Abstract
Purpose
To determine if pre-implantation genetic testing (PGT) shifts the sex ratio (SER), the ratio of male to female births in a population normalized to 100 and typically stable at 105, following in vitro fertilization (IVF).
Methods
Data from 2014 to 2016 was requested from the Society for Assisted Reproductive Technologies (SART) database including fresh and frozen transfer cycles. Women with a singleton live birth following a fresh or frozen autologous embryo transfer of a PGT blastocyst, non-PGT blastocyst, or non-PGT cleavage stage embryo were included. The SER between groups was compared using chi-square tests. Modified Poisson regression modeled the relative risk (RR) of having a male compared to a female among PGT blastocyst transfers versus non-PGT cleavage and blastocyst transfers adjusting for age, BMI, smoking status, race, parity, number of oocytes retrieved, and clinic region.
Results
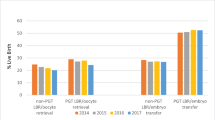
The SER was 110 among PGT blastocyst offspring, 107 among non-PGT blastocyst offspring (p = 0.005), and 99 among non-PGT cleavage offspring (p < 0.001). The risk of having a male infant was 2% higher among PGT blastocyst transfers compared to non-PGT blastocyst transfers (RR 1.02; 95% CI: 1.01, 1.04). The risk was 5% higher among PGT blastocyst transfers compared to non-PGT cleavage transfers (RR 1.05; 95% CI: 1.02, 1.07). The association between PGT and infant gender did not significantly differ by region (p = 0.57) or parity (p = 0.59).
Conclusion
Utilizing PGT shifts the SER in the IVF population from the standard of 105 to 110, increasing the probability of a male offspring.
Similar content being viewed by others
References
Age and Sex Composition: 2010. United States Census Bureau. 2011, p 1–16.
Mathews TJ, Hamilton BE. Trend Analysis of the Sex Ratio at Birth in the United States. CDC. Natl Vital Stat Rep. 2005;53(20):1–18.
Hesketh TXZ. Abnormal sex ratios in human populations: causes and consequences. PNAS. 2006;103:13271–5.
Bureau, U.S.C. Gender. 2000;2000:1–8.
Zhu WX, Lu L, Hesketh T. China's excess males, sex selective abortion, and one child policy: analysis of data from 2005 national intercensus survey. BMJ. 2009;338:b1211.
Dyson T. Causes and consequences of skewed sex ratios. Annu Rev Sociol. 2012;38(1):443–61.
CDC. Assisted Reproductive Technology (ART). National Center for Chronic Disease Prevention and Health Promotion. 2019. Available from: https://www.cdc.gov/art/artdata/index.html.
Assisted Reproductive Technology National Summary Report. National Center for Chronic Disease Prevention and Health Promotion division of reproductive health. 2015
Zhang WY, von Versen-Höynck F, Kapphahn KI, Fleischmann RR, Zhao Q, Baker VL. Maternal and neonatal outcomes associated with trophectoderm biopsy. Fertil Steril. 2019;112(2):283–90 e2.
Ethics Committee of the American Society for Reproductive Medicine. Disclosure of sex when incidentally revealed as part of preimplantation genetic testing (PGT): an Ethics Committee opinion. Fertil Steril. 2018:625–7.
Ethics Committee of the American Society for Reproductive, M. Use of reproductive technology for sex selection for nonmedical reasons. Fertil Steril. 2015;103(6):1418–22.
Capelouto SM, Archer SR, Morris JR, Kawwass JF, Hipp HS. Sex selection for non-medical indications: a survey of current pre-implantation genetic screening practices among U.S. ART clinics. J Assist Reprod Genet. 2018;35(3):409–16.
Baruch S, Kaufman D, Hudson KL. Genetic testing of embryos: practices and perspectives of US in vitro fertilization clinics. Fertil Steril. 2008;89(5):1053–8.
Eaton JL, Hacker MR, Barrett CB, Thornton KL, Penzias AS. Influence of embryo sex on development to the blastocyst stage and euploidy. Fertil Steril. 2011;95(3):936–9.
Csokmay JM, Hill MJ, Cioppettini FV, Miller KA, Scott RT Jr, Frattarelli JL. Live birth sex ratios are not influenced by blastocyst-stage embryo transfer. Fertil Steril. 2009;92(3):913–7.
Weston G, Osianlis T, Catt J, Vollenhoven B. Blastocyst transfer does not cause a sex-ratio imbalance. Fertil Steril. 2009;92(4):1302–5.
Narvaez JL, Chang J, Boulet SL, Davies MJ, Kissin DM. Trends and correlates of the sex distribution among U.S. assisted reproductive technology births. Fertil Steril. 2019;112(2):305–14.
Hentemann MA, Briskemyr S, Bertheussen K. Blastocyst transfer and gender: IVF versus ICSI. J Assist Reprod Genet. 26:433–6.
Chang HJ, Lee JR, Jee BC, Suh CS, Kim SH. Impact of blastocyst transfer on offspring sex ratio and the monozygotic twinning rate: a systematic review and meta-analysis. Fertil Steril. 2009;91(6):2381–90.
Luna M, Duke M, Copperman A, Grunfeld L, Sandler B, Barritt J. Blastocyst embryo transfer is associated with a sex-ratio imbalance in favor of male offspring. Fertil Steril. 2007;87(3):519–23.
Foundation, R.C.T.R.A.l.a.e.f.s.c.R. and V. for Statistical Computing, Austria. URL https://www.R-project.org/.
Lin PY, Huang FJ, Kung FT, Wang LJ, Chang SY, Lan KC. Comparison of the offspring sex ratio between fresh and vitrification-thawed blastocyst transfer. Fertil Steril. 2009;92(5):1764–6.
Roberts A, Shah MS, Schmidt R. Sex differences in euploid rates between day 5 and day 6 blastocyst expansion in IVF/PGT-A cycles. Fertil Steril. 2018;110(4):e72.
Zhang X, Wang Y, Zhao N, Liu P, Huang J. Variations in chromosomal aneuploidy rates in IVF blastocysts and early spontaneous abortion chorionic villi. J Assist Reprod Genet. 2020.
Ray P, Conaghan J, Winston R. Handyside A. Increased number of cells and metabolic activity in male human preimplantation embryos following in vitro fertilization. J Reprod Fertil. 1995;104:165–71.
Boulet SL, Mehta A, Kissin DM, Warner L, Kawwass JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015;313(3):255–63.
Acknowledgments
The authors would like to thank the Society for Assisted Reproductive Technology for providing the data to complete this analysis.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by all of the authors, and data collection and analysis were performed by Tracy Truong and Carl Pieper. The first draft of the manuscript was written by Kathryn Shaia, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors’ declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shaia, K., Truong, T., Pieper, C. et al. Pre-implantation genetic testing alters the sex ratio: an analysis of 91,805 embryo transfer cycles. J Assist Reprod Genet 37, 1117–1122 (2020). https://doi.org/10.1007/s10815-020-01746-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01746-1