Abstract
Purpose
In vitro fertilization (IVF) infants have lower birthweights than their peers, predisposing them to long-term health consequences. Blastocyst transfer (BT), at day 5–6 post-fertilization, is increasing in usage, partially due to improved pregnancy outcomes over cleavage-stage transfer (CT, day 2–3). Data to date, however, have been inconclusive regarding BT’s effects on birthweight.
Methods
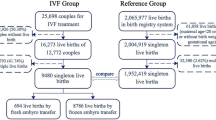
Participants included all US autologous, single-gestation, fresh embryo transfer cycles initiated from 2007 to 2014 that resulted in a term infant (N = 124,154) from the National Assisted Reproductive Technology Surveillance System. Generalized linear models including obstetric history, maternal demographics, and infant sex and gestational age were used to compare birthweight outcomes for infants born following BT (N = 67,169) with infants born following CT (N = 56,985) and to test for an interaction between transfer stage and single embryo transfer (SET).
Results
Infants born following BT were 6 g larger than those born following CT (p = 0.04), but rates of macrosomia (RR 1.00, 95% CI 0.96–1.04) and low birthweight (LBW, RR 1.00, 95% CI 0.93–1.06) were not different between the groups. The interaction between SET and transfer stage was significant (p = 0.02). Among SET infants, BT was associated with 19.26 g increased birthweight compared to CT (p = 0.008).
Conclusions
The increase in birthweights identified following BT is unlikely to be clinically relevant, as there were no differences in rates of macrosomia or LBW. These findings are clinically reassuring and indicate that the increasing use of BT is unlikely to further decrease the on average lower birthweights seen in IVF infants compared to their naturally conceived peers.

Similar content being viewed by others
References
Centers for Disease Control and Prevention; American Society for Reproductive Medicine; Society for Assisted Reproductive Technology. 2014 assisted reproductive technology fertility clinic success rates report [Internet] US Dept Heal Hum Serv 2016 Available from:https://www.cdc.gov/art/pdf/2014-report/art-2014-national-summary-report.pdf.
BeydounHA, SicignanoN, BeydounMA, MatsonDO, BoccaS, StadtmauerL, et al. A cross-sectional evaluation of the first cohort of young adults conceived by in vitro fertilization in the United States. Fertil. Steril. [Internet]. Elsevier Ltd; 2010;94:2043–9. Available from: 101016/jfertnstert2009.12.023.
BouletSL, KirbyRS, ReefhuisJ, ZhangY, SunderamS, CohenB, et al.Assisted reproductive technology and birth defects among liveborn infants in Florida, Massachusetts, and Michigan, 2000–2010. JAMA Pediatr. [Internet]. 2016;e154934. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27043648.
Albertini DF, Evers JLH, Geraedts JPM, Gianaroli L, Sharpe R, Sinclair KD, et al. Birth defects and congenital health risks in children conceived through assisted reproduction technology (ART): a meeting report. J Assist Reprod Genet. [Internet]. 2014;31:947–58. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4130939/.
Owen CM, Segars JH. Imprinting disorders and assisted reproductive technology. Semin Reprod Med [Internet]. Am Soc Reprod Med. 2009;27:417–28. https://doi.org/10.1016/j.fertnstert.2009.01.002.
Barnhart KT. How do we explain the association between assisted reproductive technologies and perinatal morbidity? Fertil Steril [Internet] Am Soci Reprod Med. 2015;103:896–7. Available from. https://doi.org/10.1016/j.fertnstert.2015.01.020.
HayashiM, NakaiA, SatohS, MatsudaY. Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril. [Internet]. Elsevier Inc.; 2012;98:922–8. Available from: https://doi.org/10.1016/j.fertnstert.2012.05.049.
Palomba S, Homburg R, Santagni S, La Sala GB, Orvieto R. Risk of adverse pregnancy and perinatal outcomes after high technology infertility treatment: a comprehensive systematic review. Reprod Biol Endocrinol [Internet] Reprod Biol Endocrinol. 2016;14:76. https://doi.org/10.1186/s12958-016-0211-8.
