholm I, Ziebe S. Kinetic markers of human embryo quality using time-lapse recordings of IVF/ICSI-fertilized oocytes. Reprod BioMed Online. 2008;17:385–91.
Meseguer M, Herrero J, Tejera A, Hilligsoe KM, Ramsing NB and Remohi J. The use of morphokinetics as a predictor of embryo implantation. Hum Reprod 2011-b Oct; 26(10): 2658–71.
Campbell A, Fishel S, Bowman N, Duffy S, Sedler M, Hickman CF. Modelling a risk classification of aneuploidy in human embryos using non-invasive morphokinetics. Reprod BioMed Online. 2013;26(5):477–85.
Payne D, Flaherty SP, Barry MF, Matthews CD. Preliminary observations on polar body extrusion and pronuclear formation in human oocytes using time-lapse video cinematography. Hum Reprod. 1997;12:532–41.
Basile N, Nogales Mdel C, Bronet F, Florensa M, Riqueiros M, Rodrigo L, et al. Increasing the probability of selecting chromosomally normal embryos by time-lapse morphokinetics analysis. Fertil Steril. 2014;101:699–704.
Cruz M, Garrido N, Herrero J, Perez-Cano I, Munoz M, Meseguer M. Timing of cell division in human cleavage-stage embryos is linked with blastocyst formation and quality. Reprod Biomed Online 2012, Oct; 25(4): 371-81Epub 2012 Jul 7.
Marcos J, Perez-Albala S, Mifsud A, Molla M, Landeras J, Meseguer M. Collapse of blastocysts is strongly related to lower implantation success: a time-lapse study. Hum Reprod. 2015;30:2501–8.
Sciorio R, Herrer Saura R, Thong KJ, Esbert Algam M, Pickering SJ, Meseguer M. Blastocyst collapse as an embryo marker of low implantation potential: a time-lapse multicentre study. Zygote. 2020 Jan;13:1–9.
Sciorio R, Thong KJ, Pickering SJ. Spontaneous blastocyst collapse as an embryo marker of low pregnancy outcome: a time-lapse study. JBRA Assist Reprod. 2020 Jan 30;24(1):34–40.
Niimura S. Time-lapse videomicrographic analyses of contractions in mouse blastocysts. J Reprod Dev. 2003 Dec;49(6):413–23.
Della Ragione T, Verheyen G, Papanikolaou EG, Van Landuyt L, Devroey P, Van Steirteghem A. Developmental stage on day-5 and fragmentation rate on day-3 can influence the implantation potential of top-quality blastocysts in IVF cycles with single embryo transfer. Reprod Biol Endocrinol. 2007 Jan 26;5:2.
Kresowik JD, Sparks AE, Van Voorhis BJ. Clinical factors associated with live birth after single embryo transfer. Fertil Steril. 2012;98:1152–6.
Thompson SM, Onwubalili N, Brown K, Jindal SK, McGovern PG. Blastocyst expansion score and trophectoderm morphology strongly predict successful clinical pregnancy and live birth following elective single embryo blastocyst transfer (eSET): a national study. J Assist Reprod Genet. 2013;30:1577–81.
Kato K, Ueno S, Yabuuchi A, Uchiyama K, Okuno T, Kobayashi T, et al. Women's age and embryo developmental speed accurately predict clinical pregnancy after single vitrified-warmed blastocyst transfer. Reprod BioMed Online. 2014 Oct;29(4):411–6.
Richter KS, Harris DC, Daneshmand ST, Shapiro BS. Quantitative grading of a human blastocyst: optimal inner cell mass size and shape. Fertil Steril. 2001 Dec;76(6):1157–67.
Chen X, Zhang J, Wu X, Cao S, Zhou L, Wang Y, et al. Trophectoderm morphology predicts outcomes of pregnancy in vitrified-warmed singleblastocyst transfer cycle in a Chinese population. J Assist Reprod Genet. 2014;31:1475–81.
Honnma H, Baba T, Sasaki M, Hashiba Y, Ohno H, Fukunaga T, et al. Trophectoderm morphology significantly affects the rates of ongoing pregnancy and miscarriage in frozen-thawed single-blastocyst transfer cycle in vitro fertilization. Fertil Steril. 2012;98:361–7.
Goto S, Kadowaki T, Tanaka S, Hashimoto H, Kokeguchi S, Shiotani M. Prediction of pregnancy rate by blastocyst morphological score and age, based on 1488 single frozen-thawed blastocyst transfer cycles. Fertil Steril. 2011;95:948–52.
Du QY, Wang EY, Huang Y, Guo XY, Xiong YJ, Yu YP, et al. Blastocoele expansion degree predicts live birth after single blastocyst transfer for fresh and vitrified/warmed single blastocyst transfer cycles. Fertil Steril. 2016;105:910–9.
Tasampalas M, Gridelet V, Berndt S, Foidart JM, Geenen V, Perrier d’Hauterive S. Human chorionic gonadotropin: a hormone with immunological and angiogenic properties. J Reprod Immunol. 2010;85:93–8.
Alfarawati S, Fragouli E, Colls P, Stevens J, Gutierrez-Mateo C, Schoolcraft WB, et al. The relationship between blastocyst morphology, chromosomal abnormality, and embryo gender. Fertil Steril. 2011;95:520–4.
Parks JC, McCallie BR, Janesch AM, Schoolcraft WB, Katz-Jaffe MG. Blastocyst gene expression correlates with implantation potential. Fertil Steril. 2011;95:1367–72.
Bendus AEB, Mayer JF, Shipley SK, Catherino WH. Interobserver and intraobserver variation in day 3 embryo grading. Fertil Steril. 2006;86:1608–15.
Hnida C, Engenheiro E, Ziebe S. Computer-controlled, multilevel, morphometric analysis of blastomere size as biomarker of fragmentation and multinuclearity in human embryos. Hum Reprod. 2004;19:288–93.
Santos Filho E, Noble JA, Wells D. A review on automatic analysis of human embryo microscope images. Open Biomed Eng J. 2010;4:170–7.
Paternot G, Debrock S, De Neubourg D, D’Hooghe TM, Spiessens C. Semi-automated morphometric analysis of human embryos can reveal correlations between total embryo volume and clinical pregnancy. Hum Reprod. 2013;28(3):627–33.
Huang TTF, Huang DH, Ahn HJ, Arnett C, Huang CTF. Early blastocyst expansion in euploid and aneuploid human embryos: evidence for a non-invasive and quantitative marker for embryo selection. Reprod BioMed Online. 2019 Jul;39(1):27–39.
Funding
Project support was provided by the Edinburgh Assisted Conception Programme, EFREC, Royal Infirmary of Edinburgh, 51 Little France Crescent, Old Dalkeith Road, Edinburgh, Scotland, EH16 4SA, UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments. The Local Ethics Committee did not require an ethical approval for this retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sciorio, R., Thong, D., Thong, K.J. et al. Clinical pregnancy is significantly associated with the blastocyst width and area: a time-lapse study. J Assist Reprod Genet 38, 847–855 (2021). https://doi.org/10.1007/s10815-021-02071-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02071-x