Abstract
Purpose
Many practices are moving away from cleavage-stage transfer in favor of blastocyst transfer. The purpose of this study is to evaluate how the overall live birth rate for fresh IVF cycles may increase by optimizing the day of transfer for each patient.
Methods
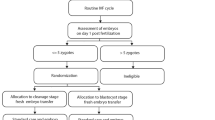
This is a retrospective cohort study of 1225 first fresh autologous IVF cycles performed between May 2012 and November 2013. Stepwise logistic regression was used to determine characteristics associated with live birth following cleavage-stage versus blastocyst transfer. The optimal transfer day (i.e., the day that maximized the odds of live birth) was determined for each patient, and the actual live birth rate was compared with the projected rate had each patient undergone transfer on her optimal day.
Results
With transfer on the optimal day for each patient, the overall birth rate would have increased from its actual value of 34.8 % to a projected 43.0 %, a 24 % increase. The majority of this increase (21 %) was due to optimization of patients who underwent cleavage-stage transfer but had a higher projected birth rate from blastocyst transfer. These patients were older (37.8 versus 36.0 years, p < 0.01) and had more follicles ≥18 mm than patients who should have remained with a cleavage-stage transfer.
Conclusions
A model can be built enabling patient-specific identification of optimal transfer day; within this discovery cohort, such optimization was estimated to increase live birth following a fresh transfer by 24 %. This study suggests blastocyst transfer should be more widely offered; however, there remain patients for whom a cleavage-stage transfer may yield better outcomes.


Similar content being viewed by others
References
Glujovsky D, Blake D, Farquhar C, Bardach A. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2012;7:CD002118.
Marsh CA, Farr SL, Chang J, Kissin DM, Grainger DA, Posner SF, et al. Trends and factors associated with the day 5 embryo transfer, assisted reproductive technology surveillance, USA, 2001–2009. Hum Reprod. 2012;27:2325–31.
Jones GM, Trounson AO. Blastocyst stage transfer: pitfalls and benefits. The benefits of extended culture. Hum Reprod. 1999;14:1405–8.
Thomas MR, Sparks AE, Ryan GL, Van Voorhis BJ. Clinical predictors of human blastocyst formation and pregnancy after extended embryo culture and transfer. Fertil Steril. 2010;94:543–8.
Gardner DK, Vella P, Lane M, Wagley L, Schlenker T, Schoolcraft WB. Culture and transfer of human blastocysts increases implantation rates and reduces the need for multiple embryo transfers. Fertil Steril. 1998;69:84–8.
Mangalraj AM, Muthukumar K, Aleyamma T, Kamath MS, George K. Blastocyst stage transfer vs cleavage stage embryo transfer. J Hum Reprod Sci. 2009;2:23–6.
Papanikolaou EG, Kolibianakis EM, Tournaye H, Venetis CA, Fatemi H, Tarlatzis B, et al. Live birth rates after transfer of equal number of blastocysts or cleavage-stage embryos in IVF. A systematic review and meta-analysis. Hum Reprod. 2008;23:91–9.
Papanikolaou EG, Camus M, Kolibianakis EM, Van Landuyt L, Van Steirteghem A, Devroey P. In vitro fertilization with single blastocyst-stage versus single cleavage-stage embryos. N Engl J Med. 2006;354:1139–46.
Zech NH, Lejeune B, Puissant F, Vanderzwalmen S, Zech H, Vanderzwalmen P. Prospective evaluation of the optimal time for selecting a single embryo for transfer: day 3 versus day 5. Fertil Steril. 2007;88:244–6.
Rienzi L, Ubaldi F, Iacobelli M, Ferrero S, Minasi MG, Martinez F, et al. Day 3 embryo transfer with combined evaluation at the pronuclear and cleavage stages compares favourably with day 5 blastocyst transfer. Hum Reprod. 2002;17:1852–5.
Van der Auwera I, Debrock S, Spiessens C, Afschrift H, Bakelants E, Meuleman C, et al. A prospective randomized study: day 2 versus day 5 embryo transfer. Hum Reprod. 2002;17:1507–12.
Frattarelli JL, Leondires MP, McKeeby JL, Miller BT, Segars JH. Blastocyst transfer decreases multiple pregnancy rates in in vitro fertilization cycles: a randomized controlled trial. Fertil Steril. 2003;79:228–30.
Maheshwari A, Kalampokas T, Davidson J, Bhattacharya S. Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of blastocyst-stage versus cleavage-stage embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril. 2013;100:1615–21.e1–10.
Dar S, Lazer T, Shah PS, Librach CL. Neonatal outcomes among singleton births after blastocyst versus cleavage stage embryo transfer: a systematic review and meta-analysis. Hum Reprod Update. 2014;20:439–48.
Racowsky C, Combelles CMH, Nureddin A, Pan Y, Finn A, Miles L, et al. Day 3 and day 5 morphological predictors of embryo viability. Reprod Biomed Online. 2003;6:323–31.
Ceyhan ST, Jackson K V., Racowsky C. Biennial Review of Infertility Voorhis BJ, Schlegel PN, Racowsky C, Carrell DT, editors. S. Temel Ceyhan, Katharine V. Jackson, Catherine Racowsky. Sel. Most Competent Embryo. Totowa, NJ: Humana Press; 2009.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocysts. Towar. Reprod. Certain. Fertil. Genet. Beyond 1999 Plenary Proc. 11th World Congr. 1999. p. 378–88.
Rubio C, Rodrigo L, Mercader A, Mateu E, Buendía P, Pehlivan T, et al. Impact of chromosomal abnormalities on preimplantation embryo development. Prenat Diagn. 2007;27:748–56.
Zakharova EE, Zaletova VV, Krivokharchenko AS. Biopsy of human morula-stage embryos: outcome of 215 IVF/ICSI cycles with PGS. PLoS One. 2014;9:e106433.
Fanchin R, Ayoubi JM, Righini C, Olivennes F, Schönauer LM, Frydman R. Uterine contractility decreases at the time of blastocyst transfers. Hum Reprod. 2001;16:1115–9.
Gardner DK, Balaban B. Choosing between day 3 and day 5 embryo transfers. Clin Obstet Gynecol. 2006;49:85–92.
Biggers JD, Racowsky C. The development of fertilized human ova to the blastocyst stage in KSOM(AA) medium: is a two-step protocol necessary? Reprod. Biomed. Online;5:133–40.
Machtinger R, Racowsky C. Culture systems: single step. Methods Mol Biol. 2012;912:199–209.
Quinn P. Culture systems: sequential. Methods Mol Biol. 2012;912:211–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
LF is supported by T32HD060454 in reproductive, perinatal, and pediatric epidemiology from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Health.
Ethical approval
For this type of study, formal consent is not required.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Capsule By optimizing the day of embryo transfer for individual patients, overall live birth rate can be significantly increased.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 37 kb)
Rights and permissions
About this article
Cite this article
Goldman, R.H., Kaser, D.J., Missmer, S.A. et al. Building a model to increase live birth rate through patient-specific optimization of embryo transfer day. J Assist Reprod Genet 33, 1525–1532 (2016). https://doi.org/10.1007/s10815-016-0803-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0803-4