D’AngeloD V., WhiteheadN, HelmsK, BarfieldW, AhluwaliaIB. Birth outcomes of intended pregnancies among women who used assisted reproductive technology, ovulation stimulation, or no treatment. Fertil Steril [Internet] Elsevier Ltd; 2011;96:314–320.e2. Available from: https://doi.org/10.1016/j.fertnstert.2011.05.073, 2011.
Hille ETM, Weisglas-Kuperus N, van Goudoever JB, Jacobusse GW, Ens-Dokkum MH, de Groot L, et al. Functional outcomes and participation in young adulthood for very preterm and very low birth weight infants: the Dutch Project on Preterm and Small for Gestational Age Infants at 19 years of age. Pediatrics [Internet]. 2007;120:e587–95. Available from:http://pediatrics.aappublications.org/cgi/doi/10.1542/peds.2006-2407.
Barker DJP. The developmental origins of adult disease. Eur J Epidemiol [Internet]. 2003;18:733–6. Available from:http://www.jstor.org/stable/3582917.
Yliharsila H, Kajantie E, Osmond C, Forsen T, Barker DJ, Eriksson JG. Birth size, adult body composition and muscle strength in later life. Int J Obes (Lond). [Internet]. 2007;31:1392–9. Available from:https://www.nature.com/ijo/journal/v31/n9/full/0803612a.html.
Glujovsky D, Blake D, Bardach A, Farquhar C. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Libr. 2013;
Kaartinen NM, Kananen KM, Rodriguez-Wallberg KA, Tomas CM, Huhtala HS, Tinkanen HI. Male gender explains increased birthweight in children born after transfer of blastocysts. Hum Reprod [Internet]. 2015;30:2312–20. Available from:. https://doi.org/10.1093/humrep/dev174.
Zhu J, Lin S, Li M, Chen L, Lian Y, Liu P, et al. Effect of in vitro culture period on birthweight of singleton newborns. Hum Reprod [Internet]. 2014;29:448–54. Available from:. https://doi.org/10.1093/humrep/det460.
Kalra SK, Ratcliffe SJ, Barnhart KT, Coutifaris C. Extended embryo culture and an increased risk of preterm delivery. Obstet Gynecol [Internet]. 2012;120:69–75. Available from:https://insights.ovid.com/pubmed?pmid=22914393.
ErnstadEG, BerghC, KhatibiA, KällénKBM, WestlanderG, NilssonS, et al. Neonatal and maternal outcome after blastocyst transfer: a population-based registry study. Am J Obstet Gynecol [Internet]. Elsevier Inc.; 2016;214:378.e1–378.e10. Available from:http://www.sciencedirect.com/science/article/pii/S0002937815025880.
BarskyM, St. Marie P, Rahil T, Markenson GR, Sites CK. Are perinatal outcomes affected by blastocyst vitrification and warming? Am. J. Obstet. Gynecol. [Internet]. Elsevier Inc.; 2016;215:603.e1-603.e5. Available from: https://doi.org/10.1016/j.ajog.2016.06.002, 2016.
ChambersGM, ChughtaiAA, FarquharCM, WangYA. Risk of preterm birth after blastocyst embryo transfer: a large population study using contemporary registry data from Australia and New Zealand. Fertil. Steril. [Internet]. Elsevier Inc.; 2015;104:997–1003. Available from: https://doi.org/10.1016/j.fertnstert.2015.07.1130, 2015.
De Vos A, Janssens R, VandeVelde H, Haentjens P, Bonduelle M, Tournaye H, et al. The type of culture medium and the duration of in vitro culture do not influence birthweight of ART singletons. Hum Reprod [Internet]. 2015;30:20–7. Available from:https://academic.oup.com/humrep/article-lookup/doi/10.1093/humrep/deu286.
Dar S, Librach CL, Gunby J, Bissonnette F, Cowan L. Increased risk of preterm birth in singleton pregnancies after blastocyst versus Day 3 embryo transfer: Canadian ART Register (CARTR) analysis. Hum Reprod [Internet]. 2013;28:924–8. https://doi.org/10.1093/humrep/des448.
Maxwell SM, Melzer-Ross K, McCulloh DH, Grifo JA. A comparison of pregnancy outcomes between day 3 and day 5/6 embryo transfers: does day of embryo transfer really make a difference? J Assist Reprod Genet. [Internet]. 2015;32:249–54. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4354181/.
Mäkinen S, Söderström-Anttila V, Vainio J, Suikkari AM, Tuuri T. Does long in vitro culture promote large for gestational age babies? Hum Reprod [Internet]. 2013;28:828–34. Available from:https://academic.oup.com/humrep/article/28/3/828/936104/Does-long-in-vitro-culture-promote-large-for.
Linder N, Lahat Y, Kogan A, Fridman E, Kouadio F, Melamed N, et al. Macrosomic newborns of non-diabetic mothers: anthropometric measurements and neonatal complications. Arch Dis childhood.Fetal neonatal Ed. [Internet]. 2014;99:353–8. Available from:http://fn.bmj.com/content/99/5/F353.long.
WennerströmCE, SimonsenJ, Melbye M. Long-term survival of individuals born small and large for gestational age. PLoS One [Internet]. 2015 [cited 2017May 9];10:e0138594. Available from:https://doi.org/10.1371/journal.pone.0138594&type=printable.
ChiavaroliV, GianniniC, D’AdamoE, de Giorgis T, ChiarelliF, Mohn A. Insulin resistance and oxidative stress in children born small and large for gestational age. Pediatrics [Internet]. 2009 [cited 2017May 9];124:695–702. Available from:http://pediatrics.aappublications.org/content/pediatrics/124/2/695.full.pdf.
RichterKS, AndersonM, OsbornBH. Selection for faster development does not bias sex ratios resulting from blastocyst embryo transfer. Reprod. Biomed. Online [Internet]. Reproductive Healthcare Ltd, Duck End Farm, Dry Drayton, Cambridge CB23 8DB, UK; 2006;12:460–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16740219.
Ray PF, Conaghan J, Winston RM, Handyside AH. Increased number of cells and metabolic activity in male human preimplantation embryos following in vitro fertilization. J Reprod Fertil [Internet]. 1995;104:165–71. Available from:http://www.reproduction-online.org/content/104/1/165.long.
Talge NM, Mudd LM, Sikorskii A, Basso O. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics [Internet]. 2014;133:844–53. Available from:http://pediatrics.aappublications.org/content/133/5/844.abstract.
MaaloufWE, MinchevaMN, CampbellBK, HardyICW. Effects of assisted reproductive technologies on human sex ratio at birth. Fertil. Steril. [Internet]. Elsevier Inc.; 2014;101:1321–5. Available from: https://doi.org/10.1016/j.fertnstert.2014.01.041, 2014.
Dean JH, Chapman MG, Sullivan EA. The effect on human sex ratio at birth by assisted reproductive technology (ART) procedures—an assessment of babies born following single embryo transfers, Australia and New Zealand, 2002–2006. BJOG An Int J Obstet Gynaecol. [Internet]. 2010;117:1628–34. Available from:. https://doi.org/10.1111/j.1471-0528.2010.02731.x/epdf.
ChangHJ, LeeJR, JeeBC, SuhCS, KimSH. Impact of blastocyst transfer on offspring sex ratio and the monozygotic twinning rate: a systematic review and meta-analysis. Fertil. Steril. [Internet]. Elsevier Ltd; 2009;91:2381–90. Available from: https://doi.org/10.1016/j.fertnstert.2008.03.066, 2009.
Luna M, Duke M, Copperman A, Grunfeld L, Sandler B, Barritt J. Blastocyst embryo transfer is associated with a sex-ratio imbalance in favor of male offspring. Fertil Steril [Internet]. 2007;87:519–23. Available from:http://www.sciencedirect.com/science/article/pii/S0015028206040143?via%3Dihub.
WestonG, OsianlisT, CattJ, VollenhovenB. Blastocyst transfer does not cause a sex-ratio imbalance. Fertil. Steril. [Internet]. Elsevier Ltd; 2009;92:1302–5. Available from: https://doi.org/10.1016/j.fertnstert.2008.07.1784, 2009.
Milki AA, Jun SH, Hinckley MD, Westphal LW, Giudice LC, Behr B. Comparison of the sex ratio with blastocyst transfer and cleavage stage transfer. J Assist Reprod Genet [Internet]. 2003;20:323–6. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3455273/.
Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, et al. Assisted reproductive technology surveillance—United States, 2013. MMWR Surveill Summ [Internet]. 2015;64:1–28. Available from:https://www.cdc.gov/mmwr/preview/mmwrhtml/ss6411a1.htm.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol [Internet]. 2008;61:344–9. Available from:http://www.strobe-statement.org/index.php?id=strobe-publications.
DickeyRP, XiongX, KlempelMC, PridjianG. Singleton birth weight by gestational age following in vitro fertilization in the United States. Am J Obstet Gynecol [Internet]. Elsevier Inc.; 2016;214:101.e1–101.e13. Available from:http://www.sciencedirect.com/science/article/pii/S0002937815008595.
Hamilton BE, Martin JA, Osterman MJ, Curtin SC, Mathews T. National Vital Statistics Reports Births: final data for 2014. Statistics (Ber). [Internet]. 2015;64:1–104. Available from:https://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_12.pdf.
Kalra, S.K., Ratcliffe, S.J., Barnhart, K.T., Coutifaris C. abstract: Day 3 vs blastocyst embryo transfer: extended embryo culture is associated with an increased risk of preterm delivery. Fertil Steril [Internet]. Elsevier Ltd; 2010;94:S242. Available from: https://doi.org/10.1016/j.fertnstert.2010.07.938&atitle=Day+3+vs+blast.
De Sutter P, Delbaere I, Gerris J, Verstraelen H, Goetgeluk S, Van der Elst J, et al. Birthweight of singletons after assisted reproduction is higher after single- than after double-embryo transfer. Hum Reprod [Internet]. 2006;21:2633–7. Available from:. https://doi.org/10.1093/humrep/del247.
Kalu E, Thum MY, Abdalla H. Reducing multiple pregnancy in assisted reproduction technology: towards a policy of single blastocyst transfer in younger women. BJOG An Int J Obstet Gynaecol [Internet]. 2008;115:1143–50. https://doi.org/10.1111/j.1471-0528.2008.01764.x/epdf.
Palomba S, De Wilde MA, Falbo A, Koster MPH, La Sala GB, Fauser BCJM. Pregnancy complications in women with polycystic ovary syndrome. Hum Reprod Update. 2015;21:575–92.
MaheshwariA, RajaEA, BhattacharyaS. Obstetric and perinatal outcomes after either fresh or thawed frozen embryo transfer: an analysis of 112,432 singleton pregnancies recorded in the Human Fertilisation and Embryology Authority anonymized dataset. Fertil. Steril. [Internet]. Elsevier Inc.; 2016;106:1703–8. Available from: https://doi.org/10.1016/j.fertnstert.2016.08.047, 2016.
Sunkara SK, Antonisamy B, Selliah HY, Kamath MS. Pre-term birth and low birth weight following preimplantation genetic diagnosis: analysis of 88 010 singleton live births following PGD and IVF cycles. Hum Reprod. 2017;32:432–8.
HassonJ, LimoniD, MalcovM, FrumkinT, AmirH, ShavitT, et al.Obstetric and neonatal outcomes of pregnancies conceived after preimplantation genetic diagnosis: cohort study and meta-analysis. Reprod Biomed Online [Internet] Elsevier Ltd; 2017; Available from: 101016/jrbmo2017.05.003.
Funding
This work is funded by grants from the National Institutes of Health (NIH-NIMH R01MH094609, NIH-NIEHS R01ES022223, P01 ES022832) and the Environmental Protection Agency (EPA RD8354420). Funding sources had no involvement in data collection, data analysis, or generation of the manuscript.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This project was approved by the Institutional Review Board at the CDC.
Conflict of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Supplemental Table 1
(PDF 88kb)
Supplemental Table 2
(PDF 87kb)
Rights and permissions
About this article
Cite this article
Litzky, J.F., Boulet, S.L., Esfandiari, N. et al. Birthweight in infants conceived through in vitro fertilization following blastocyst or cleavage-stage embryo transfer: a national registry study. J Assist Reprod Genet 35, 1027–1037 (2018). https://doi.org/10.1007/s10815-018-1168-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1168-7